Research - (2021) Volume 9, Issue 8
Usage of Sling Suture and Horizontal Mattress Suture Following Third Molar Surgeries
Ramvihari Thota* and Senthilnathan Periasamy
*Correspondence: Ramvihari Thota, Department of Oral & Maxillofacial Surgery, Saveetha Dental College, Saveetha Institute of Medical and Technical Science, Saveetha University Tamilnadu, India, Email:
Abstract
Aim: The aim of this clinical study was to compare the influence of 2 different suturing techniques on postoperative complications and wound healing after surgical extractions of impacted mandibular third molars. Materials and methods: In this randomized split mouth study, 30 patients were examined in whom 60 consecutive surgical extractions of symmetrically positioned impacted mandibular third molars were performed. After the extractions, the surgical flaps were sutured with either the sling or horizontal mattress suturing technique. Postoperative swelling and trismus were recorded on the 3rd, 7th, and wound dehiscence was recorded on the10th postoperative days. Results: The sling suture was significantly superior regarding the improvement of periodontal pocket depth. The dehiscence was significantly smaller in the horizontal mattress suture group 7 days postoperatively. This difference was not significant 14 days postoperatively. Conclusion: The results of this study show that the sling suture was superior to the horizontal mattress suture regarding periodontal pocket depth. Whereas horizontal mattress suture showed better healing compared to sling suture. However, the technique of suturing does not seem to have a significant long-term effect on wound dehiscence.
Keywords
Third molars, Sling sutures, Horizontal mattress suture, Suturing technique, wound healingIntroduction
In general, 90% of the world’s population have third molar teeth, which are impacted in 33% of the cases [1]. Surgical extraction of impacted third molars traumatizes the hard and soft tissues. Resultantly, patients often experience pain, edema, and trismus postoperatively, which decrease their quality of life [2-5]
Wound dehiscence (separation of wound edges) is among the complications that can delay wound healing. Dehiscence often occurs due to two main reasons, namely the absence of a sufficient amount of bone beneath the flap and suturing the wound under tension [6]. Primary closure of the flap decreases the incidence of dehiscence after suturing and improves wound healing. In some cases, dehiscence may occur secondarily and heal with no complication. However, patients experience discomfort and constant pain during this period. Moreover, dehiscence may result in alveolar osteitis or clinical attachment loss (CAL) at the distal surface of the adjacent second molar tooth [7]. Periodontal problems at the distal surface of the second molars are among other possible complications following surgical extraction of impacted mandibular third molars [8]. Age, third molar inclination, large contact area, visible plaque on the distal surface of second molars, and pathologically enlarged third molar follicles are among the risk factors related to periodontal pocket formation around second molars adjacent to impacted third molars [9]. Surgeons can take measures to minimize the risk of postoperative complications [6].
There is controversy regarding the effects of techniques of wound closure following third molar extraction surgery on the rate of complications. Wound closure can be categorized into two types of primary and secondary closure. Primary closure is defined as primary complete coverage of the surgical site with the muco periosteum. In secondary closure, a window remains, which is managed secondarily [10]. Plaque accumulation affects wound healing, and dehiscence occurs due to the presence of inflammation. Unlike the single interrupted suture, the knot in the sling technique is located far from the distal surface of second molars where dehiscence mostly occurs [11,12]. Different suturing techniques are employed for advanced soft tissue closure [13]. The single interrupted suture is used to approximate the buccal and lingual flaps. The sling suture is also used to prevent gingival recession around teeth and dental crowns [6]. Sling sutures are used to cover the exposed root surfaces in advanced flap surgeries and to attach the papilla to the interdental connective tissue. The efficacy of single interrupted and sling sutures after impacted third molar extraction surgery has not been compared so far. Considering the advantages of sling sutures in decreasing postoperative complications, this study aimed to compare sling and single interrupted sutures in terms of dehiscence, probing pocket depth (PPD), and CAL around the adjacent second molar tooth after surgical extraction of third molars to find out whether the sling suturing technique can decrease postoperative complications.
