Research Article - (2022) Volume 10, Issue 12
Utility of Denta Scan in Evaluating Relationship of Inferior Alveolar Canal and Impacted Mandibular Third Molar Roots
Anuraag Bhaskar Choudhary1*, Mukta B Motwani1, Trupti Chordia2, Mayur B Chaudhary3, Pankaj Banode4 and Manoj Patil5
*Correspondence: Dr. Anuraag Bhaskar Choudhary, Department of Oral Medicine and Radiology, Vidya Shikshan Prasarak Mandal’s Dental College, Nagpur, Maharashtra, India, Email:
Abstract
Background: The impacted mandibular third molar may cause pathologies like pain, pericoronitis, periodontal infection, periapical infection, cellulitis, orthodontic problems, and facilitation of fracture of mandible at the angle of mandible, cyst and tumors from the tooth germ or follicle or from tooth itself. Any of these reasons could necessitate the extraction of the tooth, which could be either intentional or prophylactic. This study tried to evaluate the necessity of using CT as against only panoramic radiographs and the diagnostic accuracy of panoramic radiography for pre-operative assessment of patients with impacted mandibular third molars showing close approximation to the Inferior Alveolar Canal (IAC). Objectives: To evaluate the relationship of inferior alveolar canal to the impacted mandibular third molar root using radiographic markers on rotational panoramic radiographs (OPG) and assessing its true relationships on Computed Tomography (Dental CT) scan.
Methods: Patients referred for CT assessment of impacted lower third molars were used in this study. The lower third molars were assessed using OPG and on confirming the intimate relationship of third molar root relation to inferior alveolar canal, denta scan CT was done to determine the spatial relationship and morphology of the inferior dental canal relative to the roots and the cortical plates. The radiographic markers on panoramic radiographs were correlated with the CT findings when rotational panoramic radiographs were available.
Results: The 40 patients referred had 70 impacted, various radiographic markers used to determine the relation of inferior dental canal to the impacted mandibular third molar roots using OPG like S-Superimposition of canal on roots, Na- Narrowing of canal, R-Reduction in density of roots, D-Deviation of canal along with combination markers like S and RSuperimposition with Reduction in density of root, S and N-Superimposition with Narrowing and S and D-Superimposition with deviation using Chi square test (χ2) . There markers were compared with CT findings of Contact (C), Narrowing (N) and Thinning (T). Sensitivity and specificity of OPG was also evaluated with respect to CT markers using Fishers Exact test for accuracy using graph pad prism software.
Conclusions: Contacting of the inferior dental canal is a common finding when impacted lower third molars are assessed using CT. On rotational panoramic radiographs S and N of the inferior dental canal is the best predictor of contact of the inferior dental canal and its close relationship to the roots.
Keywords
Impacted, Third molar, Inferior alveolar nerve, Proximity, Dentascan, Panoramic radiograph
Introduction
An impacted tooth is one which because of some impediment is prevented from assuming its normal position in the arch at its physiological time of eruption [1]. The frequency with which certain teeth become impacted follows a particular order which includes mandibular third molars the most frequently, followed by maxillary third molars, the cuspids and less common the premolars and the incisors. The impacted mandibular third molar may cause pathologies like pain, pericoronitis, periodontal infection, periapical infection, cellulitis, orthodontic problems, facilitation of fracture of mandible at the angle of mandible, cyst and tumors from the tooth germ or follicle or from tooth itself. Any of these reasons could necessitate the extraction of the tooth, which could be either intentional or prophylactic [2]. Surgical removal of an impacted mandibular third molar needs a proper planning; this is all the more important in case of mandibular molars because of its relationship to the mandibular canal. This relationship of mandibular canal to the apices of mandibular third molar is of great academic and practical importance [3]. The radiographic diagnosis of impacted mandibular third molar predominates the planning of their surgical extraction. Radiographic assessment of the position of the tooth, the number and morphology of roots and in particular relationship between mandibular canal and third molar roots is mandatory before the surgical procedure [4]. The end of the 20th century marked a revolutionary change in the process of removal of impacted third molars as a result of improved imaging, as well as, surgical techniques [5].
