Case Report - (2021) Oral and Systemic Health
Unusual presentation of Aggressive Giant cell Granuloma with non-vital tooth Case report: The importance of using CBCT in diagnosis of the non-odontogenic lesions.
Sandra H El-khatib*, Dontra B Scott and Asgeir Sigurdsson
*Correspondence: Sandra H El-khatib, Department of Endodontics, College of Dentistry New York University New York, USA, Email:
Abstract
Introduction: This case reports a Central Giant Cell Granuloma (CGCG); a lesion that is uncommon, idiopathic, and benign. However, it can be quite invasive and has reported high rate of recurrence. Its radiographic similarity to routine inflammatory peri-radicular lesions can lead to not only delay in diagnosis, but also further delay in successful treatment.
Method: a 55-year-old Caucasian man presented with tenderness on palpation of the apical area of upper canine, patient had no other symptoms. A large periapical lesion associated with the canine and first premolar was realized on a periapical radiograph. Based on radiographic signs and symptoms the patient underwent regular endodontic treatment. During the endodontic visits, there was a suspicion of a more complex diagnosis. A CBCT taken that further increased the concern about the lesion such that a biopsy was thought to be needed.
Result: Evaluation of every single detail of a radiographic image, signs and symptoms must be taken in consideration. If there is a large radiolucent lesion on the radiographic image, CBCT image should be considered, which is a very versatile tool for early diagnosis of Odontogenic and Non–Odontogenic lesions especially with cases of unusual presentation. The Diagnosis is confirmed by histological biopsy and blood tests, which are important tools to diagnose the Giant Cell Granulomas.
Conclusion: The importance of computed tomography-guided biopsy in the diagnosis of such inaccessible lesions, cone beam images help in detecting cases misdiagnosed non-odontogenic lesions from the normal digital periapical radiograph films.
Keywords
CBCT, Biopsy, Radicular cyst, Central Giant Cell Granuloma (CGCG)
Introduction
The Central Giant Cell Granuloma (CGCG) was first described by Jaffe in 1953 as a giant-cell reparative granuloma of the jaw bones. It was hypothesized that it was not a true neoplasm, but it might be the result of a local reparative reaction [1]. The central giant cell granuloma is classified as a benign non-odontogenic Multilocular radiolucency of the jaws, it may also appear as a Monocular radiolucent. Clearly, this idiopathic lesion is not derived from pulpal pathosis. But its presentation around the roots of teeth can lead to incorrect diagnosis [2-4]. The incidence of CGCG in the Netherland’s population is estimated to be 0.0001%. The survival rate after the surgical therapy and removing the lesion is 76.1% after 5 years [5]. It occurs most in young adults with a female predilection and is the most common in mandibular posterior. Giant cell reparative granuloma accounts for 17% of all benign lesions of the jaw [6].
World Health Organization defines the CGCG as a benign interosseous lesion that might be aggressive osteolytic proliferation consisting of cellular fibrous tissue and contains many foci of hemorrhage, aggregations of multinucleated giant cells, [7]. CGCG belongs to the family so-called GCLs, together with brown tumor of the hyperparathyroidism, giant cell tumor. In which is difficult to distinguish solely by microscopic examination [8]. The radiographic appearance of the CGCG may be confused with other jaw lesions. Typically, it has a well demarcated margin; can produce adjacent root divergence; create smooth, concave root resorption; and cross the midline. CGCGs are classified, according to location, as central giant cell granuloma in bone or peripheral giant cell granuloma in gingiva. The most troublesome characteristic of the CGCG is its locally aggressive destructive nature and high recurrence rate [9]. The present report illustrates a rare case of CGCG, with an atypical clinical presentation; attention has been focused on Cone Beam Computed Tomography (CBCT), guided biopsy and a surgical treatment.
