Research Article - (2022) Volume 10, Issue 8
Utility of Optic Nerve Sheath Diameter Measurement by Point of Care Ultrasound to Detect Raised Intracranial Pressure: A Prospective Observational Study
Hemanth VS, Sethu Babu* and Mithun Murali
*Correspondence: Sethu Babu, Department of Emergency Medicine, Pushpagiri Institute of Medical Sciences, Tiruvalla, Kerala, India, Email:
Abstract
Introduction: The main objective of the study was to evaluate the diagnostic utility of Optic Nerve Sheath Diameter (ONSD) measured by Point of Care Ultrasound (POCUS) to detect raised Intracranial Pressure (ICP) among high risk patients in the Emergency Department (ED).
Materials and Methods: Patients above the age of 18 years who presented to the Emergency department with signs and symptoms of raised ICP were included in the study. Patients with cataracts, severe maxillofacial injury, previous history of traumatic brain injury, or ocular surgery were excluded from the study. As per the institutional protocol, the patient was taken for CT head after initial stabilisation. Once the patient had returned back to the ED, investigator performed POCUS to measure ONSD. ONSD value equal to or greater than 5 mm (whether on right eye or left eye) was taken as abnormal. Raised ICP was diagnosed based on the findings of CT brain. Receiver Operating Characteristic curve (ROC) was drawn with ONSD to predict raised ICP and to determine the standard diagnostic test characteristics like Sensitivity, Specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV) and Accuracy.
Results: A total of 69 subjects with high clinical suspicion of raised ICP were included in the study. Of this, 50 subjects (72.5%) had CT findings consistent with raised ICP. 44 (63.8%) patients had the ONSD value of a single eye more than 5 mm. The average ONSD in patients with features of raised ICP in CT brain was 5.4 mm while that in those patients without features of raised ICP on CT brain was 4.4 mm. At the cut-off of 5 mm, ONSD measured by POCUS had a sensitivity of 88%, Specificity of 100%, Positive Predictive Value of 100% and Accuracy of 91.3% to diagnose raised ICP. ROC analysis revealed that the Area under curve (AUC) was 0.983 suggesting excellent discriminative capacity for ONSD to detect patients with raised ICP.
Conclusion: ONSD measurement by POCUS carries excellent accuracy to diagnose raised ICP among high risk patients in acute care settings.
Keywords: Optic nerve sheath diameter, Raised intracranial pressure, Point of care ultrasound
Introduction
Intracranial Pressure (ICP) is a fundamental parameter for monitoring critically ill neurological patients. Invasive intraventricular monitoring is considered the gold standard for ICP measurement [1]. Apart from being invasive and expensive; this modality is associated with complications such as infection, bleeding, mal positioning, and risk of neurological deficits [2]. CT and MRI are the alternative regular assessment techniques but transporting critically ill patients to the radiology department also poses danger [3]. Optic Nerve Sheath Diameter (ONSD) measured by Point of Care Ultra Sound (POCUS) has been showing promising results for early diagnosis of raised ICP in acute care settings. ONSD measurement by bedside ultrasound is simple to perform, cost-effective, and can be repeated multiple times without any risk of radiation. This can help in the early detection of raised intracranial pressure in the Emergency Department or any other acute care setting and can be repeated for revaluation to assess the response to treatment also. Early detection and proper monitoring of ICP help to initiate anti-edema measures promptly, thus improving the patient outcomes.
Systematic review and meta-analysis have confirmed that ocular ultrasound exhibits good diagnostic test accuracy for detecting raised ICP compared to head CT [4,5]. Previous studies have pointed out that ONSD, being an anatomical measurement made by ocular ultrasound, requires validation in different population subgroups based on age, gender, race, and ethnicity [6-10]. So far, the studies in the Indian population are limited in this regard. A previous study by Sahoo SS and Deepak Agrawal et al have reported a cut-off of 6.3 mm for predicting an ICP >20 mmHg in patients of neuro critical care by using Codman Intra parenchymal probes [11]. Their study was limited by the small sample size. Hence, the goal of our study was to gather further evidence regarding the applicability of ONSD in the Indian population, by determining the accuracy of ONSD measurement taken by POCUS in diagnosing raised ICP among high-risk patients in the Emergency department of a tertiary care hospital in South India.
