Research - (2021) Volume 9, Issue 5
Ultrasound and Magnetic Resonance Imaging Correlation of Adnexal Lesions
*Correspondence: Ravindran C, Department of Radio diagnosis, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
To evaluate accuracy of ultrasound and magnetic resonance imaging in characterizing adnexal lesions. To determine which patients may benefit from magnetic resonance imaging.
Keywords
Ultrasound, Adnexal lesions, Benign lesions, Surgery
Introduction
Adnexal lesions are a common clinical problem, a common cause for morbidity and mortality in female population. An estimated 5 - 10% of women undergo surgery for suspicious adnexal lesions, less than 25% of which prove to be malignant. The surgery for a benign lesion is a simple excision, but for malignant adnexal lesion radical surgery is performed. Since there is a considerable difference between these two types of surgeries, it is important to differentiate malignant and benign diagnoses to direct patients to the appropriate treatment algorithm. The benign or malignant nature of a clinically diagnosed adnexal lesion is frequently not evident before surgical exploration and histological examination. A reliable method to differentiate benign from malignant adnexal lesions would allow for appropriate subspeciality referral, optimal preoperative planning, and counselling of the patient [1].
Ultrasonography (US) is the accepted primary imaging technique for evaluating adnexal lesions because of its widespread availability, relatively low cost and high sensitivity in the detection of lesions. Many women need no other imaging if the lesion has features indicating that it is clearly benign. However, sonography is limited by its decreased specificity for diagnosis of benignity [2-5].
Magnetic resonance imaging (MRI) has been shown to have potential for tissue characterization of adnexal lesions, and contrastenhanced MRI has been reported to be more accurate than US for assessing them [6].
Materials and Methods
Source of data
A prospective study was performed with 40 women between October 2014 and September 2016 (period of 2 years) who were referred to our hospital with clinically suspected adnexal lesion. Informed consent was taken from each patient and they were instructed to be on fasting for at least 4-6 hours before the scan time. Each patient underwent ultrasound examination, followed by MRI within a period of 1 week. These participants had a laparotomy whenever indicated and based on the surgical and/ or pathological findings were categorized as having benign or malignant lesions. Lesions with absolute benign nature were followed up for results.
Inclusion criteria
99 Patients with clinically suspected ultrasound detected adnexal lesion.
99 Age group between 14 to 70 years.
99 Patients willing to undergo this study.
99 Patients willing to undergo surgery for biopsy /FNAC.
Exclusion criteria
99 Any absolute contraindication for MRI like metal implants/ ferromagnetic substance in the body.
99 Deranged renal function test.
99 Patients who refused MRI examination.
99 Pregnant women.
Method of collection of data
Detailed clinical history and consent were taken from patients or their attenders. Ultrasound of pelvis was performed on every patient on Seimens Acuson 2000 ultrasound machine. Transvaginal scan was performed whenever required. The US images were evaluated prospectively without knowledge of the serum tumour marker, CA- 125, or MR findings. For each participant, the presence of ascites and lymphadenopathy was documented on the TAS examination. The lesions were measured, and each lesion was categorized as solid, solid-cystic or cystic. For cystic lesions wall thickness and regularity, the presence of soft tissue nodules and septa were documented. On Doppler examination, the presence of vascularity in lesions was noted. Following US examination, a subjective assessment was made as to whether each lesion was malignant or benign.
Statistical analysis
The US and MRI characterization of the subjects was compared with the final diagnosis. Data were analyzed with student t test/z test. Chi square test was adopted (with the Yates correction as appropriate) for categorical variables. Descriptive statistical values including sensitivity, specificity, and positive and negative predicative values were determined.
Results
The US and MRI characterization of the subjects was compared with the final diagnosis. Data were analyzed with student t test/ z test. Chi square test was adopted (with the Yates correction as appropriate) for categorical variables. Descriptive statistical values including sensitivity, specificity, and positive and negative predicative values were determined.
Study design
A correlative study with 40 patients to study the role of ultrasound and magnetic resonance imaging in adnexal lesions and to correlate their findings. Table 1: Age distribution of the patients is mentioned in table 1.
| Age in years | Number | % |
|---|---|---|
| 14-20 | 3 | 7.5 |
| 21-30 | 1 | 35 |
| 31-40 | 7 | 17.5 |
| 41-50 | 9 | 22.5 |
| 51-60 | 3 | 7.5 |
| 61-70 | 4 | 10 |
| Mean +/-SD | 37.8+/-14.5 | |
Table 1: Age distribution of the patients.
Figure 2 represents the T2WI - sagittal and axial images show a well-defined thin-walled fluid attenuating lesion in the pelvis. Patients’ complaints are mentioned in Table 2.
