Research - (2020) Volume 8, Issue 6
Vitamin-D Deficiency and its Effect on Bone Profile: An Observational Study
Mohammed A Noureddin1*, Abdullah S Al-Dosary2, Fahad M AlGhamdi2, Ziyad M Ali Alshehri2, Tariq F Bindaaj2 and Saud S Alanazi2
*Correspondence: Mohammed A Noureddin, Department of Medicine, Division of Nephrology, College of Medicine, Prince Sattam Bin Abdulaziz University, Kingdom of Saudi Arabia, Email:
Abstract
Background: 25- hydroxyvitamin D (25-OHD) is an essential vitamin to be regulated in the body. It has a key function in the regulation of calcium, phosphate, and magnesium homeostasis. This study aims to explore the association between vitamin-D and bone profile.
Study design: Observational study.
Methods: Laboratory results including vitamin D and bone profile had been collected from 197 patients who visited the university hospital between the period of January 2013-March 2018 aging more than or equal to 10 years. Data were analyzed through SPSS.
Results: 76.4% of normal PTH patients had decreased vitamin D levels, 80.5% of optimal ALP subjects were vitamin D deficit, 80.1% of people with normal calcium had low vitamin D and 80% of normal serum phosphate patients had lower than normal vitamin D levels.
Conclusion: No significant association was found between vitamin D deficit patients and other bone profiles.
Keywords
Vitamin D, Calcium, Phosphate, PTH, Bone profile
Introduction
Bone is an organ that is characterized by rigidity and hardness and has a highly specialized framework that supports the body and had the power for regeneration and repair [1]. It has the ability for remodeling throughout life and the purpose of this process is to repair micro-fraction by the consequence of the coupled reaction of (osteoclast) which is boneresorbing cells and (osteoblast) which is boneforming cells [2]. Bone also serves as a reservoir for minerals like calcium and phosphorus homeostasis and a reservoir of growth factors and cytokines [1]. For maintaining bone health, some interactions between deferent factors affect bone mineral density (BMD) like genetic, endocrine, mechanical, and nutritional factors [3]. The strategy for optimizing the peak of bone mass throughout childhood is one of the best strategies to prevent age-related osteoporosis [4].
Vitamin D plays an important role in the nurturement of bones, and a deficiency of the vitamin may end up in metabolic bone diseases leading to rickets in children or osteomalacia in adults [5]. Both vitamin D and calcium nutrients have strongly been linked with optimal building for bone mass [4]. Vitamin D is the “sunshine vitamin” which is a fat-soluble hormone that plays a principal part in calcium hemostasis and mineralization of bones [6]. Vitamin D is also distinct in its physiologic and metabolic functions [6]. Humans rely on Both endogenic syntheses which is activation through exposure to ultraviolet light that accounts for about 90% and exogenic sources (diet, primarily fortified food) [4,6]. More lately, the levels of vitamin D have been associated with bone health in adults, vitamin D level is regulated from the interaction of various factors, including intestinal absorption, renal function, serum calcium level, and parathyroid hormone (PTH) [5]. The traditional role of vitamin D includes the transformation to its active metabolite (1,25- dihydroxyvitamin D) in response to PTH, when the level of calcium is low, which results in enhancement of calcium absorption from the gut, renal calcium reabsorption, and bone resorption [4]. Sub-par serum vitamin D leads to increased serum PTH, which in turn raises bone remodeling and results in elevated risk of fractures [4]. The parathyroid gland increases its secretion of (PTH) causing hyperparathyroidism which leads to hypercalcemia [7]. Secondary hyperparathyroidism, which is a result of decreased levels of calcium, is related to poor vitamin D status [8,9]. It has been established that the association between serum 25-hydroxyvitamin D (25-OHD) and serum PTH is an inverse relationship [8]. The rise in serum PTH related to the level of 15-OHD is still a matter of debate [10–12]. Reports indicate that not all who have poor vitamin D status have a high level of PTH [13].