The risk damage to inferior alveolar canal and injury to the inferior alveolar nerve is the most commonly reported risk during removal of lower third molars owing to its proximity to roots of third molar [6]. Several radiological methods have been used for evaluation of this intimate relationship of third molar roots and mandibular canal which includes right from the plane radiography viz intra oral periapical films, panoramic radiography (OPG), Multiple Narrow Beam Radiography (MNBR) or stereo radiography, occlusal radiographs, lateral radiographs and lateral skull radiographs. Although easy to acquire these aids carried disadvantages like inability to image the jaw in bucco lingual cross section and image distortion also invariably occurs [7,8]. A limitation of all these x-ray transmission radiography is that they are two dimensional production of complex extrinsically three dimensional anatomy which results in indistinguishable buccal and lingual structures as well as superimposition of other structures in bucco lingual cross sectional perspective tangential view. With the advent of the Computed Tomography (CT) scans greatly facilitated access to the internal morphology of soft and skeletal tissue without any magnification errors which are inherent in conventional radiographs because of geometric distortion [9]. Since the late 1980’s when dedicated software became available, multi planar reconstruction has been widely used in the pre-operative assessment of impacted mandibular third molars [10]. The emergence of dental Computed Tomographic (CT) reformatting programs revolutionized the process of radiological evaluation of jaws with provision of more accurate information about jaw dimensions and location of vital structures such as the mandibular canal. Excellent image quality eliminates the streak artifact from dental restorations [11]. The prediction of close proximity of inferior alveolar nerve to mandibular third molar roots relies mainly on radiographic analysis which provides a two dimensional image of a three dimensional object of interest or area [12]. In extraction of third molars with all the degrees of impactions where there is an intimate relationship of third molar roots and mandibular canal the incidence has been reported as high as 23-35% leading to severe discomfort for the patient when it occurs [13].
The present study was carried out to evaluate the necessity of using CT as against only panoramic radiographs for pre-operative assessment of patients with impacted mandibular third molars showing close approximation to the Inferior Alveolar Canal (IAC). It also evaluated the diagnostic accuracy of panoramic radiography for assessment of patients with impacted mandibular third molars showing close approximation to the Inferior Alveolar Canal (IAC).
Materials and Methdos
Study design
After the approval from institutional ethical committee this cross sectional study was conducted in the department of oral medicine and radiology of sharad pawar dental college and hospital, sawangi (meghe) and in department of radio diagnosis and imaging science at Acharya Vinoba Bhave Hospital, Sawangi, Datta Meghe Institute of Medical Sciences Deemed University (AVBRH, DU), Wardha, Maharashtra, India. The present study consisted 40 subjects with 70 impacted mandibular third molars, selected from OPD in oral medicine department after confirming the presence of an impacted mandibular third molar on clinical examination and asserting that Inferior Alveolar Nerve canal (IAN) was closely related to the roots of the impacted mandibular third molars in OPG. Each patient underwent clinical evaluation and the information was entered in the proforma after taking patient’s informed consent. After clinical evaluation a conventional OPG on planmeca proline CC panoramic xray, planmeca OY Helsinki, Finland, with parameters constant 68-70 kVp, constant 10 mA, 18 seconds and constant magnification of 1.2 and cassettes used were 6" × 12" (inches) Kodak Ektavision, Eastman Kodak company, New York, USA, was carried out to check the relationship of IAN to the roots of mandibular third molar. Only when a close relationship was seen, the patient was subjected for computed tomography evaluation on Multi Detector Cardiac spiral CT Scan (MDCT) machine. On entering the patients details on CT console, a lateral scout image was obtained and the section to be scanned was selected an scanning was done in caudal cranial direction beginning from inferior to the body of the mandible and extending superiorly to the middle of the rami. Images were reconstructed using dental CT software (dentascan) with following parameters of 120 kV, 250 mA with inbuilt denta scan software with pitch factor of 0.417, slice thickness 0.8 mm, Gantry tilt 0⁰, collimator width of 4 × 0.75 mm. After selecting the particular multi planar reconstruction images in all the axial, sagittal and coronal planes, the images were printed on Fuji dry fix films using Fuji laser printers.
The panoramic radiographs were evaluated for the presence of any of the radiographic (OPG) markers in relation to the impacted third molars and the mandibular canal as per the description [14]. Four panoramic radiographic markers predicting the close or intimate relationship of inferior alveolar nerve canal with that of roots of impacted mandibular third molars were evaluated which included: Superimposition–S (Figure 1) when the canal was superimposed over part of the roots and the root showed a uniform radiopaque area in that region as compared to the remaining portion of the root, Narrowing–N (Figure 2), when there was a narrowing of the inferior alveolar canal as it passes apical to the root of third molar at the expense of the top of the canal. The narrowing is usually at the expense of superior cortication of the canal, Reduction of root density–R (Figure 3) when part of the root was superimposed but was above the inferior cortex of the mandibular canal and appeared less radiopaque than the remaining radiological image of the roots the relation was considered to be reduced density (at apical third) and Deviation–D of the mandibular canal, when both superior and inferior cortication of the canal appears to be deviated than the normal oblique path in third molar region. In some cases a combination of markers may be present and these were grouped separately as three different combination markers like Superimposed with Narrowing–S and N (Figure 4) in such cases where both the radiographic signs like uniform radiopaque area as well as narrowing of the canal cortication were evident. Superimposed with Reduced density–S and R (Figure 5) when the roots superimposed the entire thickness of the canal but there was reduction in density of the roots in that area such cases were considered to be superimposed and reduced density. Superimposed with Deviation–S and D (Figure 6) in such cases where both the radiographic signs like superimposed roots as well as deviation of the mandibular canal were evident.