Materials and Methods
This split-mouth randomized clinical trial involved patients with impacted mandibular third molars requiring surgical extraction. The study has been approved by the Ethics Committee of Saveetha dental college and hospitals. The variables were PPD, CAL, healing and wound dehiscence, which were evaluated after surgical procedures. A total of 60 mandibular impacted third molar surgeries were performed on 30 patients on separate occasions. Each patient had fairly symmetrically positioned, bone retained asymptomatic and class III B surgical difficulty grade (scales of Pell– Gregory and Winter) mandibular third molars. Patients with any systemic disease, pregnancy, poor oral hygiene or aged <18 were excluded from the study. All surgical procedures were performed by the same surgeon with the same flap design.
The inclusion criteria were as follows: patients with equal bilateral semi-impacted or impacted mandibular third molars. The degree of impaction was determined according to a classification by Pell and Gregory. The soft tissue coverage over the teeth was determined using a probe. Patients were between 18 to 25 years of age, nonsmokers, systemically healthy, not pregnant or nursing, and not taking any medication within the past six months; they had no inflammatory condition (such as acute pericoronitis or periodontal disease), patients with good hygiene were included in the study. The exclusion criteria included patients with asymmetrically impacted teeth, the presence of inflammation in the oral cavity, poor oral hygiene.
The surgeries of right and left impacted mandibular third molars were performed in 2 sessions at a 4-week interval in all patients. The type of suturing technique was randomly selected for each side. Before the surgery, all patients were given 0.2% chlorhexidine mouth rinse for 30 seconds. Then, local anaesthetic lignocaine with 1:200,000 adrenaline was administered to sustain local anaesthesia of the inferior alveolar nerve and buccal nerve respectively. All impacted mandibular third molar surgeries were performed with the traditional triangular flap. The surgical incision was started from the rising edge of the anterior border of the mandibular ramus to the distal surface of the distobuccal cup of the mandibular second molar. The incision was then continued along the sulcus of the buccal side of the mandibular second molar. Finally, a vertical incision was made to relieve the flap. The mucoperiosteum was elevated with a periosteal elevator and the alveolar bone around the impacted molar was removed with a round burr under saline irrigation. The impacted tooth was sectioned with a fissure bur and extracted using an elevator and a third molar forceps. The primary wound closure of each patient was applied with the sling sutures on 1 side (Group A) (Figure 1) and with horizontal mattress sutures on the other side (Group B) (Figure 2) using 3/0 synthetic silk sutures. All vertical releasing incisions in all patients were sutured with simple interrupted sutures to relieve edema (Figure 1). After the surgery, the patients were prescribed NSAIDs twice per day, 500 mg amoxicillin 3 times per day, and 2% chlorhexidine gluconate for 5 days. All patients were recalled on the 3rd and 7th days postoperatively for the evaluation of postoperative complications.
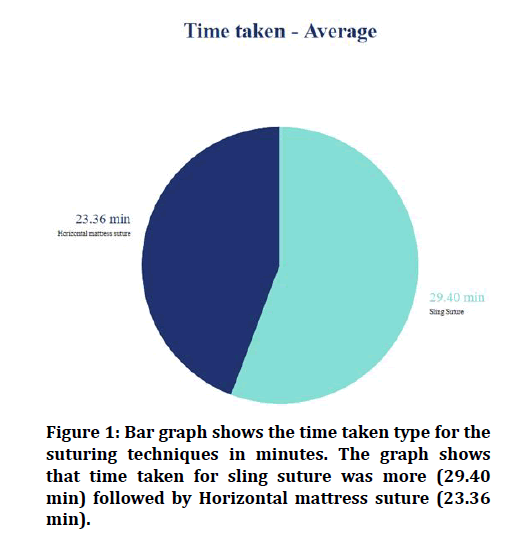
Figure 1: Bar graph shows the time taken type for the suturing techniques in minutes. The graph shows that time taken for sling suture was more (29.40 min) followed by Horizontal mattress suture (23.36 min).