Aims and objectives
The main aim is to reach a conclusion regarding the relationship between vitamin D and bone profile. This first can be done by gaining access to the 197 patient’s files to record the necessary results then running those through a statistical program to reach our conclusion.
Methodology
This observational study was conducted on 197 patients who visited the university hospital from January of 2013 until March of 2018, aging more than or equal to 10 years. The sample size was calculated through SurveyMonkey.com. Laboratory results regarding 25- hydroxyvitamin D (25-OHD) and bone profile “PTH, ALP, Calcium and, Phosphate” were selected for correlation to a low than normal vitamin D levels. The data were analyzed through a statistical package for the social sciences (SPSS). Inclusion criteria: all patients aging more than or equal to 10 years who visited the university hospital and had the appropriate laboratory results. Exclusion criteria: patients aging less than 10 years.
Results
In this study, we aimed to study the correlation between vitamin D and bone profile levels. This study was conducted on 197 patients who attended the university hospital from January of 2013 until March of 2018. Table 1 displays full demographics.
| Demographics |
| Sample size: 197 |
| Gender: 48.7% males and 51.3% females |
| Mean age: 40.9 years |
| Nationality: 56.9% are Saudis and 43.1% are non-Saudis |
| Mean weight is 80.8 KG |
Table 1: Study demographics.
Vitamin D and Gender: 48.7% [96] were men and 51.3% [101] were women. Cumulatively, we found that 79.2% [156] of our patients had some sort of sub-par vitamin D levels “whether severe deficiency 14.7% [23], deficiency 54.5% [85] or insufficiency 30.8% [48].” and 18.2% [37] had optimal levels, whereas 2% [4] had toxic levels. Table 2 summarizes the correlation between Vitamin D levels and gender.
| Count | Gender | Total | ||
| 1 | 2 | |||
| Vit D | 1 | 9 (9.3%) | 14 (13.9%) | 23 (11.7%) |
| 2 | 39 (40.6%) | 46 (45.5%) | 85 (43.1%) | |
| 3 | 27 (28.1%) | 21 (20.8%) | 48 (24.4%) | |
| 4 | 20 (21%) | 17 (16.8%) | 37 (18.8%) | |
| 5 | 1 (1%) | 3 (3%) | 4 (2%) | |
| Total | 96 (48.7%) | 101 (51.3%) | 197 (100%) | |
Table 2: Vit D * gender crosstabulation.
Vitamin D and PTH: Most of the patients had normal levels of PTH 73.1% [144]. 25.4% [50] had higher levels, and 1.5% [3] had lower levels. Out of the 144 normal PTH patients, we found that 76.4% [110] had decreased vitamin D levels, 21.5% [31] had normal vitamin D, and 2.1% [3] had toxic levels. Table 3 and Graph 1 summarize all the findings regarding vitamin D and PTH relation.
| Vit D | Total | |||||||
| 1 | 2 | 3 | 4 | 5 | ||||
| PTH | 1 | Count | 0 | 2 | 1 | 0 | 0 | 3 |
| % within PTH | 0.00% | 66.70% | 33.30% | 0.00% | 0.00% | 100.00% | ||
| % within Vit D | 0.00% | 2.40% | 2.10% | 0.00% | 0.00% | 1.50% | ||
| 2 | Count | 11 | 60 | 39 | 31 | 3 | 144 | |
| % within PTH | 7.60% | 41.70% | 27.10% | 21.50% | 2.10% | 100.00% | ||
| % within Vit D | 47.80% | 70.60% | 81.30% | 83.80% | 75.00% | 73.10% | ||
| 3 | Count | 12 | 23 | 8 | 6 | 1 | 50 | |
| % within PTH | 24.00% | 46.00% | 16.00% | 12.00% | 2.00% | 100.00% | ||
| % within Vit D | 52.20% | 27.10% | 16.70% | 16.20% | 25.00% | 25.40% | ||
| Total | Count | 23 | 85 | 48 | 37 | 4 | 197 | |
| % within PTH | 11.70% | 43.10% | 24.40% | 18.80% | 2.00% | 100.00% | ||
| % within Vit D | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% | ||
Vit D: 1=Severe deficiency [<10 ng/ml], 2=Deficiency [<20 ng/ml], 3=Insufficiency [<30 ng/ml], 4=Optimal [30-60 ng/ml] and 5=Toxic [>60 ng/ml]
Table 3: PTH * Vit D Crosstabulation.