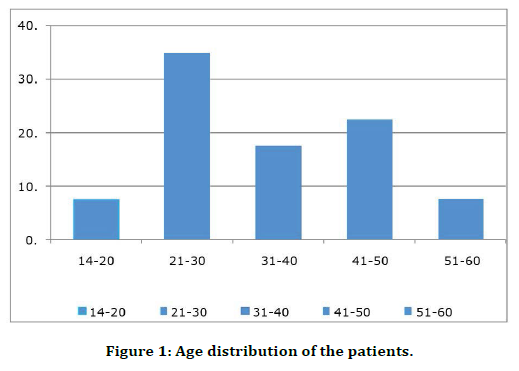
Figure 1. Age distribution of the patients.
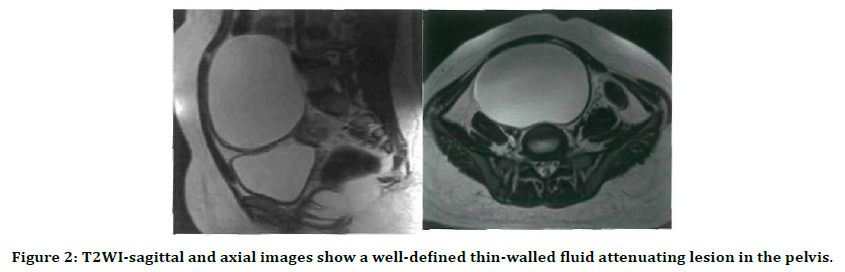
Figure 2. T2WI-sagittal and axial images show a well-defined thin-walled fluid attenuating lesion in the pelvis.
| Presenting complaints | Number (n=40) | % |
|---|---|---|
| Pain abdomen | 26 | 65 |
| Abdominal distension | 5 | 12.5 |
| Irregular menstruation | 3 | 7.5 |
| Mass per abdomen | 5 | 12.5 |
| Abdominal discomfort | 1 | 2.5 |
Table 2: Chief presenting complaints of the patients.
USG images show a well-defined predominantly solid lesion with central areas of an echogenicity (cystic component). Colour Doppler images show minimal vascularity in the solid component of the lesion (Figure 3).
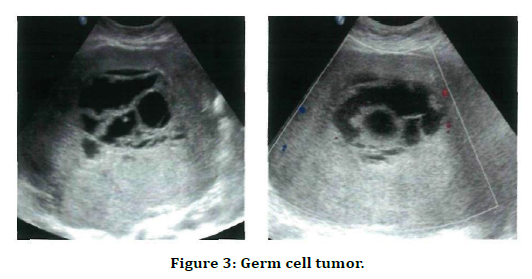
Figure 3. Germ cell tumor.
Coronal T2 W and Tl W post contrast images show a well-defined predominantly solid with cystic component lesion in the pelvis with solid component of the lesion showing minimal enhancement on contrast study (Figure 4). Maximum cases diagnosed by MRI were benign lesions (Table 3). In 28 (70%), both USG and MRI gave same diagnosis. However, 12 cases had controversies between the characterization of the lesion. (Table 4 and Figure 5).
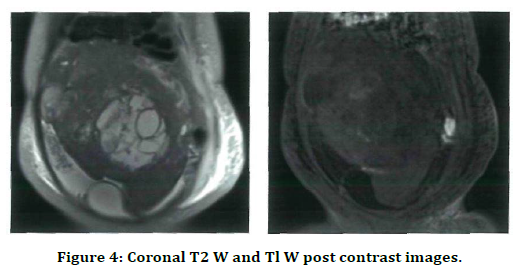
Figure 4. Coronal T2 W and Tl W post contrast images.
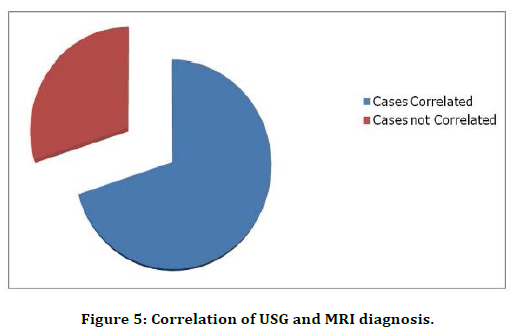
Figure 5. Correlation of USG and MRI diagnosis.