Case Presentation
A 55 years old Caucasian man was referred to the post graduate endodontics clinic. The patient’s chief complaint was tenderness above the maxillary right canine on palpation. His medical history reveals type I diabetes that was well controlled, and an allergy to cats and dust. The patient’s dental history revealed no reports of previous buccal swelling, or facial pain, and he denied any history of traumatic dental injury [10-14].
On the Clinical Examination, the Extra Oral Examination revealed normal appearance with no swelling but tenderness on palpation above the upper maxillary right canine and first premolar. While the Intra Oral Examination revealed normal appearance to the oral mucosa, with no swelling and there was no pain to percussion on either tooth #5 or #6, but tenderness on palpation above the upper maxillary right canine and first premolar [15]. There was no tenderness on palpation of the adjacent palatal and buccal regions. Class V composite restorations were in place on both teeth.
The Tooth Sensibility Tests consist of two different tests: the cold test using endo ice and the analytic technology electric pulp test (EPT). All upper teeth, except the maxillary upper left first premolar #5 and canine #6 responded with in normal limits to these tests, there was no response in either of the two teeth # 5 and #6 to neither of the tests. Both teeth gave no response on cold test and EPT with reading 80. The Radiographic Findings from the periapical radiographs revealed large well-defined radiolucency of approximately 30 mm that involved both the canine and first premolar.
The Diagnosis Based on the clinical test results and periapical radiograph findings, was necrotic pulp with symptomatic periapical periodontitis for both teeth #5 and #6. The Treatment plan was Endodontic therapy for both teeth #5 and #6 was recommended.
Methods and Materials
The endodontic therapy was initiated for each tooth on separate dates. Local anesthesia used was 1.8 mL of 2% lidocaine with 1:100,000 epinephrine (Xylocaine; Dentsply, York, PA) via infiltration buccally and palatally. Rubber dam application was applied. The canine was treated first, access was opened, pulp chamber was sclerosed and no vital pulp tissue was observed (Figure 1). The working length was measured using apex locator and a periapical x-ray (Figure 2). The tooth was instrumented by rotary ProTaper files with a working length of 25.5 mm to a F2 size (Figure 3). During the following appointment the premolar was treated. Upon accessing the tooth, it was noted that the pulp chamber was sclerosed but a vital pulp tissue was detected.

Figure 1: (A and B): Microscopic pictures shows pulp chamber sclerosis in tooth #5 and #6

Figure 2: Periapical radiograph exhibited large well defined unilocular round shaped radiolucency of approximately 30 mm that involved both the canine and first premolar. The periodontal ligament space (PDL) of the canine was noted to be wide and irregular, for the first premolar it was considered to be more regular. There was no apparent displacement of the involved teeth on the periapical film and no root resorption was detected. presence of radiopacity in the crowns of both teeth.
Figure 3:X-Ray shows working length of teeth #5 and #6. Initial film with angulation shows large unilocular radiolucent lesion associated with tooth #5,#6 expanded to tooth no.#4
This indicated a possible misdiagnosis for the premolar. The premolar was instrumented by rotary ProTaper files to a working length of 20.5 mm for palatal root and 20 mm for buccal root to a F1 size (Figure 4). Irrigation used for both teeth was sodium hypochlorite, EDTA, chlorohexidine and calcium hydroxide intracanal medicament was placed for 1 week. Obturation was completed using thermal vertical condensation technique and AH plus sealer (Figure 5).
Figure 4: Master cone x-ray of teeth #5 and #6 before obturation
Figure 5: x-ray shows obturation of teeth #5 and #6. post-operative film with parallel technique shows the extension of the lesion.
After the second endodontic visit, it was decided to investigate the periapical lesion further with a limited field of view cone beam exposure. This adjunctive treatment was recommended because of the fact that the premolar had vital tissue present. Also, because it was noted at the second visit for the canine that the anesthetic needle passed easily into a lumen, indicating a very minimal cortical bone coverage facial to the radiographic radiolucency. In addition to the extent of the radiolucent lesion on the periapical radiograph was of concern and therefore a CBCT image would help elucidate the exact size of the lesion [16].