Vitamin D and ALP: An overwhelming majority of the patients had a normal ALP, 91.4% [180], and the others had high ALP, 8.6% [17]. A large percent, 80.5% [145] of the 180 patients had sub-levels of vitamin D. Full summary is included in Table 4.
| Vit D | Total | |||||||
| 1 | 2 | 3 | 4 | 5 | ||||
| ALP | 2 | Count | 20 | 80 | 45 | 33 | 2 | 180 |
| % within ALP | 11.10% | 44.40% | 25.00% | 18.30% | 1.10% | 100.00% | ||
| % within Vit D | 87.00% | 94.10% | 93.80% | 89.20% | 50.00% | 91.40% | ||
| 3 | Count | 3 | 5 | 3 | 4 | 2 | 17 | |
| % within ALP | 17.60% | 29.40% | 17.60% | 23.50% | 11.80% | 100.00% | ||
| % within Vit D | 13.00% | 5.90% | 6.30% | 10.80% | 50.00% | 8.60% | ||
| Total | Count | 23 | 85 | 48 | 37 | 4 | 197 | |
| % within ALP | 11.70% | 43.10% | 24.40% | 18.80% | 2.00% | 100.00% | ||
| % within Vit D | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% | ||
Vit D: 1=Severe deficiency [<10 ng/ml], 2=Deficiency [<20 ng/ml], 3=Insufficiency [<30 ng/ml], 4= optimal [30-60 ng/ml] and 5=Toxic [>60 ng/ml]
Table 4: ALP * Vit D Crosstabulation.
Vitamin D and Calcium: An immense number of patients had normal calcium levels, 94.4% [186], whereas 2.5% [5] had lower levels and 3% [6] were hypercalcemic. Of those with normal levels, 80.1% [149] had low vitamin D; moreover, 17.7% [33] were found to have normal vitamin D and 2.2% [4] had hypervitaminosis D. Table 5 summarizes all the findings.
| Vit D | Total | |||||||
| 1 | 2 | 3 | 4 | 5 | ||||
| Calcium | 1 | Count | 1 | 2 | 0 | 2 | 0 | 5 |
| % within Calcium | 20.00% | 40.00% | 0.00% | 40.00% | 0.00% | 100.00% | ||
| % within Vit D | 4.30% | 2.40% | 0.00% | 5.40% | 0.00% | 2.50% | ||
| 2 | Count | 21 | 83 | 45 | 33 | 4 | 186 | |
| % within Calcium | 11.30% | 44.60% | 24.20% | 17.70% | 2.20% | 100.00% | ||
| % within Vit D | 91.30% | 97.60% | 93.80% | 89.20% | 100.00% | 94.40% | ||
| 3 | Count | 1 | 0 | 3 | 2 | 0 | 6 | |
| % within Calcium | 16.70% | 0.00% | 50.00% | 33.30% | 0.00% | 100.00% | ||
| % within Vit D | 4.30% | 0.00% | 6.30% | 5.40% | 0.00% | 3.00% | ||
| Total | Count | 23 | 85 | 48 | 37 | 4 | 197 | |
| % within Calcium | 11.70% | 43.10% | 24.40% | 18.80% | 2.00% | 100.00% | ||
| % within Vit D | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% | ||
Table 5: Calcium* Vit D crosstabulation.