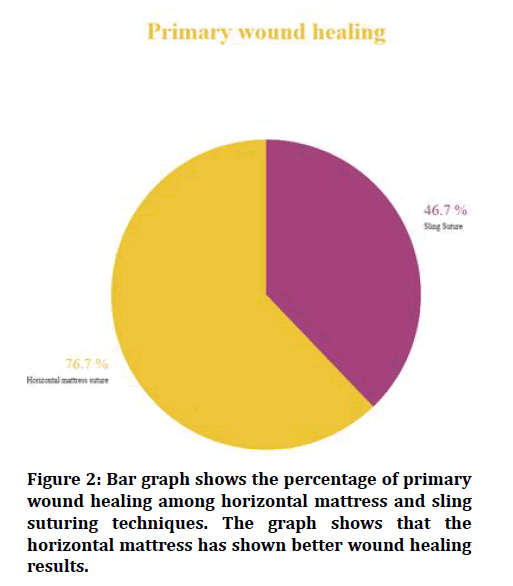
Figure 2: Bar graph shows the percentage of primary wound healing among horizontal mattress and sling suturing techniques. The graph shows that the horizontal mattress has shown better wound healing results.
The level of postoperative pain was evaluated using a 100 mm visual analogue scale (VAS) with zero (0) representing no pain and 10 excruciating pain. Following the surgeries, patients were given the VAS and told to mark their postoperative pain along the scale at 6 and 12 hours after surgery and daily thereafter for 7 days. The degree of trismus was evaluated by measuring the changes in the maximum distance between the incisal edge of the right lower and upper central incisors with a ruler before and after the surgery on the 3rd and 7th days. Postoperative swelling was evaluated by measuring the changes of the 5 distances on the face of the patients preoperatively and postoperatively. These distances were from the angle of the mandible to the lateral corner of the mouth, from the angle of the mandible to the ala of the nose, from the angle of the mandible to the lateral canthus of the eye, from the tragus to the lateral corner of the mouth, from the tragus to the ala of the nose. The first measurement was taken before the surgery and recorded as the normal value, and was then repeated on the 3rd and 7th days postoperatively. The arithmetic average of the 5 distances on the face was calculated. The swelling was then calculated as a percentage: [(postoperative values-preoperative values)/preoperative values) x 100.1 Primary wound healing was evaluated on the postoperative 7th day.
Results
This study included 30 patients, comprising 16 females and 14 males with a mean age of 23.2 ± 3.06 years (range, 20–28 years). In all patients, the alveolar bone was removed and the teeth were sectioned. The average time of the surgical procedures was 29.40 minutes for the sling suturing group and 23.36 minutes for the horizontal mattress suturing group.
No statistically significant difference was determined between the groups in respect of the relationship between the postoperative complications (P > 0.05) but the operation time was greater in the sling suture group compared to horizontal mattress group. There was an interval of 4 weeks between each surgical session. No patient complained of sensitivity loss due to damaged inferior alveolar or lingual nerves. No statistically significant difference was determined between the 2 groups in the VAS scores at 6, 12 hours and on each of the first 7 day (P>0.05). Also no statistically significant differences were determined in the trismus and postoperative swelling levels between the 2 groups at the 3rd and 7th days (P>0.05).
Primary and secondary wound healing were seen in both groups on the 7th day postoperatively. Primary wound healing was measured with a 46.7% in the sling suturing group and 76.7% for the horizontal mattress suturing group. The difference between the 2 groups was statistically significant (P:0.017).