Materials and Methods
Study design and procedure
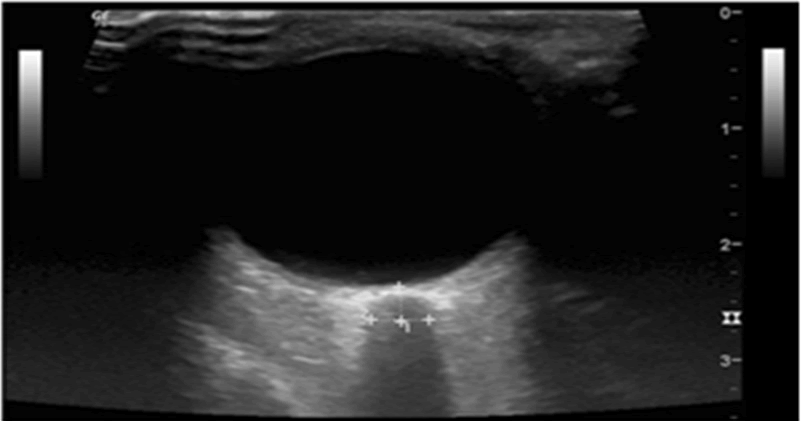
The study was conducted as a prospective observational study at the Department of Emergency Medicine, Pushpagiri Institute of Medical Sciences, Thiruvalla, and Kerala, India. The study was approved by the Institutional Research Committee and the Institutional Ethics Committee (PIMS and RC/IRC/413/’19). Assuming the 95% Confidence interval and 5% absolute precision with Sensitivity of 96% and Specificity of 94%, the required minimum sample size calculated was 60. Patients were recruited into the study from June 2019 to November 2020. Patients above the age of 18 years who presented to the Emergency Department (ED) with signs and symptoms of raised intracranial pressure (defined by the presence of 2 or more clinical features which include altered mental status, loss of consciousness, sudden onset severe headache with vomiting, seizures, anisocoria, and 6th cranial nerve palsy) were included in the study. Those patients with cataracts, prior history of ocular surgery, or traumatic brain injury were excluded. Upon the arrival of the patient to the ED, the treating physician did the initial evaluation and stabilization and the investigator were informed about the case. As per institutional protocol, the patient was transported to the Radiology Department for head CT imaging. Soon after the patient returned to the ED after Head CT, the investigator performed POCUS (using Sonority M Turbo TM) to measure Optic Nerve Sheath Diameter (ONSD). The measurement was done in a supine position with the patient directing his gaze anteriorly. The probe was applied horizontally over the closed eyelid after applying a copious amount of gel. ONSD was measured as the distance between the external borders of the hyperechoic area 3 mm posterior to the point where the optic nerve entered the globe, using an electronic calliper along the axis perpendicular to the retina for both eyes (Figure 1). Three recordings were taken from each eye and the average of these three values was taken. The higher ONSD value (whether Right or Left Eye) was taken for statistical analysis. Raised ICP was diagnosed based on the presence of Midline shift, diffuse cerebral oedema, effacement of sulci and gyri, or dilatation of the ventricles in Head CT.
Figure 1: ONSD measurement: Measured 3 mm behind the globe.
Statistical Analysis
Categorical and quantitative variables were expressed as frequency (percentage) and mean ± SD respectively. Descriptive statistics such as mean ± SD, Median with Inter Quartile Range, minimum and maximum were used to describe ONSD. Receiver Operating Characteristic (ROC) graphs was plotted and the Area under the Curve (AUC) was calculated to assess the diagnostic accuracy of ONSD in detecting raised ICP. Sensitivity, Specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV), and accuracy were calculated for ONSD in detecting raised ICP. For all statistical interpretations, p<0.05 was considered the threshold for statistical significance. Statistical analyses were performed by using a statistical software package SPSS, version 20.
Results
Baseline demographics
The study sample included 69 subjects who fulfilled the inclusion criteria. The mean age of the study population was 56 years (SD=19.7). The minimum age included in this study was 19 years and the maximum age was 89 years. Among the study population, 48 (69.6%) were males and 21 (30.4%) were females. These observations are shown in Table 1.
| Age | |
|---|---|
| Mean Age | 56 years (SD=19.7) |
| Minimum age | 19 years |
| Highest age | 89 years |
| Gender | Count (%) |
| Male | 48 (69.6%) |
| Female | 21 (30.4%) |
Table 1: Baseline demographics.