| MRI diagnosis | Number (n=40) | % |
|---|---|---|
| Serous cystadenoma | 8 | 20 |
| Mucinous cystadenoma | 3 | 7.5 |
| Serous cystadenocarcinoma | 3 | 7.5 |
| Mucinous cystadenocarcinoma | 2 | 5 |
| Other carcinoma | 3 | 7.5 |
| Germ cell tumor | 2 | 5 |
| Dermoid cyst | 1 | 2.5 |
| Subserosal fibroid | 3 | 7.5 |
| Hemorrhagic cyst | 2 | 5 |
| Hydro/hematosalpinx | 2 | 5 |
| Polycystic ovaries | 2 | 5 |
| Tubo-ovarian abscess | 4 | 10 |
| Peritoneal inclusion cyst | 1 | 2.5 |
| Simple ovarian cyst | 3 | 7.5 |
| Endometriosis | 1 | 2.5 |
| Indeterminate | 0 | 0 |
Table 3: MRI diagnosis.
| Correlation | Number | % |
|---|---|---|
| Cases correlated | 28 | 70 |
| Cases not correlated | 12 | 30 |
Table 4: Correlation of USG and MRI diagnosis.
USG image shows multiple ovarian follicles arranged peripherally. T2W MRI images in axial and sagittal planes show mildly bulky ovary with multiple peripherally arranged hyperintense follicles (Figure 6A and 6B).
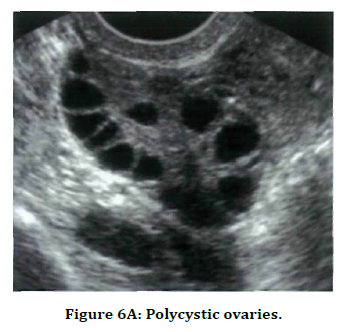
Figure 6A. Polycystic ovaries.
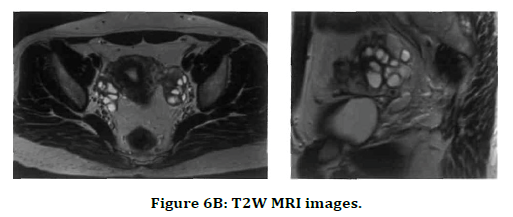
Figure 6B. T2W MRI images.
Out of 40 cases, there were 7(17.5%) indeterminate cases, out of which MRI could solve all cases. However, one case was misdiagnosed by MRI. USG called 6 (15%) lesions as malignant whereas, MRI could diagnose 8 (20%) lesions as malignant. On both modalities, one malignant case was misdiagnosed as benign. This study comprised of a greater number of benign cases than malignant tumors (Table 5 and Figure 7).
| Diagnosis | Number (N=40) | % |
|---|---|---|
| Benign | 31 | 77.5 |
| Malignant | 9 | 22.5 |
Table 5: Number of malignant lesions Vs. benign lesions.
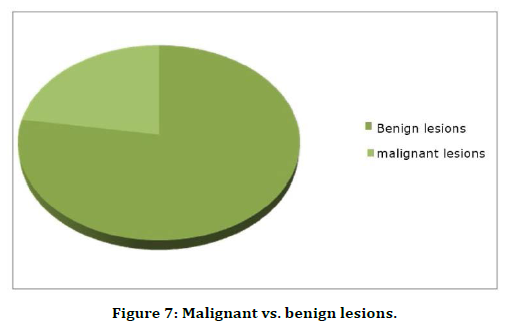
Figure 7. Malignant vs. benign lesions.
MRI has better sensitivity, specificity and accuracy in diagnosing overall adnexal lesions. However, it is more significantly sensitive and specific in the diagnosis of malignant lesions (Table 6 and Table 7), (Figure 8 and Figure 9).
| USG Diagnosis | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) |
|---|---|---|---|---|---|
| Benign lesions | 96.7 | 55.5 | 88.2 | 83.3 | 87.5 |
| Malignant lesions | 55.5 | 96.7 | 83.3 | 88.2 | 87.5 |
Table 6: Sensitivity and specificity of USG diagnosis.
| MRI Diagnosis | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) |
|---|---|---|---|---|---|
| Benign lesions | 100 | 88.8 | 96 | 100 | 97 |
| Malignant lesions | 88.8 | 100 | 100 | 96 | 97 |
Table 7: Sensitivity and specificity of MRI diagnosis.
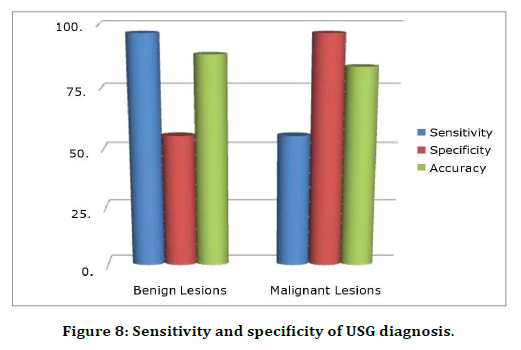
Figure 8. Sensitivity and specificity of USG diagnosis.