Figure 1: Panoramic radiograph showing superimposition mandibular canal by of third molar root.
Figure 2: Panoramic radiograph showing narrowing of mandibular canal.
Figure 3: Panoramic radiograph showing reduction in density of third molar root.
Figure 4: Panoramic radiograph showing superimposition with narrowing of mandibular canal by of third molar root.
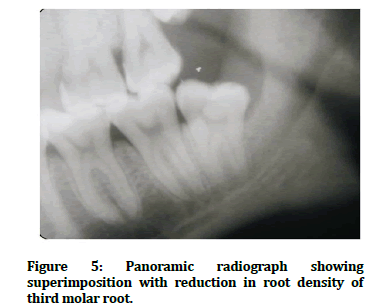
Figure 5: Panoramic radiograph showing superimposition with reduction in root density of third molar root.
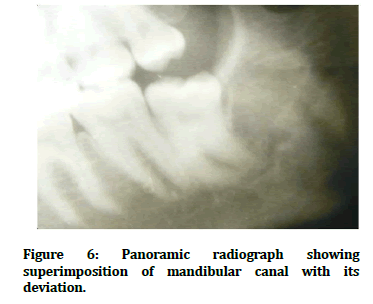
Figure 6: Panoramic radiograph showing superimposition of mandibular canal with its deviation.
All these 40 patients with 70 impacted molars underwent Computed Tomographic (CT) scan by using denta scan software for evaluating the contact with mandibular third molar roots as well as its thinning and narrowing in coronal section. A topogram is scanned digital projection radiographic image used for localization of the area to be examined (Figure 7). Data were acquired in the axial plane, but reformatted images were generated in the corrected sagittal and coronal planes to best demonstrate the location of the inferior dental canal (Figure 8a, b and c). Axial slices of 0.8 mm were then obtained as the primary data which was further utilized to achieve secondary and tertiary reconstructions in coronal and sagittal planes using dedicated software programmer called as dental CT by dental planning. The coronal reformatted view also provided the information regarding any evidence of narrowing, contact and thinning of cortex of mandibular canal in relation to roots of impacted mandibular third molars (Figure 9). The sagittal reconstruction images depict the ramus and body of mandible in sagittal plane similar to that seen in a true lateral radiographs or panoramic radiograph. The relationship of mandibular canal to root apices of impacted teeth will be evident in these sections. The findings were evaluated and statistical analysis was done using z test for single proportion and chi square test using graph pad prism software. All the panoramic radiographic markers were compared with the CT markers and assessed to determine the true contact and thinning of inferior alveolar canal cortication. Also sensitivity and specificity of panoramic radiographic markers for contact of the canal was evaluated using test statistics and fisher's exact test using the same software.
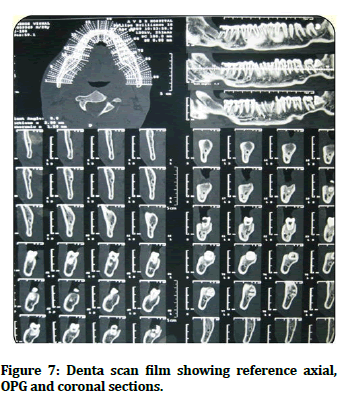
Figure 7: Denta scan film showing reference axial, OPG and coronal sections.

Figure 8 a, b and c: Denta scan images in MPR sections (C-canal R- root).
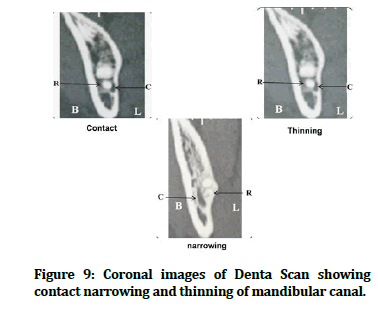
Figure 9: Coronal images of Denta Scan showing contact narrowing and thinning of mandibular canal.