Vitamin D and Phosphate: A large portion had optimal phosphate levels 89.3% [175], and 3.6% [7] had decreased levels. 7.1% [14] had higher markers. 80% [140] of normal serum phosphate had lower than normal vitamin D levels. Refer to Table 6 for the full summary (Figure 1).
| Vit D | Total | |||||||
| 1 | 2 | 3 | 4 | 5 | ||||
| Phosphate | 1 | Count | 2 | 1 | 2 | 2 | 0 | 7 |
| % within Phosphate | 28.60% | 14.30% | 28.60% | 28.60% | 0.00% | 100.00% | ||
| % within Vit D | 8.70% | 1.20% | 4.30% | 5.40% | 0.00% | 3.60% | ||
| 2 | Count | 20 | 80 | 40 | 31 | 4 | 175 | |
| % within Phosphate | 11.40% | 45.70% | 22.90% | 17.70% | 2.30% | 100.00% | ||
| % within Vit D | 87.00% | 94.10% | 85.10% | 83.80% | 100.00% | 89.30% | ||
| 3 | Count | 1 | 4 | 5 | 4 | 0 | 14 | |
| % within Phosphate | 7.10% | 28.60% | 35.70% | 28.60% | 0.00% | 100.00% | ||
| % within Vit D | 4.30% | 4.70% | 10.60% | 10.80% | 0.00% | 7.10% | ||
| Total | Count | 23 | 85 | 47 | 37 | 4 | 196 | |
| % within Phosphate | 11.70% | 43.40% | 24.00% | 18.90% | 2.00% | 100.00% | ||
| % within Vit D | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% | ||
Vit D: 1=Severe deficiency [<10 ng/ml], 2=Deficiency [<20 ng/ml], 3=Insufficiency [<30 ng/ml], 4=Optimal [30-60 ng/ml] and 5=Toxic [>60 ng/ml]
Table 6: Phosphate * Vit D crosstabulation.
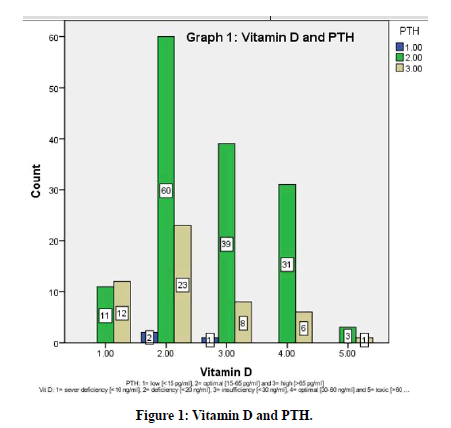
Figure 1. Vitamin D and PTH.
Discussion
In this study, the main aim was to investigate the relationship between vitamin D reduction below the normal and bone profile levels. Serum PTH had not shown a significant alteration to decreased 25-hydroxyvitamin D (25-OHD). Previous studies disagreed and displayed a negative association [14,15]. However, one study had described similar results [16]. Serum ALP, calcium, and phosphate were not increased nor decreased in relation to vitamin D deficient subjects. This same association was reached in past studies [17,18].
Conclusion
There was no significant change in serum PTH, ALP, calcium, and phosphate in relation to low vitamin D levels. In our study bone profile markers were unreliable to aid in the diagnosis of vitamin D deficiency, so clinicians must maintain high suspicion and treat vitamin D deficiency promptly to avoid unwanted complications.
Limitations
The nature of our study is an important limitation as is the time limit of approximately 16 weeks.
Acknowledgments
This publication was supported by the Deanship of scientific research at Prince Sattam bin Abdul Aziz University, Al-Kharj, Saudi Arabia.
Author Contributions
The research was conducted by the author and mentioned students.
Funding
This research received no external funding.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Written consent was obtained from the university hospital administration. Additional informed consent was obtained from all individual participants for whom identifying information is included in this manuscript.
Ethical Approval for Human
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards (ethical approval number: (REC-HSD-004-2020).
Data and Materials Availability
All data associated with this study are present in the paper.
References
- Taichman RS. Blood and bone: Two tissues whose fates are intertwined to create the hematopoietic stem-cell niche. Blood 2005; 105:2631-2639.
- Pietschmann P, Rauner M, Sipos W, et al. Osteoporosis: An age-related and gender-specific disease–A mini review. Gerontology 2009; 55:3–12.