Cone beam computed tomography radiograph Imaging findings:
There was a well-defined, non-corticated, unilocular radiolucency of the anterior right maxilla. The radiolucency extended anteriorly to the maxillary right lateral incisor, posteriorly to the maxillary right second premolar, and superiorly through the floor of the right nasal cavity and the antero-medial wall of the right maxillary sinus. The palatal cortex was noted to be thinned (Figure 6). The buccal cortex overlying the canine –first premolar region was thinned and expanded, and notably the expansion flowed over normal bone in the superior area (Figure 7).
Figure 6: Reconstruction view of cone beam Panoramic reconstruction of the 40 x 40 mm cone beam CT study of the anterior right maxilla shows the well-defined, non-corticated, unilocular radiolucency extending from the maxillary right second premolar anteriorly to the maxillary right canine region. The radiolucency has perforated the anteromedial wall of the right maxillary sinus and extended into the sinus cavity.
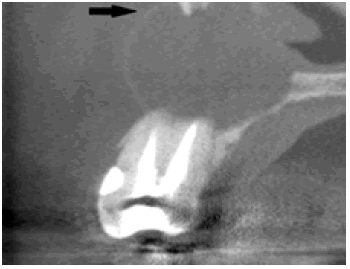
Figure 7: Bucco-palatal image of the cone beam CT study shows the well-defined, non-corticated, unilocular radiolucency has expanded and perforated the labial cortex, overflowing onto adjacent, intact, normal bone. The overflow feature (arrow) is the second key finding that is not consistent with the pathophysiology of radicular cysts.
Imaging impression: The findings of the anterior right maxilla were considered to be consistent with benign developmental cystic process, favoring unicystic ameloblastoma over keratocystic odontogenic tumor (odontogenic keratocyst) and biopsy was advised (Figure 8).
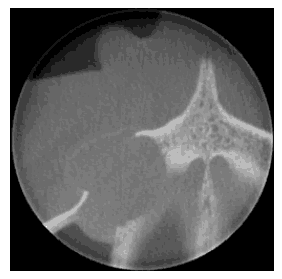
Figure 8: Axial image of the cone beam CT study shows the well-defined, non-corticated, unilocular radiolucency of the anterior right maxilla lacking the balloon-like, hydraulic expansion associated with radicular cysts.
Surgical treatment
Patient presented to the post graduate endodontic clinic for incisional biopsy of the lesion that was identified via the cone beam imaging. The surgical procedure, risk and benefits associated with the procedure were reviewed with the patient and consent was obtained. All procedures were performed by an endodontic post graduate resident (DS) under local anesthesia [17]. Infiltration buccally over the apices of the teeth to be treated and the adjacent teeth was undertaken using 1.8 mL of 2% lidocaine with 1:50,000 epinephrine (Xylocaine; Dentsply, York, PA) followed by infiltration buccally and palatally with 3 mL of 2% lidocaine containing 1:100,000 epinephrine (X) to involve the entire surgical site. With the exception of incisions, flap elevation, and suturing, all surgical procedures were performed with an Operating Microscope (OPMI PICO; Carl Zeiss, Göttingen, Germany).
A vertical incision was performed with a #15 scalpel blade and a triangular full thickness flap was raised following an intrasulcular incision. The tissue was gently reflected toward the apical area with a Molten 2– 4 curettes (G Hartzell and Son Inc, Concord, CA). The tissues exposed by the reflection of the flap were kept moistened with sterile saline throughout the surgery to avoid the bone or the soft-tissue flap from drying out. Upon reflection the extent of the lesion was noted [18,19]. Complete perforation of the buccal cortex was observed, Figure (5). A well-defined irregular shaped dark tan brown 3cm × 4cm non-pulsating lesion extending from the apex of tooth #4 to the apical region of tooth #6 was noted. The lesion had embedded itself in the mucoperiosteum and required careful separation.