Dehiscence is defined as a distance between the lingual and buccal mucosa. Dehiscence was measured using a Michigan O probe with Williams’s markings. PPD is defined as the distance between the gingival margin and the depth of the pocket expressed in millimetres (mm). PPD and CAL were recorded preoperatively and averagely 4 weeks postoperatively. Dehiscence was evaluated 7 and 14 days postoperatively. All assessments were made by a dental student who was blinded to the protocols done before.
The comparison of the two techniques, by taking into account the degree of impaction and PPD at the baseline, revealed that PPD at the end of 4 weeks in the horizontal mattress suture group was 1 mm deeper than that in the sling suture group (P=0.003). And the degree of impaction and CAL at the baseline, revealed that CAL at the end of 4 weeks in the horizontal mattress suture group was 0.5 mm more than that in the sling suture group (P=0.003). Measurement of dehiscence after 7 days showed that its size in the single suture technique was 0.36 mm larger than that in the horizontal mattress suture technique, and this difference was significant (P=0.059). However, this difference was not significant after 14 days.
Discussion
Third molar impaction can cause cystic and neoplastic changes, orthodontic and prosthodontics problems, and even temporomandibular joint (TMJ) symptoms [13-17]. This study compared the efficacy of single interrupted and sling sutures following third molar extraction surgery regarding postoperative sequelae wound healing, dehiscence, PPD, and CAL. This study had a split-mouth design and the same surgeon performed all surgical procedures. Thus, the effect of confounders such as age, gender, the technique of surgery, and the experience and expertise of the surgeon on the results was eliminated. Because the preoperative impaction and parameters were reported very wide range, the results and mean parameters ranged over many amounts.
In this study, we investigated whether the suturing technique has any effect on reducing the postoperative complications and especially primary wound healing after impacted mandibular third molar surgery. Following this surgery, morbidities such as trismus, swelling, pain, and delayed wound closure are severe health concerns for the patients. The duration of the surgical operation, the surgical flap design, the surgical approach, and primary wound closure may increase or decrease the postoperative complications [7,9,18]. Thus, clinicians have focussed on studies to reduce postoperative complications after impacted mandibular third molar surgery. In the literature, several applications have been reported which have aimed to improve the quality of patients’ life.
Yolcu et al. [18] evaluated postoperative swelling, trismus, pain, and primary wound healing after mandibular third molar surgery using 2 different flap techniques. They used a dental tweezers to determine the primary wound closure. Elo et al. [19] defined wound dehiscence after third molar surgery as a gap of the surgical wound edges along the sutures. In the current study, the healing process was evaluated without applying an active force. If there was a little opening along the incision, it is evaluated as a wound dehiscence. Also the photographs of the surgical areas were taken to be used for objective evaluation. Wound closure was clinically evaluated on the 7th day during suture removal; some of our patients experienced minor bleeding and suffered from pain. We believe that further studies are needed to be done to clarify the evaluation of wound closure after third molar surgery
Several suture materials such as resorb able and nonrestorable sutures can be used after third molar surgery in oral and maxillofacial clinics. In general, resorbable sutures such as vicryl are widely preferred after third molar surgery. Although silk, nonresorbable suture, is preferred for vascular hemostasis in surgical procedures, it is routinely used after third molar surgery in eastern countries [18]. Also there is no evidence on which suture material is superior to another in terms of reducing the postoperative complications of impacted third molar surgery. In our study, we used 3.0 size silk suture materials as several studies have demonstrated that it can be used after third molar surgery [20].
After fully impacted third molar surgery, surgeons try to close the surgical flap by approximation of the wound edges. Thus, the simple interrupted suturing technique is most commonly used after any oral surgical procedures, including impacted mandibular third molar surgery. However, in some patient wound eversion cannot be achieved with the simple interrupted suturing technique. In this situation, other suturing techniques such as horizontal mattress suturing can be used. This technique is also preferred for skin flap closure because it can promote wound eversion and reduce the tension across the wound edges. If there is tension between the wound edges, such as in vertical and horizontal bone grafting patients, horizontal mattress suturing can relieve the wound tension and achieve greater closure strength [21,22]. Although this is a proven suturing technique, there has been no comparison study between this technique and the sling suturing technique based on impacted mandibular third molar surgery postoperative complications.