- New SA, Robins SP, Campbell MK, et al. Dietary influences on bone mass and bone metabolism: further evidence of a positive link between fruit and vegetable consumption and bone health? Am J Clin Nutr 2000; 71:142–151.
- Weaver CM. Vitamin D, calcium homeostasis, and skeleton accretion in children. J Bone Miner Res 2007; 22:45–49.
- Sayyari A, Farag Y. Prevalence of vitamin D deficiency in Saudi adults. Saudi Med J 2013;
- Al-Horani H, Abu Dayyih W, Mallah E, Hamad M, Mima M, Awad R, et al. Nationality, gender, age, and body mass index influences on Vitamin D concentration among elderly patients and young Iraqi and Jordanian in Jordan. Biochem Res Int. 2016;2016.
- Sadat-Ali M, Al-Omran AS, Al-Turki HA. Parathyroid glands response to low vitamin d levels in healthy adults: A cross-sectional study. Ulster Med J 2015; 84:26–29.
- Chapuy MC, Preziosi P, Maamer M, et al. Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int 1997; 7:439–443.
- Dawson-Hughes B, Harris SS, Dallal GE. Plasma calcidiol, season, and serum parathyroid hormone concentrations in healthy elderly men and women. Am J Clin Nutr 1997; 65:67–71.
- Du X, Greenfield H, Fraser DR, et al. Vitamin D deficiency and associated factors in adolescent girls in Beijing. Am J Clin Nutr 2001; 74:494–500.
- El-Hajj Fuleihan G, Nabulsi M, Choucair M, et al. Hypovitaminosis D in healthy schoolchildren. Pediatrics 2001; 107.
- Shakinba M, Tefagh S, Nafei Z. The optimal dose of vitamin D in growing girls during academic years: A randomized trial. Turk J Med Sci 2011; 41:33–37.
- McCabe MP, Smyth MP, Richardson DR. Current concept review: Vitamin D and stress fractures. Foot Ankle Int 2012; 33:526–533.
- Mori H, Okada Y, Tanaka Y. Incidence of vitamin d deficiency and its relevance to bone metabolism in Japanese postmenopausal women with type 2 diabetes mellitus. Intern Med 2015; 54:1599–604.
- Chin KY, Ima-Nirwana S, Ibrahim S, et al. Vitamin D status in Malaysian men and its associated factors. Nutrients 2014; 6:5419–5433.
- Khashayar P, Aghaei Meybodi HR, Homami MR, et al. The discriminative value of various biochemical parameters in detecting varying degrees of vitamin D deficiency in the Iranian population. Clin Lab 2011; 57:163–170.
- Al Faraj S, Al Mutairi K. Vitamin d deficiency and chronic low back pain in Saudi Arabia. Spine 2003; 28:177–179.
- Saqib MAN, Rafique I, Hayder I, et al. Comparison of vitamin D levels with bone density, calcium, phosphate, and alkaline phosphatase-An insight from major cities of Pakistan. J Pak Med Assoc 2018; 68:543–547.
Author Info
Mohammed A Noureddin1*, Abdullah S Al-Dosary2, Fahad M AlGhamdi2, Ziyad M Ali Alshehri2, Tariq F Bindaaj2 and Saud S Alanazi2
1Department of Medicine, Division of Nephrology, College of Medicine, Prince Sattam Bin Abdulaziz University, Al-Kharj, Kingdom of Saudi Arabia2Medical Students, College of Medicine, Prince Sattam Bin Abdulaziz University, Al-Kharj, Kingdom of Saudi Arabia
Citation: Mohammed A Noureddin, Alhumaidi M Alsubaie, Abdullah S Al-Dosarry, Fahad M Al-Ghamdi, Ziyad M Ali Alshehri, Tariq F Aldaej, Vitamin-D Deficiency and its Effect on Bone Profile: An Observational Study, J Res Med Dent Sci, 2020, 8 (6): 246-250.
Received: 07-Sep-2020 Accepted: 28-Sep-2020