A small incisional biopsy was performed using a #15 scalpel blade to remove a 1cm × 1cm section of the lesion to submit for histological examination. Tissues were approximated and adapted using 6-0 Vicryl interrupted and sling sutures. Firm pressure was applied to the tissues with a gauze swab dampened with sterile saline for 5 to 10 minutes to ensure close adaptation of the soft tissue to the remaining bone. Post-operative written and verbal instructions were given. Patient was advised to take analgesics (ibuprofen 400 mg every six hours or paracetamol 500 mg every six hours) as required (Figure 9).
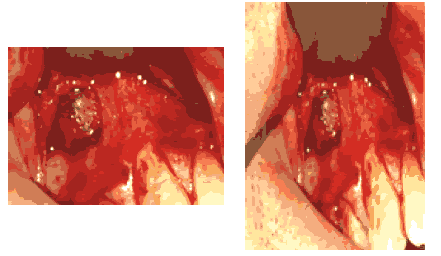
Figure 9: Picture after reflecting the soft tissue for biopsy, shows complete perforation of the buccal cortex with a well-defined irregular shaped dark tan brown 3cm x 4cm non-pulsating lesion extending from the apex of tooth #4 to the apical region of tooth #6 was noted. The lesion had embedded itself in the mucoperiosteum and required careful separation.
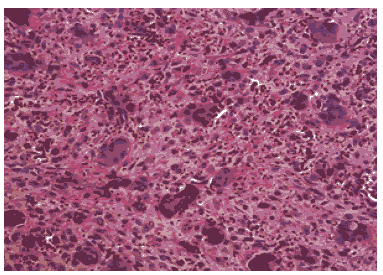
Figure 10: The Microscopic description showed a portion of soft tissue composed of cellular fibrous connective tissue with abundant diffusely scattered multi-nucleated giant cells extravagated red blood cells are seen in background. Residual and Reactive bone are also seen. Differential Diagnosis was given wither its Brown Tumor Disease or Central Giant Cell Granuloma as they have the same Microscopic Histology Appearance.
The Gross pathology of the biopsy described an irregular shaped rough-surfaced portion of firm, dark tan and brown tissue. The microscopic description showed a portion of soft tissue composed of cellular fibrous connective tissue with abundant diffusely scattered multi-nucleated giant cells. Extravagated red blood cells were seen in background [20,21]. Residual and reactive bone was also seen (Figure 10). A Differential diagnosed was given either Central giant cell granuloma or brown tumor of hyperthyroidism. Patient was referred to the oral surgery department for further evaluation and possible sectional surgery, where the total lesion would be removed. Laboratory Blood tests were requested for differentiation between CGCG and brown tumor lesions (Figure 11).
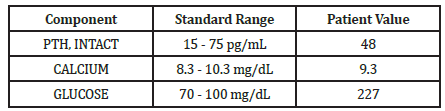
Figure 11: The above table of Blood Test Result shows normal Calcium level in patient’s blood and does not shows Hyperthyroidism which exclude Brown Tumor Disease and proves its Central Giant Cell Granuloma.
Discussion
In the present report, we describe a rare case of CGCG developing close to non-vital tooth maxilla canine without any history of pain or facial swelling. In contrast to radicular cyst, CGCG is non-odontogenic bone lesion, that looks similar to radicular cyst in radiographic examination, but on a cone beam image it shows the difference in expansion, destruction, and invasion. The radiologic features of CGCG have not been clearly defined, and there are many of conflicting descriptions in the literature (2,10). The CGCG usually demonstrates radiographic and clinical features of a benign lesion with some aggressive characteristics.
The Cone Beam Computed Tomography (CBCT) is an extra-oral imaging system which was developed in the late 1990s. It produces 3-D scans of the maxillo- facial skeleton at a lower radiation dose than more traditional CT. A CBCT scan should be considered after a comprehensive clinical examination and after periapical 2-D radiographic evaluation [12-13]. In our presented case, there was a debate whether to do a cone beam or not and whether to harvest a biopsy or not. Initially it was believed that the lesion was of odontogenic origin and associated with non-vital tooth (endodontic lesion) and therefore no need to expose the patient for the radiation, and more cost.