Results
Considering all the inclusion and exclusion criteria a total 40 subjects with 70 impacted mandibular third molars having a positive radiographic signs of root approximation with inferior alveolar canal as seen in Orthopantomogram (OPG) were selected for the study. These patients were divided according to panoramic radiographic markers and data was tabulated and also presented as graphical representations. All the samples then underwent CT scan and separate CT markers were evaluated and used to find out the spatial relationship of mandibular canal, narrowing, contact and thinning of the cortication of mandibular canal. The various radiographic markers used to determine the relation of inferior dental canal to the impacted mandibular third molar roots using rotational panoramic radiographs were SSuperimposition of canal on roots, Na-Narrowing of canal, R-Reduction in density of roots, D-Deviation of canal, S and R-Superimposition with Reduction in density of root, S and N-Superimposition with Narrowing and S and D-Superimposition with and Deviation. Out of 70 impacted mandibular third molars the maximum number of third molars showed S (35) followed by S and R (17), S and N (12), Na (3), S and D (2) and R (1). There was not a single case of deviation alone (Table 1 and Figure 10). All the patients were subjected to the Spiral CT scan and the following findings were noted. On CT evaluation of coronal MPR images for evidence of contact, narrowing and thinning of canal cortication, out of 70 impacted mandibular third molars 49 (70%) cases showed contact on CT, 19 (38.77%) cases also showed narrowing of inferior alveolar canal in relation to impacted mandibular third molars along with contact whereas there was thinning of canal cortication along with contact in 34 (69.38%) cases. 4 cases showed only contact of the canal with the roots without narrowing or thinning. While evaluating the MPR images 20 (28.57%) cases showed the presence of all the CT markers like narrowing, contact and thinning, whereas 21 (28.57%) cases showed no contact of mandibular canal with the third molar roots (Table 2 and Figure 11). When comparing the panoramic radiographic markers with the CT findings of cases where all the three CT markers were present, significant results were seen in S, S and R and S and N which were 3.22, 3.04 and 2.44 respectively (Table 3 and Figure 12). When comparing the panoramic radiographic markers with the CT findings of cases where no contact of the mandibular canal was evident on CT scan images, the significant results were observed in S, N, S and R, S and N and S and D which were 50.00, 4.29, 24.29, 17.17 and 2.86 respectively (Table 4 and Figure 13). The sensitivity of the panoramic radiographic marker superimposition was found to be 52.27% with specificity of 53.85%. The positive predictive value was 65.71% and the negative predictive value was 40%. For narrowing of the canal, sensitivity and specificity was calculated to be 8.69% and 97.87% respectively, whereas the accuracy rate was 52%. Similarly when radiographic marker of reduction in root density of the roots of third molars is evident then the specificity was 100% along with the positive predictive value was 100%; the sensitivity was only 4.54% and accuracy rate of 70%. When superimposition with reduction in density of the root was observed then sensitivity and specificity was found to be 30% and 80% respectively with accuracy rate of 58.57%. However when the radiographic markers of superimposition with narrowing of mandibular canal was observed the specificity was found to be 100% with positive predictive value also to be 100% along with significant p value. The accuracy rate was 70% which was highest. The sensitivity and specificity for superimposition with deviation was evaluated to be 8.69% and 100% respectively with the positive and negative predictive value was found to be 100% and 69.12% respectively. The accuracy rate was also 70% (Table 5).
| Panoramic radiograph group (n=70) | Number | Percentage (%) |
|---|---|---|
| S | 35 | 50.00 |
| N | 3 | 4.29 |
| R | 1 | 1.43 |
| D | 0 | 0.00 |
| S and R | 17 | 24.29 |
| S and N | 12 | 17.14 |
| S and D | 2 | 2.85 |
| Total | 70 | 100 |
| S-Superimposition of canal on roots; N-Narrowing of canal; R-Reduction in density of roots; D-Deviation of canal | ||
Table 1: Radiographic markers indicating relationship of inferior alveolar nerve canal with impacted mandibular third molar roots on panoramic radiograph.
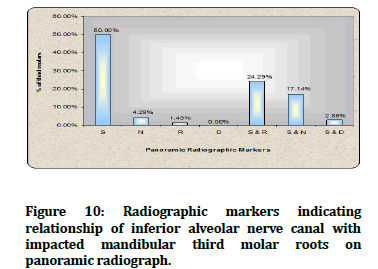
Figure 10: Radiographic markers indicating relationship of inferior alveolar nerve canal with impacted mandibular third molar roots on panoramic radiograph.
| CT findings (markers) | Number | Percentage (%) |
|---|---|---|
| Contact (C) | 49 | 70% |
| Narrowing (N) | 19 | 27.14% |
| Thinning (T) | 34 | 48.57% |
| N, C and T | 20 | 28.57% |
| No contact | 21 | 30% |
Table 2: CT markers indicating relationship of inferior alveolar nerve canal with impacted mandibular third molar roots on panoramic radiograph.