Distribution of the study population based on clinical features
Five clinical features of raised ICP were included-Loss of consciousness, altered sensorium, sudden onset severe headache, seizures, and anisocoria. The most common presentation was altered sensorium (87%). The distribution of other clinical features was Loss of consciousness (69.6%), severe headache (30.4%), Seizures (26.1%), and Anisocoria (27.5%). This is shown in Table 2.
| Clinical features | Count | Percent |
|---|---|---|
| Loss of consciousness | 48 | 69.6 |
| Altered sensorium | 60 | 87 |
| Severe headache | 21 | 30.4 |
| Seizures | 18 | 26.1 |
| Anisocoria | 19 | 27.5 |
Table 2: Distribution of the study population based on clinical features.
Distribution according to CT brain findings
Among 69 subjects, 64 patients (92.8%) had abnormal CT findings and 5 (7.2%) had normal CT. The most common CT diagnosis was Intra parenchymal hematoma (37.7%) followed by Subdural haemorrhage (34.8%) and Subarachnoid haemorrhage (34.8%). Other CT diagnoses were Ischaemic stroke (11.6%), Epidural haemorrhage (7.2%), and Brain tumour (2.9%) (Table 3).
| CT report | Count | Percent |
|---|---|---|
| EDH | 5 | 7.2 |
| SDH | 24 | 34.8 |
| SAH | 24 | 34.8 |
| Intra parenchymal hematoma | 26 | 37.7 |
| Ischemic stroke | 8 | 11.6 |
| Brain tumour/abscess | 2 | 2.9 |
| Normal | 5 | 7.2 |
Table 3: Distribution of the study sample based on CT brain diagnosis.
Midline shift, diffuse cerebral oedema, effacement of sulci and gyri, and dilatation of ventricles were taken as the features of raised ICP in CT. Even though 69 subjects with clinical suspicion of raised ICP were included in the study, 50 subjects (72.5%) had CT findings consistent with raised ICP. Analysing the CT report, 63.8% of subjects had midline shift, 60.9% had effacement of sulci and gyri and 4.3% had dilated ventricle (Table 4).
| Individual CT features suggestive of raised ICP* | Count | Percent |
|---|---|---|
| Midline shift | 44 | 63.8 |
| Effacement of Sulci and Gyri | 42 | 60.9 |
| Dilatation of Ventricles | 3 | 4.3 |
| Number of patients with CT features of raised ICP* | ||
| YES | 50 | 72.5 |
| NO | 19 | 27.5 |
| *Intracranial pressure | ||
Table 4: Distribution of the study population based on CT features suggestive of raised Intra cranial pressure.
Distribution according to the ONSD value
In this study, 44 (63.8%) of subjects had the ONSD value of a single eye equal to or more than 5 mm, and the rest, 25 (36.2%) had an ONSD value less than 5 mm (Table 5).
| ONSD * diameter (mm) | Count (Percent) |
|---|---|
| <5 mm | 25 (36.2%) |
| > 5 mm | 44 (63.8%) |
| *Optic Nerve Sheath Diameter | |
Table 5: Distribution of the study population according to the Optic nerve sheath diameter.
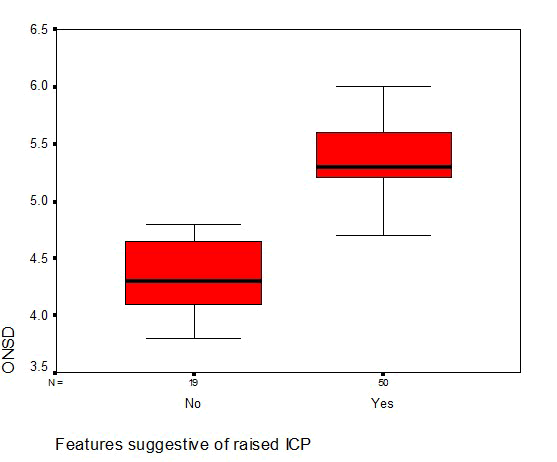
Mean ONSD in subjects with CT finding suggestive of raised ICP was 5.4 mm (standard deviation of 0.4 mm) and ranging between 4.5 mm to 6.2 mm. In patients without CT findings of raised ICP, mean ONSD was found to be 4.4 mm (standard deviation of 0.3 mm) and ranging between 3.8 mm to 4.8 mm (Table 6 and Figure 2).
| ONSD* | CT features suggestive of Raised ICP** | |
|---|---|---|
| NO | YES | |
| Mean+SD | 4.4 mm+0.3 | 5.4 mm+0.4 |
| Median (IQR) | 4.3 mm (4.1-4.7) | 5.3 mm (5.2-5.63) |
| Minimum | 3.8 mm | 4.5 mm |
| Maximum | 4.8 mm | 6.2 mm |
| *Optic nerve sheath diameter**Intracranial pressure | ||
Table 6: Descriptive statistics of ONSD according to the CT features of raised ICP.