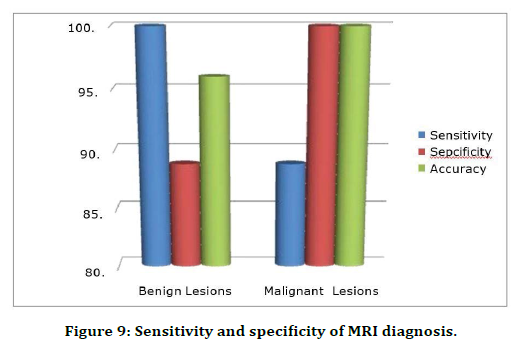
Figure 9. Sensitivity and specificity of MRI diagnosis.
Discussion
A prospective study was performed with 40 females who presented with clinically suspected adnexal lesions. Evaluation of adnexa has evolved significantly in past decade due to application and advancement of ultrasound and magnetic resonance imaging. The current study evaluated the role of ultrasound and magnetic resonance imaging in adnexal lesions [9]. Accuracy and effectiveness of both modalities in characterising the adnexal lesions were correlated and compared. This study comprised of females between 14 to 70 years with mean age of 37.5 years. Most of the patients were in reproductive age.
In present study, all the 40 patients underwent Transabdominal ultrasound and Transvaginal ultrasound was performed wherever applicable. MRI was performed on all patients and diagnosis of both USG and MRI was compared with the results that included histopathology, operative findings or through follow up.
Most common presenting complaints in patients in current study was abdominal pain predominantly confined to lower abdomen, which comprised of 26 of 40 cases (65%). This is like the study where abdominal pain was the most common presenting symptoms [10]. This was followed by abdominal distension and mass per abdomen (5 cases each). Another study also gave similar results [11].
The most common subtype of ovarian neoplasm is derived from the epithelial lining cells of the ovary. Ovarian epithelial ovarian neoplasms comprise approximately 60% of all ovarian tumors and more than 85% to 90% of ovarian malignancies [12-16].
More number of benign than malignant lesions were detected in this study. Of the benign lesions, most common lesion was serous cystadenoma of ovary (n=8) which were easily diagnosed by both ultrasound and MRI. Next common benign cystic lesion diagnosed was mucinous cystadenoma of ovary (n=3) which were also diagnosed by using ultrasound as well as MRI because of its internal echoes and Tl hyperintensity.
Two cases of serous cystadenocarcinoma were wrongly diagnosed as benign serous cystadenomas on USG. However, on MRI, the lesions were categorised as malignancy. USG also missed a diagnosis of mucinous cystadenocarcinoma and labelled it benign. MRI however, recognised the malignant nature of the lesion.
Among the malignant lesions, USG was able to pick one case of serous cystadenocarcinoma and another case of mucinous cystadenocarcinoma correctly because of its solid component which were showing vascularity [17]. There was also associated ascites in case of serous cystadenocarcinoma.
USG also picked up 2 cases of solid malignant lesions of the ovaries which were correlated with similar features on MRI. On USG a case of carcinoma cervix with parametrial extension was diagnosed as ovarian pathology. MRI in this case was able to tell the origin of the lesion.
A case of benign germ cell tumor was called as malignancy on USG because of its large size and solid- cystic component and associated minimal free pelvic fluid [18]. However, MRI could suggest its benign nature due to well defined margins and no evidence of adjacent organ invasion.
This study has one case of dermoid cyst which was diagnosed correctly by both USG and MRI because of its solid cystic nature and hyperechoic fat content. On fat-sat MRI, presence of fat was confirmed.
3 cases of subserosal fibroids are present in this study, out of which only two were diagnosed by USG and confirmed by MRI. One case of subserosal fibroid was mistaken as a solid ovarian lesion, in which MRI was the problem-solving tool in recognising organ of origin [19,20]. This was similar to study carried out by Fleischer, et al. where MRI was more accurate than USG [21].
One case of vaginal hypoplasia with hematosalpinx was diagnosed in this study. USG could delineate the dilated fallopian tubes and recognise few echoes within. However, MRI could characterise the hematosalpinx as well as recognise the cause as vaginal hypoplasia. However, another case of hydrosalpinx was not picked up by USG which was delineated on MRI.
There are three cases of tubo-ovarian abscess in this study out of which two were correctly diagnosed as tubo- ovarian origin on both USG and MRI. One was mistaken as just ovarian origin in which case MRI was helpful. However, one case was wrongly diagnosed as tubo-ovarian origin on both USG and MRI because of associated psoas abscess, but on histopathology turned out to be ovarian carcinoma.