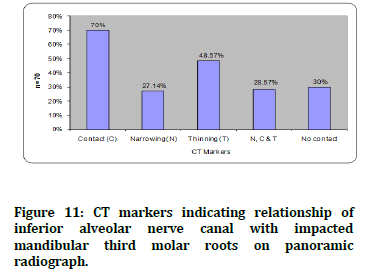
Figure 11: CT markers indicating relationship of inferior alveolar nerve canal with impacted mandibular third molar roots on panoramic radiograph.
| Panoramic radiograph group | Number in OPG group (n=70) | Number with narrowing, contact and thinning on CT (n=20) | Proportion with narrowing, contact and thinning on CT | Z |
|---|---|---|---|---|
| S | 35 | 8 | 0.23 | 3.22,S |
| N | 3 | - | 0.00 | NA |
| R | 1 | 1 | 1.00 | NA |
| D | 0 | - | - | - |
| S and R | 17 | 6 | 0.35 | 3.04,S |
| S and N | 12 | 4 | 0.33 | 2.44,S |
| S and D | 2 | 1 | 0.50 | 1.41,NS |
| S-Superimposition of canal on roots; N-Narrowing of canal; R-Reduction in density of roots, D-Deviation of canal | ||||
Table 3: Comparison of panoramic radiographic markers with CT showing all the three CT markers narrowing, contacting and thinning of the inferior dental canal.
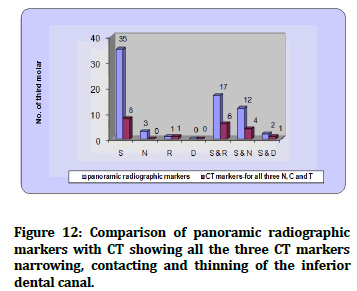
Figure 12: Comparison of panoramic radiographic markers with CT showing all the three CT markers narrowing, contacting and thinning of the inferior dental canal.
| Panoramic radiograph group | Number in OPG group (n=70) | Number with no contact on CT (n=21) | Proportion with no contact on CT | Z |
|---|---|---|---|---|
| S | 35 | 12 | 0.34 | 50.00, S |
| N | 3 | 1 | 0.33 | 4.29, S |
| R | 1 | - | 0.00 | 1.43, NS |
| D | 0 | - | 0.00 | 0.00, NS |
| S and R | 17 | 8 | 0.47 | 24.29, S |
| S and N | 12 | - | 0.00 | 17.17, S |
| S and D | 2 | - | 0.00 | 2.86, S |
| S-Superimposition of canal on roots; N-Narrowing of canal; R-Reduction in density of roots; D-Deviation of canal | ||||
Table 4: Comparison of panoramic radiographic markers with CT where there was no contact of the inferior alveolar nerve canal.
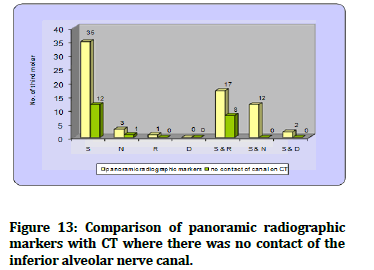
Figure 13: Comparison of panoramic radiographic markers with CT where there was no contact of the inferior alveolar nerve canal.
OPG finding |
S |
N |
R |
S and R |
S and N |
S and D |
|---|---|---|---|---|---|---|
Positive |
23 |
12 |
2 |
1 |
1 |
0 |
Negative |
21 |
14 |
21 |
46 |
21 |
48 |
Sensitivity |
52.27% |
8.69% |
4.54% |
30% |
36.36% |
8.69% |
Specificity |
53.85% |
97.87% |
100% |
80% |
100% |
100% |
Positive Predictive Value (PPV) |
65.71% |
66.67% |
100% |
52.94% |
100% |
100% |
Negative Predictive Value (NPV) |
40% |
68.66% |
69.57% |
60.38% |
63.80% |
69.12% |
Fisher’s exact test (p-value S if p>0.05) |
0.8, NS |
0.24,NS |
0.31, NS |
0.40, NS |
0.0001, S |
0.10, NS |
Accuracy |
52% |
68.57% |
70% |
58.57% |
70% |
70% |
Table 5: Sensitivity and specificity of panoramic radiographic markers.