Figure 2: Box plot for Optic Nerve sheath Diameter and CT features suggestive of raised intracranial pressure.
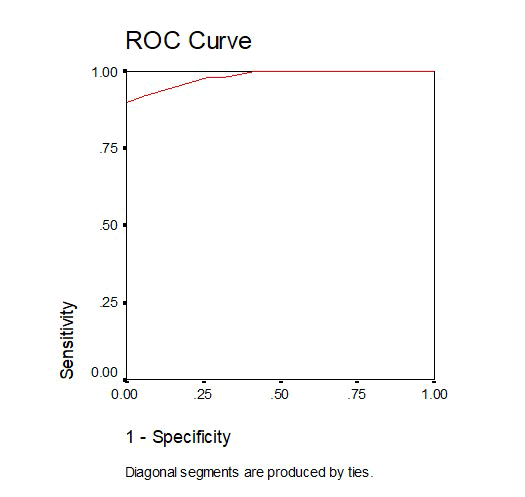
Receiver operating characteristic curve analysis with ONSD for diagnosing raised ICP
This is shown in Figure 3. The AUC was 0.983 ranging between 0.96-1 (p-value <0.01). The Sensitivity, Specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV), and Accuracy at the ONSD cut-off value of 5 mm are shown in Table 7.
| Sensitivity | 88% |
|---|---|
| Specificity | 100% |
| False negative rate | 12% |
| False positive rate | 0 |
| Positive predictive value | 100% |
| Negative predictive value | 76% |
| Accuracy | 91.3% |
Table 7: Standard test characteristics of ONSD at the cut off value of 5 mm for predicting raised intracranial pressure.
In this study, the accuracy of ONSD measured using POCUS to detect raised ICP was 91.3% with a Sensitivity of 88% and Specificity of 100%. Result also showed a 100% Positive Predictive Value and 76% Negative predictive value for diagnosing raised ICP with ONSD.
Figure 3: ROC curve for predicting raised ICP with ONSD.
Discussion
ONSD measurement by POCUS has recently emerged as a promising modality to identify raised ICP at bedside. ONSD measurement technique by POCUS can be learned easily by the acute care physician as the learning curve is short. This study is mainly intended to identify the standard diagnostic test characteristics of ONSD measurement by POCUS for predicting raised ICP among high-risk patient population.
The study has included 69 subjects who have possessed high clinical suspicion of having raised ICP. This sample is representative of a high risk population. The sample size of our study is comparable to that of other international studies [12-17]. In this study, due to practical considerations; we have taken CT brain as the reference standard to diagnose raised ICP.
The ROC and AUC analysis has revealed that, the curve being located in the left upper corner, ONSD by POCUS carries excellent discriminative capacity to detect raised ICP. At the ONSD cut of value of 5 mm, the test has carried a sensitivity of 88%, Specificity of 100%, PPV of 100%, and NPV of 76% and an overall accuracy of 91% to diagnose Raised ICP. These results are in accordance with the findings of the previous studies. The comparison between our study and other international studies is shown in Table 8.
| Study | Sample Size | ONSD cut off | Specificity | Sensitivity |
|---|---|---|---|---|
| Rajajee V | 65 | 4.8 mm | 94% | 96% |
| Blaivas | 35 | 5 mm | 95% | 100% |
| Tayal | 59 | 5 mm | 65% | 100% |
| Kimberly | 15 | 5 mm | 93% | 88% |
| Moretti | 94 | 5.2 mm | 73.8% | 93.1% |
| Major | 26 | 5 mm | 100% | 86% |
| Our study | 69 | 5 mm | 100% | 88% |
Table 8: Comparison of previous studies with our study.
As evident in the table, the standard diagnostic test characteristics of ONSD measurement by USG as a non-invasive parameter to detect raised ICP are almost similar to that of other international studies [12-17]. But we can see that the threshold value of the ONSD is different in each study. It may be due to the fact that ONSD varies according to age, region, and ethnicity. The strength of this study was its relatively high sample size compared to other similar studies (and includes all age group of adult population). So our study shows a strong relationship between signs of raised ICP on Head CT and optic nerve sheath diameter on ocular ultrasound.