In the literature, there is a general belief that primary wound closure increases postoperative complications [23]. Danda et al [11] compared primary and secondary wound closures after mandibular third molar surgery. Patients in the secondary wound closure group were reported to have less postoperative pain and swelling than those in the primary wound closure group. Similarly, Osunde et al [23] found that a suture-less technique showed a lower inflammatory postoperative response than a multiple suture technique after impacted mandibular third molar surgery. The reason for less postoperative pain and swelling with secondary wound closure may be the facilitation of the drainage of exudates [18]. However, in some cases such as patients on bisphosphonates or immunosuppressive drugs, or those receiving radiotherapy, primary wound healing is preferable. If primary wound healing is delayed in these patients, osteomyelitis, osteoradionecrosis, and medication-related osteonecrosis of the jaw can occur. In addition, even in systemically healthy patients, delayed wound healing can cause alveolar osteitis, food residue, and periodontal problems at the second molar tooth [18].
Another issue is how many sutures should be placed after third molar surgery. Danda et al stated that 1 suture on the distal side of the incision is more comfortable for patients when comparing 2 sutures. In our study, 1 simple sutures were placed on the distal side of the incision in group A whereas mesial side for group B. However, there is no study about how many sutures should be placed for sling and horizontal mattress suture techniques after impacted third molar surgery. More suturing can block the drainage of the hematoma and exudates. So patients with more sutures can suffer more from postoperative complications. Besides it has been shown that a gap in the vertical incision can help the drainage, and thus reduce the postoperative complications [7]. In our study, all patients had a gap in the vertical incision area.
According to our results, horizontal mattress suturing has no negative impact on postoperative trismus, pain, and swelling, and is superior to sling suturing in terms of primary wound healing. Whereas in terms of PPD and CAL sling suturing showed superior results. However there are some limitations of our study. Such a horizontal mattress suturing did not decrease the pain, swelling, and trismus level in this study, but faster primary healing established by the mattress suturing may decrease the postoperative complications. Also quantity and quality of keratinized gingiva around the third molar could not be evaluated since all the third molar teeth involved in this study were impacted. We recalled the patients on 3,7, and 30 days; however, we did not evaluate middle and longterm patients’ complaints such as food residue and periodontal problems since such complications after impacted third molar surgery are rarely seen.
Conclusion
In conclusion, horizontal mattress suturing can be used in impacted mandibular third molar surgery to improve primary wound healing and sling suture to improve PPD and CAL. Also the results of this study are useful for not only impacted mandibular third molar surgery but also other surgical procedures in oral cavity. However, we think that further studies are needed to be done on patients who have risk of postoperative osteonecrosis of impacted third molar surgery. However, the technique of suturing does not seem to have a significant long-term effect on wound dehiscence.
References
- Scherstén E, Lysell L, Rohlin M. Prevalence of impacted third molars in dental students. Swed Dent J 1989; 13:7–13.
- Rosa AL, Carneiro MG, Lavrador MA, et al. Influence of flap design on periodontal healing of second molars after extraction of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93:404–7.
- Kim K, Brar P, Jakubowski J, et al. The use of corticosteroids and nonsteroidal antiinflammatory medication for the management of pain and inflammation after third molar surgery: A review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107:630–40.
- UStün Y, Erdogan O, Esen E, et al. Comparison of the effects of 2 doses of methylprednisolone on pain, swelling, and trismus after third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96:535–9.
- Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: Postoperative complications and their risk factors. J Can Dent Assoc 2007; 73:325.
- Pourdanesh F, Esmaeelinejad M, Aghdashi F. Clinical outcomes of dental implants after use of tenting for bony augmentation: A systematic review. Br J Oral Maxillofac Surg 2017; 55:999–1007.