Discussion
The potential treatment complications and resultant patient morbidity associated with the removal of complex impacted mandibular third molar are well known. When emphasizing prevention of complications it has been indicated that recognizing the difficulty of the proposed extraction is paramount and one of the most important steps is to obtain appropriate radiographs, depicting the exact location of the inferior alveolar nerve canal. Damage to the nerve manifests itself as a sensory disturbance of the lower lip and chin up to the midline. Howe and Poyton were of the view that for the teeth in true relationship to the IAN the occurrence ranges up to 35.6% [15]. Bell suggested that conventional radiographs (OPG) has been recommended as the primary investigation of choice in the pre-operative assessment of mandibular third molars [16]. However, it lacks in furnishing the diagnostic information with respect to spatial anatomic location of specific anatomic structures like mandibular canal and root relationship of impacted third molars [17]. Radiographic evidence of deep impactions and horizontal impactions were associated with altered labial sensation suggests that any relationships between roots of mandibular third molars and the mandibular canal seen on panoramic radiograph may be associated with post-operative dysesthesia, with two factors significantly associated viz distance between the root tips and the superior canal cortication (encroachments), cases with superimposed roots over canal with roots appearing more radiolucent (radiolucent band) and loss of lamina dura indicating break in the continuity of the radio dense canal borders narrowing of canal, cases without any distinction [18]. Chaipasco, et al. evaluated the incidence of complications and side effects of mandibular third molar surgery was 1.1% and 4% respectively and damage to inferior alveolar nerve was 0.7% respectively [19]. Also the sensory impairment of lingual and inferior alveolar nerves following removal of impacted mandibular third molars are significantly depended on factors like patient’s age, development of roots, the degree of impactions, and radiographic position of the nerve canal [20].
Though the panoramic radiographs provide mesio distal and vertical position of the impacted tooth clearly, the bucco lingual angulation is not reflected. Use of CT with computer generated image is able to better portray the 3D anatomical picture and spatial relationships of anatomical structures. Hence CT has been preferred for dental imaging. CT with Multi Planar Reformatting (MPR) is as the most reliable technique for the assessment of bone measurements and localization of anatomic structures.
On evaluating the panoramic radiographic markers the present study showed that out of total 70 impacted mandibular third molars 35 teeth showed only superimposition with mandibular canal, 3 teeth showed only narrowing and 1 tooth showed only reduction in density. Superimposition along with Reduction in density (S and R) was seen in 17 cases whereas Superimposition along with Narrowing (S and N) was seen in 12 cases. Deviation of mandibular canal alone was not evident in any of the radiographs, but the Deviation along with Superimposition (S and D) was seen in 2 cases. Mahasantipiya, et al. in their study also found maximum teeth to be in superimposition group followed by Superimposition along with Narrowing (S and N) and superimposition and reduction in root density. Bell in his study also found the most common radiographic appearance was superimposition (110 teeth) but when he compared these with intra operative findings there was intimate relation with inferior alveolar canal only in 12 cases. Therefore superimposition alone cannot be a predictor for the intimate relation of the canal to the roots of impacted mandibular third molars. Bell in his study further stated that the deflection of inferior alveolar nerve canal and reduction in root density were the most common radiographic signs associated with intimate contact between third molar roots and inferior alveolar canal [21]. In our study there was no case of deviation and only 1 case of reduction of root density although there were 2 cases of superimposition along with deviation observed on panoramic radiograph Studies by Tammisalo, et al. and Monaco, et al. have also stated that the Superimposition (S) of the mandibular third molar roots and mandibular canal is seen in 40-80% of the radiographs of impacted mandibular third molar roots although most of the third molar surgeries are without complications, asserting the fact that the diagnostic accuracy of superimposition on dental panoramic radiograph is disappointingly low [22].
On evaluating the dentascan images out of 70 impacted mandibular third molars, the mandibular canal was seen to be in contact with 49 (70%) mandibular third molars. Out of these 19 (27.14%) cases also showed narrowing of canal and 34 (48.57%) also showed thinning of the superior cortex and 20 (28.57%) showed all the three features. Out of these 70 impacted third molars which showed intimate contact with mandibular canal in panoramic radiographs, 21 (30%) teeth did not show any contact when examined on dentascan. All the 70 cases were selected on the criteria that they had an intimate contact with the canal on OPG, irrespective of the type of radiographic marker seen, but only 70% of these teeth were actually in contact as seen from CT scans and in 30% cases the canal was away from the roots. Monaco, et al. in their study also found a true relationship of the canal in 74% cases, whereas, Ohman, et al. has given the presence of the contact in 94% cases. When CT markers were compared with panoramic radiographic markers, out of 35 teeth with superimposition of roots over canal on OPG, 3 were found having contact with the mandibular canal on CT which was statistically significant. Significant values were also seen when narrowing and superimposition with reduction in density of the roots was compared with the CT findings. In the present study there were 31 cases where more than one radiographic marker were present and out of these 23 showed a true relationship between mandibular canal and third molar roots. All the cases of superimposition with narrowing and superimposition with deviation were seen to be in contact with the canal suggesting that if more than one panoramic radiographic markers are evident on panoramic radiographs, then the chances of the canal being in contact with the third molar roots are high. Monaco, et al. also found in their study that in all cases where two or more radiographic markers were evident, a true relationship between the mandibular canal and the third molar on the CT scan was evident. Mahasantipiya, et al. in their study found that maximum number of sites of Superimposition (S) was seen to be in contact with inferior alveolar canal.