Limitations of the study: This study has many limitations. First of all, this is a single centre study that has included 69 cases only. It needs to be validated in other settings and in a bigger population before extrapolating the results. The cut-off value of ONSD was more than or equal to 5 mm in this study. But it may vary depending on ethnicity, region, and age. Also, due to practical reasons, we used CT as our reference standard for the detection of raised ICP in this study even though invasive ICP monitoring is the gold standard. Additionally, a single investigator who is trained in ocular ultrasound has performed all the measurements hence inter observer variation is not assessed. Hence future studies are required to address all these issues and to gather further evidence in this regard.
Conclusion
Optic nerve sheath diameter measurement obtained by Point of care ultrasound carries excellent diagnostic accuracy to predict raised ICP among high-risk patients in acute care settings.
References
- Zhang X, Medow JE, Iskandar BJ, et al. Invasive and non-invasive means of measuring intracranial pressure: a review. Physiol Meas 2017; 38:143-182.
- Tavakoli S, Peitz G, Ares W, et al. Complications of invasive intracranial pressure monitoring devices in neurocritical care. Neurosurg Focus 2017; 43:6.
- Beckmann U, Gillies DM, Berenholtz SM, et al. Incidents relating to the intra-hospital transfer of critically ill patients. Intensive care medicine 2004; 30:1579-1585.
- Ohle R, McIsaac SM, Woo MY, et al. Sonography of the optic nerve sheath diameter for detection of raised intracranial pressure compared to computed tomography: a systematic review and meta-analysis. J Ultrasound Med 2015; 34:1285-1294.
- Robba C, Santori G, Czosnyka M, et al. Optic nerve sheath diameter measured sonographically as non-invasive estimator of intracranial pressure: a systematic review and meta-analysis. Intensive care med 2018; 44:1284-1294.
- Ballantyne J, Hollman AS, Hamilton R, et al. Transorbital optic nerve sheath ultrasonography in normal children. Clin radiol 1999; 54:740-742.
- Maude RR, Hossain MA, Hassan MU, et al. Transorbital sonographic evaluation of normal optic nerve sheath diameter in healthy volunteers in Bangladesh. PloS one 2013; 8:81013.
- Asghar A, Hashmi M, Hussain A. Optic nerve sheath diameter evaluated by transorbital sonography in healthy volunteers from Pakistan. Anaesthesia, Pain and Intensive Care. 2019; 282-286.
- Shrestha GS. Transorbital sonographic evaluation of normal optic nerve sheath diameter in healthy Nepalese adults. J Neuroanaesthesiol Criti Care 2016; 3:115-118.
- Steinborn M, Fiegler J, Ruedisser K, et al. Measurement of the optic nerve sheath diameter in children: comparison between transbulbar sonography and magnetic resonance imaging. Ultraschall Med 2012; 33:569-573.
- Sahoo SS, Agrawal D. Correlation of optic nerve sheath diameter with intracranial pressure monitoring in patients with severe traumatic brain injury. Indian J Neurotrauma 2013; 10:9-12.
- Rajajee V, Vanaman M, Fletcher JJ, et al. Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocriti care 2011; 15:506-515.
- Blaivas M, Theodoro D, Sierzenski PR. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad emerg med 2003; 10:376-381.
- Tayal VS, Neulander M, Norton HJ, et al. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann emerg med 2007; 49:508-514.
- Kimberly HH, Shah S, Marill K, et al. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med 2008; 15:201-204.
- Moretti R, Pizzi B, Cassini F, et al. Reliability of optic nerve ultrasound for the evaluation of patients with spontaneous intracranial hemorrhage. Neurocriti care 2009; 11:406-410.
- Major R, Girling S, Boyle A. Ultrasound measurement of optic nerve sheath diameter in patients with a clinical suspicion of raised intracranial pressure. Emerg Med J 2011; 28:679-681.
Author Info
Hemanth VS, Sethu Babu* and Mithun Murali
Department of Emergency Medicine, Pushpagiri Institute of Medical Sciences, Tiruvalla, Kerala, IndiaCitation: Hemanth VS, Sethu Babu, Mithun Murali, Utility of Optic Nerve Sheath Diameter Measurement by Point of Care Ultrasound to Detect Raised Intracranial Pressure: A Prospective Observational Study, J Res Med Dent Sci, 2022, 10 (7): 000-000.
Received: 07-Jun-2022, Manuscript No. JRMDS-22-57771; , Pre QC No. JRMDS-22-57771; Editor assigned: 10-Jun-2022, Pre QC No. JRMDS-22-57771; Reviewed: 24-Jul-2022, QC No. JRMDS-22-57771; Revised: 09-Aug-2022, Manuscript No. JRMDS-22-57771; Published: 17-Aug-2022