- Jakse N, Bankaoglu V, Wimmer G, et al. Primary wound healing after lower third molar surgery: evaluation of 2 different flap designs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93:7–12.
- Richardson DT, Dodson TB. Risk of periodontal defects after third molar surgery: An exercise in evidence-based clinical decision-making. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 100:133–7.
- Kugelberg CF, Ahlström U, Ericson S, et al. The influence of anatomical, pathophysiological and other factors on periodontal healing after impacted lower third molar surgery. A multiple regression analysis. J Clin Periodontol 1991; 18:37–43.
- Pasqualini D, Cocero N, Castella A, et al. Primary and secondary closure of the surgical wound after removal of impacted mandibular third molars: a comparative study. Int J Oral Maxillofac Surg 2005; 34:52–7.
- Bello SA, Olaitan AA, Ladeinde AL. A randomized comparison of the effect of partial and total wound closure techniques on postoperative morbidity after mandibular third molar surgery. J Oral Maxillofac Surg 2011; 69:e24–30.
- Zuhr O, Rebele SF, Thalmair T, et al. A modified suture technique for plastic periodontal and implant surgery--the double-crossed suture. Eur J Esthet Dent 2009; 4:338–47.
- Akkaya M, Böke F. Shallow localized gingival recession defects treated with modified coronally repositioned flap technique: A case series. Eur J Dent 2013; 7:368–72.
- Nemcovsky CE, Tal H, Pitaru S. Effect of non-erupted third molars on roots of approximal teeth. A radiographic, clinical and histologic study. J Oral Pathol Med 1997; 26:464–9.
- Güven O, Keskin A, Akal UK. The incidence of cysts and tumors around impacted third molars. Int J Oral Maxillofac Surg 2000; 29:131–5.
- Knutsson K, Brehmer B, Lysell L, et al. Pathoses associated with mandibular third molars subjected to removal. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 82:10–7.
- Eliasson S, Heimdahl A, Nordenram A. Pathological changes related to long-term impaction of third molars. A radiographic study. Int J Oral Maxillofac Surg 1989; 18:210–2.
- Yolcu Ü, Acar AH. Comparison of a new flap design with the routinely used triangular flap design in third molar surgery. Int J Oral Maxillofac Surg 2015; 44:1390–7.
- Elo JA, Sun HH, Dong F, et al. Novel incision design and primary flap closure reduces the incidence of alveolar osteitis and infection in impacted mandibular third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol 2016; 122:124–33.
- Koray M, Ofluoglu D, Onal EA, al. Efficacy of hyaluronic acid spray on swelling, pain, and trismus after surgical extraction of impacted mandibular third molars. Int J Oral Maxillofac Surg 2014; 43:1399–403.
- Chacon A, Shiman M, Strozier N, et al. Horizontal running mattress suture modified with intermittent simple loops. J Cutaneous Aesthetic Surg 2013; 6:54.
- Moody BR, McCarthy JE, Linder J, et al. Enhanced cosmetic outcome with running horizontal mattress sutures. Dermatol Surg 2005; 31:1313–6.
- Osunde OD, Adebola RA, Saheeb BD. A comparative study of the effect of suture-less and multiple suture techniques on inflammatory complications following third molar surgery. Int J Oral Maxillofac Surg 2012; 41:1275–9.
Author Info
Ramvihari Thota* and Senthilnathan Periasamy
Department of Oral & Maxillofacial Surgery, Saveetha Dental College, Saveetha Institute of Medical and Technical Science, Saveetha University Tamilnadu, IndiaCitation: Ramvihari Thota, Senthilnathan Periasamy,Usage of Sling Suture and Horizontal Mattress Suture Following Third Molar Surgeries, J Res Med Dent Sci, 2021, 9(8): 307-311
Received: 02-Aug-2021 Accepted: 19-Aug-2021