When sensitivity and specificity of these radiographic markers were evaluated the values were statistically significant for Superimposition with Narrowing (S and N) only. The specificity was found to be 100% but the sensitivity was only 8.96%, whereas the positive predictive value was also 100%. Thus indicating that an intimate relationship of the mandibular canal with the third molar roots can be predicted on OPG by these combination markers, but they have a very low sensitivity, emphasizing the need to locate and to evaluate the true relationship by other confirmatory imaging modalities. The specificity of 100% was also observed at the sites where reduction of the Root density (R) and Superimposition with root reduction in Density was observed (S and D) and at sites where there was Narrowing (N) of mandibular canal alone. The positive predictive values in these cases were also evaluated as maximum (100%) for radiographic markers like reduction in Root density (R), Superimposition with Narrowing (S and N) and Superimposition with Deviation of canal (S and D). The accuracy rate was found to be 70% which is highest for all the combination markers except for Superimposition with reduction of Root density (S and R). 70 % accuracy rate was also seen with radiographic marker reduction in Root density (R), followed by Narrowing (N) which was 68.5% the least accuracy was seen with Superimposition (S) and Superimposition with reduction in Root density (S and R), although the maximum number of cases were seen in these two groups. From this it can be concluded that superimposition is not an ideal marker to indicate the intimate contact of the nerve to the third molars. Narrowing of the canal and when more than one marker is present, the inferior alveolar canal is likely to be in contact with the roots of the molars suggesting that careful planning has to be done for removal of such teeth. Similarly findings were obtained by Monaco, et al. in their study, in all cases where two or more radiographic markers were evident, a true relationship between the mandibular canal and the third molar on the CT scan was evident as well as positive predictive value for the relationship of third molar roots with canal was 100%. Similar findings were reported by Khan, et al. [23].
In our study we can suggest that it is not necessary to perform a CT scan for each and every patients although all the panoramic radiographic markers utilized in the study did not show significant results, but markers like superimposition, superimposition with narrowing and superimposition with deviation of mandibular canal have shown significant relations, with specificity being 100% for both superimposition with narrowing and superimposition with deviation. This could mean that whenever these two markers are present a CT evaluation would become necessary. But none of the markers have shown sensitivity more than 50% which could mean that each time an intimate contact cannot be predicted on the basis of panoramic radiographic markers. Therefore the choice of most appropriate imaging modality should be based on the requirements of image quality, expected details and the clinical circumstances.
Conclusion
The present study was carried out to evaluate the potential advantage of Computed Tomography (CT) over Panoramic Radiographs (OPG) in pre-operative evaluation of patients with impacted mandibular third molars with intimate relationship with the inferior alveolar nerve canal. The results of this study will help to frame some useful guidelines for oral surgeons and facilitate the determination of precise anatomical relationship between the teeth and the mandibular canal. Evaluation of the seven radiographic markers like Superimposition (S) Narrowing (Na), Reduction of root density (R), Deviation of the mandibular canal (D), as well as combination of the above two factors i.e. Superimposition with Narrowing (S and N), Superimposition with reduction in Root density (S and R) and Superimposition with Deviation of the canal (S and D) suggested that out of these markers, only Superimposition with Narrowing (S and N) had a high predictive value in identifying a contact between the lower third molar root and the mandibular canal. Under these circumstances, it could be suggested that a CT scan should be obtained to confirm the exact relationship of the mandibular canal to the third molar roots.
References
- Sandhu SS, Kapila BK. Incidence of impacted third molars. J Indian Dent Asso 1982; 54:441-444.
- Grover SP, Lorton L. The incidence of un-erupted permanent teeth and related clinical cases. Oral Surg Oral Med Oral Pathol 1985; 59:420-425.
- Tammisalo T, Happonen RP, Tammisalo EH. Stereographic assessment of mandibular canal in relation to the roots of impacted lower third molars using multi projection narrow beam radiography. Int J Oral Maxillofac Surg 1992; 21:85-89.
- Lam EWN, Ruprecht A, Yang J. Comparison of two dimensional and ortho radially reformatted computed tomography and panoramic radiography for dental implant treatment planning. J Prosthet Dent 1995; 74:42-46.
- Vannier MW, Hildebolt CF, Conover G et al. Three dimensional dental imaging by Spiral CT. A progress report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 84:561-570.