One case of peritoneal inclusion cyst was recognised on both USG and MRI and its benign nature was identified with no obvious difficulty. There were 7 (17.5%) cases in the study in which USG could not conclude any specific diagnosis. This was like study conducted by Schwartz et al. [22] where they had 26% doubtful cases. There was also confusion regarding the benignity of the lesions. In such cases MRI played a problemsolving role. One was diagnosed as subserosal fibroid, one as tubo-ovarian abscess, one as endometriosis, one as dilated fallopian tube, one as hemorrhagic cyst and the last as malignant neoplasm of ovary.
References
- Sohaib SA. The role of MRI and ultrasound in patients with adnexal masses. Clin Radiol 2005; 60:340-348.
- Cambell S, Newman GB. Growth of fetal biparietal diameter during normal pregnancy. J Obstet Gynaecol Brit Cwelth 1971; 78:513-519.
- Curry TS, Dowdey JE, Murry RC. Christenses physics of diagnostics radiology. Lea Febiger, 4th edition, 1990.
- Bloch F, Hasen W.W, Packward ME, Nuclear Induction, Phys Rev 1946; 69:127.
- Hawkes RC, Holland GN, Moore WS, et al. Nuclear magnetic resonance (NMR) tomography of the brain: A preliminary clinical assessment with demonstration of pathology. J Computer Assisted Tomography 1980; 4:577-586.
- Rumack CM, Wilson SR. Diagnostic ultrasound, 4th edition, p556 -598.
- Vilaro MM, Rifkin MD, Pennell RG, et al. Endovaginal ultrasound. A technique for evaluation of nonfollicular pelvic masses. J Ultrasound Med 1987; 6:697-701.
- Neeharika C, Ravindran C. Ultrasound and magnetic resonance imaging correlation of adnexallesions. Annals Romanian Society Cell Biol 2021; 3404-3418.
- Levine D. Pelvic doppler seminars in ultrasound, CT and MRI. 1999; 20:239-249.
- Long MG, Boultbee J, Begent RH, et al. Doppler ultrasound of the uterine artery and uterus in invasive mole and choriocarcinoma. Br J Radiol 1987; 60:621.
- Adusumilli S, Hussain HK. MRI of sonologically indeterminate adnexal masses. AJR 2006; 87:732 -740.
- Outwater EK, Sieeelman ES, Chiowanich P, et al. Dilated fallopian tubes: MR imaging characteristics. Radiology 1998; 208:463-469.
- Ha HK, Lim GY, Cha ES, et al. MR imaging of tubo ovarian abscess. Acta Radiol 1995; 36:510 -514.
- Noone TC, Semelka RC, Worawattanakul S, et al. Intraperitoneal abscesses: diagnostic accuracy of and appearances at MR imaging. Radiology 1998; 208:525-528.
- Jain KA. Imaging of peritoneal inclusion cysts. AJR Am J Roentgenol 2000; 174:1559 -1563.
- Kurachi H, Murakami T, Nakamura H, et al. Imaging of peritoneal pseudocysts: value of MR imaging compared with sonography and CT. AJR Am J Roentgenol 1993; 161:589 -591.
- Kim JS, Lee HJ, Woo SK, et al. Peritoneal inclusion cysts and their relationship to the ovaries: evaluation with sonography. Radiology 1997; 204:481-484.
- Sala EJ, Atri M. Magnetic resonance imaging of benign adnexal disease. Top Magn Reson Imaging 2003; 14:305-327.
- Togashi K, Ozasa H, Konishi I, et al. Enlarged uterus: Differentiation between adenomyosis and leiomyoma with MR imaging. Radiology 1989; 171:531-534.
- Kim JC, Kim SS, Park JY. "Bridging vascular sign" in the MR diagnosis of exophytic uterine leiomyoma. J Comput Assist Tomogr 2000; 24:57-60.
- Fleischer AC, Kalemeris GC, Entman SS. Sonographic depiction of the endometrium during normal cycles. Ultrasound Med Biol 1986; 12:271-277.
- Lisa Bame Schwartz, Ellen Panageas. Female pelvis: Impact of MR Imaging on treatment decision and net cost analysis. Radiology 1994; 192:55 -60.
Author Info
Department of Radio diagnosis, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Neeharika C, Ravindran C, Ultrasound and Magnetic Resonance Imaging Correlation of Adnexal Lesions, J Res Med Dent Sci, 2021, 9 (5):282-289.
Received: 03-Apr-2021 Accepted: 24-May-2021