As a CBCT scan should only be considered if an additional information from the 3-D images will aid in the diagnosis [14]. It has shown that CBCT has significantly higher diagnostic accuracy in detecting periapical periodontitis compared to periapical 2D radiograph, using human histopathological findings as a reference standard [15]. Additionally, up 38% more periapical lesions were detected with CBCT compared with periapical radiographs [16] and CBCT has twice the odds of detecting a periapical lesion than with conventional radiographs [17]. It has been suggested that CBCT aids in diagnosis of nonodontogenic lesions such as CGCG (14) and it can also aid in management of CGCG. As CBCT is needed for the Pre-surgical assessment prior to complex peri-radicular surgery, and to identify which treatment is preferred for management of the CGCG depending on the aggressiveness of the CGCG lesion [14,16].
After assessment of the CBCT image and identifying the aggressiveness, its deep extent, and its close relationship to the surroundings anatomical structures, it has been decided that only an excisional biopsy will be done in the endodontic department, and then depending on the histological findings the patient would be referred to the oral maxilla-facial department for complete surgical excision and management if needed. CGCG has various histopathological differential diagnosis includes: Brown Tumour of hyperparathyroidism, PGCG, Cherubism, GCT, Aneurysmal bone cyst and Fibrous dysplasia [2]. In our microscopic histological investigation taken from the biopsy, we could not identify the diagnosis if it is a CGCG or a brown tumor of hyperparathyroidism. They have the similar microscopic histological picture, and our case was presenting similar clinical features. The only way to differentiate between the two, is by the laboratory blood tests. The brown tumor associated with hyperthyroidism has increase of calcium in the blood. So, the laboratory tests were requested, and the diagnosis was confirmed to be a CGCG lesion. That diagnosis was made due to absence of increase of the calcium in the patient blood laboratory test.
Several alternative treatments have been suggested in the literature, including interferon alpha-2a, calcitonin and intra-lesional corticosteroid injection. Surgical methods that have been described for removal of aggressive CGCRGs, include curettage and cryosurgery, curettage and peripheral osteotomy, excision and followed by reconstruction by using an autologous iliac crest bone graft [7,18]. The traditional therapy of CGCRG has been surgical local curettage, and this has been reported with a high success rate or about 76.1% - 80% [5,]). Non-surgical treatment of CGCRG has though been suggested as a good treatment option for small, slowly, enlarging lesions [7,19,20]. Successful treatment of painful, large, and rapidly growing lesions is more likely achieved by surgical removal. Many authors do agree that a correct diagnosis and complete surgical excision with curettage is effective in complete resolution of the CGCG lesions [5,7,20,21].
This case report had a misleading diagnosis at the beginning between the odontogenic endodontic diagnosis and non- odontogenic CGCG diagnosis, due to presence of endodontic signs and symptoms associated with a necrotic tooth, periapical radiolucent and tenderness on palpation. It is not possible to state if the non-odontogenic CGCG lesion origin in our case was associated by the endodontic infection or it just occurred by chance at the same time [22], or if the CGCG lesion caused the pulpal necrosis in the canine due to the extent and aggressiveness of the CGCG lesion, that caused excessive pressure on the neurovascular bundle to the tooth.