- Preda L, Di Maggio EM, Dore R, et al. Use of spiral computed tomography for multi planar dental reconstruction. Dentomaxillofac Radiol 1997; 26:327-331.
- Wenzel A, Aagaard E, Sindet Pederson S. Evaluation of new radiographic technique: Outcome following removal of mandibular third molars. Dentomaxillofacial Radiol 1998; 27:264-269.
- Wenzel A and Verdonschot E. H. Evaluation of new radiographic technique: outcome following removal of mandibular third molars. Dentomaxillofacial Radiology 1998; 27:264-269.
- Flick GW. The third molar controversy: Framing the controversy as a public health policy issue. J Oral Maxillofac Surg 1999; 57:438-444.
- Valmaseda Castellon E, Berini Aytes L, Gay Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: A prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92:377-383.
- Abrahams JJ. Dental CT imaging: A look at the jaw. Radiol 2001; 219:334–345.
- Tay ABG, Go WS. Effect of exposed inferior alveolar neurovascular bundle during surgical removal of impacted lower third molars. J Oral Maxillofac Surg 2004; 62:592-600.
- Maegawa H, Sano K, Kitagawa Y, et al. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96:639-646.
- Mahasantipiya PM, Savage NW, Monsour PA, et al. Narrowing of the inferior dental canal in relation to the lower third molars. Dento Maxillofacial Radiol 2005; 34:154–163.
- Howe GL. Prevention of damage to the inferior alveolar nerve during the extraction of mandibular third molars. Bri Dent J 1960; 109:355-363.
- Bell GW, Rodgers JM, Grime RJ, et al. The accuracy of dental panoramic tomographs in determining the root morphology of mandibular third molar teeth before surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 95:119-125.
- Ylikontiola L, Moberg K, Hummonen S, et al. Comparison of three radiographic methods used to locate the mandibular canal in the buccolingual direction before bilateral sagittal split osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93:736-742.
- Mercier P, Precious D. Risks and benefits of impacted third molars-A critical review of the literature. Int J Oral Maxillofac Surg 1992; 21:17-27.
- Chaipasco M, Cicco LD, Marrone G. Side effects and complications associated with third molar surgery. Oral Surg Oral Med Oral Pathol 1993; 76:412-420.
- Renton T, Hankins M, Sproate C, et al. A randomized controlled clinical trial to compare the incidence of injury to the inferior alveolar nerve as a result of coronectomy and removal of mandibular third molars. Br J Oral Maxillofac Surg 2005; 43:7-12.
- Bell GW. Use of dental panoramic tomographs to predict the relation between mandibular third molar teeth and the inferior alveolar nerve. Radiological and surgical findings and clinical outcome. Br J Oral Maxillofac Surg 2004; 42:21-27.
- Monaco G, Montevecchi M, Bonetti GL, et al. Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc 2004; 135:312-318.
- Khan I, Halli R, Gadre P, et al. Correlation of panoramic radiographs and spiral CT scan in the preoperative assessment of intimacy of the inferior alveolar canal to impacted mandibular third molars. J Craniofac Surg 2011; 22:566–570.
Author Info
Anuraag Bhaskar Choudhary1*, Mukta B Motwani1, Trupti Chordia2, Mayur B Chaudhary3, Pankaj Banode4 and Manoj Patil5
1Department of Oral Medicine and Radiology, Vidya Shikshan Prasarak Mandal’s Dental College, Nagpur, Maharashtra, India2Department of Oral Pathology and Microbiology, Vidya Shikshan Prasarak Mandal’s Dental College, Nagpur, Maharashtra, India
3Department of Oral Pathology, Bharti Vidyapeeth, Pune, Maharashtra, India
4Department of Radio Diagnosis and Imaging Sciences, Acharya Vinoba Bhave Rural Hospital, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India
5Department of Community Medicine, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India
Citation: Anuraag Bhaskar Choudhary, Mukta B Motwani, Trupti Chordia, Mayur B Chaudhary, Pankaj Banode, Manoj Patil, Utility of Dentascan in Evaluating Relationship of Inferior Alveolar Canal and Impacted Mandibular Third Molar Roots, J Res Med Dent Sci, 2022, 10 (12): 109-118.
Received: 03-Oct-2022, Manuscript No. JRMDS-22-49671 ; , Pre QC No. JRMDS-22-49671(PQ) ; Editor assigned: 07-Oct-2022, Pre QC No. JRMDS-22-49671(PQ) ; Reviewed: 21-Oct-2022, QC No. JRMDS-22-49671 ; Revised: 05-Dec-2022, Manuscript No. JRMDS-22-49671(R) ; Published: 12-Dec-2022