The CGCG is a rare lesion, that has high incidence of misdiagnoses with other lesions, which complicates the fact that the early detection of CGCG gives much better prognosis. This is due to its aggressiveness and has chance to turn into malignant lesion if left for long time. There is a high incidence of the CGCGs clinicopathologic features associated with necrotic teeth or teeth that had received previous root canal treatment. This incidence is 20% of CGCG were associated with necrotic teeth and 88% were associated with previous endodontic treatment [22]. Though it is not clear if the CGCG is responsible for the need for endodontic treatment or if the presence of the lesion was misdiagnosed as a periapical lesion of endodontic origin. In this case report, the endodontic misdiagnosis was at the beginning of the treatment until further investigation and CBCT were requested due to the large size of the periapical radiolucency and the fact a vital pulp tissue was encountered in the premolar. Nowadays, the advance technology of CBCT allowed more image accuracy, 3-D anatomic details and low dose exposure [12-17]. It is recommended and emphasized for CBCT consideration in case of large periapical radiolucency, to include the CGCGs in the differential diagnosis to the endodontic treatment. CGCGs malignant transformation is rare but might occur if left untreated. An early diagnosis of CGCGs is therefore crucial to avoid serious complications [22-24].
The patient in this case report had an aggressive variant of CGCG: The lesion was larger than 5 cm, the cortical bone erosion was demonstrated by CBCT examination. It was fast growing and the extent and aggressiveness of the lesion anterior- posterior and mesiodistal, which made conventional conservative surgical treatment (curettage) unfeasible. Therefore, the patient was referred to the oral-maxilla facial department for complete sectional excision. This case shows also that even aggressive variants of CGCG do not always fulfill all the criteria for diagnosis of aggressive one, because in this case it was asymptomatic, there was no swelling, no tooth displacement or root resorption [2,6,8,9]. It is worth noting that there is no histological differences between the aggressive and non-aggressive varieties. Literatures have agreed upon using their clinical behavior to mark their aggressiveness progression.
Conclusion
CGCG is a bony lesion that can be misdiagnosed as an apical lesion of endodontic origin. The current case report presents a case of unusual presentation of a CGCG. The CGCG lesion was associated with nonvital tooth, and the correct extent of the lesion was not appreciated until a CBCT examination was done. The suggested way for differentiation is by using CBCT and surgical biopsy after full evaluation of clinical examination and endodontic tests. Early accurate diagnosis of CGCG is crucial, to avoid serious complications and malignant transformation.
Acknowledgement
The author thank KC Chan, DMD, MS,Diplomate, ABOMP, ABOMR,Director, Oral and Maxillofacial Radiology.
Sonal S Shan, DDS pathologist.
Hatem Amer Oral and Maxillofacial pathologist Cairo University.
Consent for Publication
The authors used non identifiable photographs and no identifying details were mentioned in the report.
Conflict of Interest
The authors have disclosed no potential conflicts.
References
- Jaffe HL. Giant-cell reparative granuloma, traumatic bone cyst, and fibrous (fibro-osseous) dysplasia of the jawbones. Oral Surgery. 1953; 6:159-175.
- Ehtisham M, Kaur P, Nissar S, et al. Central giant cell gran- uloma: uncommon yet important. journal of dental and medical sciences 2016; 15:74-80.
- Jadu FM, Pharoah MJ, Lee L, et al. Central giant cell granulo- ma of the mandibular condyle: a case report and review of the literature. Dentomaxillofac Radiol 2011; 40:60-4.
- Barnes L, Eveson JW, Sidransky D, et al. Pathology and ge- netics of head and neck tumours IARC 2005.
- de Lange J, van den Akker HP, Klip H. Incidence and dis- ease-free survival after surgical therapy of central giant cell granulomas of the jaw in The Netherlands: 1990–1995. Head & Neck: Journal for the Sciences and Specialties of the Head and Neck 2004; 26:792-795.
- Jundt G, Barnes L, Eveson JW, et al. World health organi- zation classification of tumours pathology and genetics of head and neck tumours. Lyon: IARC Press 2005: 324.
- Schütz P, El-Bassuoni KH, Munish J, et al. Aggressive central giant cell granuloma of the mandible. J of Oral Maxillofacial Surgery. 2010; 68:2537-44.
- Eisenbud L, Stern M, Rothberg M, et al. Central giant cell granuloma of the jaws: experiences in the management of thirty-seven cases. J Oral Maxillofac Surg. 1988; 46:376- 384.
- Chuong R, Kaban LB, Kozakewich H, et al. Central giant cell lesions of the jaws: a clinicopathologic study. J Oral Maxil- lofac Surg 1986; 44:708-13.
- Kaffe I, Ardekian L, Taicher S, et al. Radiologic features of central giant cell granuloma of the jaws. Oral Surgery. 1996; 81:720-6.
- Stavropoulos F, Katz J. Central giant cell granulomas: a sys- tematic review of the radiographic characteristics with the addition of 20 new cases. Dentomaxillofac Radiol. 2002; 31:213-7.
- Patel S, Dawood A, Whaites E. New dimensions in end- odontic imaging: part 1. Conventional and alternative ra- diographic systems. Int endod J. 2009; 42:447-62.
- Patel S. New dimensions in endodontic imaging: Part 2. Cone beam computed tomography. Int endod J. 2009; 42:463-75.
- Patel S, Durack C, Abella F, et al. European Society of Endodontology position statement: the use of CBCT in end- odontics. Int Endod J. 2014; 47:502-504.
- Kanagasingam S, Lim CX, Yong CP, et al. Diagnostic accu- racy of periapical radiography and cone beam computed tomography in detecting apical periodontitis using histo- pathological findings as a reference standard. Int Endod J 2017; 50:417-26.
- Patel S, Durack C, Abella F, et al. Cone beam computed tomography in e ndodontics–a review. Int Endod J 2015; 48:3-15.
- Aminoshariae A, Kulild JC, Syed A. Cone-beam computed tomography compared with intraoral radiographic lesions in endodontic outcome studies: a systematic review. J En- dod 2018 Nov; 44:1626-31.
- de Lourdes Suárez-Roa M, Reveiz L, Rivera LM, et al. In- terventions for central giant cell granuloma (CGCG) of the jaws. Cochrane Database Syst Rev 2009.
- De Lange J, Van den Akker HP, Van den Berg H, et al. Limit- ed regression of central giant cell granuloma by interferon alpha after failed calcitonin therapy: a report of 2 cases. Int J Oral Maxillofac Surg 2006; 35:865-9.
- Triantafillidou K, Venetis G, Karakinaris G, et al. Central gi- ant cell granuloma of the jaws: a clinical study of 17 cases and a review of the literature. Ann Otol Rhinol Laryngol 2011; 120:167-74.
- Tosco P, Tanteri G, Iaquinta C, et al. Surgical treatment and reconstruction for central giant cell granuloma of the jaws: a review of 18 cases. J Craniomaxillofac Surg 2009; 37:380- 387.
- Dahlkemper P, Wolcott JF, Pringle GA, et al. Periapical cen- tral giant cell granuloma: a potential endodontic misdiag- nosis. Oral Surgery 2000; 90:739-745.
- Lombardi T, Bischof M, Nedir R, et al. Periapical central gi- ant cell granuloma misdiagnosed as odontogenic cyst. Int Endod J 2006; 39:510-515.
- Lanza A, Laino L, Rossiello L, et al. Clinical practice: Giant cell tumour of the jaw mimicking bone malignancy on three-dimensional computed tomography (3D CT) recon- struction. Open Dent J 2008; 2:73-77.
Author Info
Sandra H El-khatib*, Dontra B Scott and Asgeir Sigurdsson
1Department of Endodontics, College of Dentistry New York University New York, USACitation: Sandra H. El-khatib, Dontra B. Scott, Asgeir Sigurdsson, Unusual presentation of Aggressive Giant cell Granuloma with non-vital tooth Case report:The importance of using CBCT in diagnosis of the non-odontogenic lesions, J ResMedDentSci,2021,9(S1):50-57.
Received: 14-Apr-2021 Accepted: 21-Apr-2021 Published: 10-May-2021
Sources of funding : GB´s PhD-project on ethical challenges and decision-making in nursing homes has been financially supported by the Norwegian Extra Foundation for Health and Rehabilitation through EXTRA funds (grant no. 2008/2/0208).
