Research - (2021) Volume 9, Issue 4
Ultrasonogram Evaluation of Scrotal Pathologies with Elastography
Anish N and Prabakaran M*
*Correspondence: Prabakaran M, Department of Radio Diagnosis, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
The present study aims to evaluate the role of ultrasonography in diagnosis and Characterization of the scrotal pathologies and to compare with ultrasound elastography. Different ultrasound machines and transducers in a phantom and found the difference in mean shear wave velocities between three machines to be statistically significant (p ≤ 0.002). This necessitates a caution while using absolute cut-off values for comparison of measurements obtained from different ultrasound machines and transducers. Outcome of evaluation is better when elastography is done along with the routine B-mode ultrasound in terms of characterization of the lesion and early diagnosis in case of testicular tumors.
Keywords
Ultrasound, Elastography, Ultrasonography and Scrotal pathologies
Introduction
The scrotum which is a cutaneous bag contains the testes, the epididymis and the lower part of spermatic cord. Exteriorly, the median raphe/ ridge divides the scrotum into left and right hemiscrotum. This raphe persists backwards along the perineum in the midline towards the anus as well as forwards on to the undersurface of the root of penis. The testes are covered by some fibro muscular tissue as well as loose skin of little mm thickness and are not easily accessible for clinical examination. Depending solely on the physical examination does not permit diagnosis of some testicular pathology. Furthermore, it cannot be assumed that a palpable scrotal mass is a result of extra testicular elements or the testis itself. Significant pathology can be overlooked by the normal examination if interpreted improperly [1]. In scrotal swelling, the scrotal contents gross distortion, swelling or tenderness results in inadequate physical evaluation. Generally, the clinical symptoms and signs tend to be misleading, variable and nonspecific. The clinical evaluation for scrotal pathologies mainly included trans-illumination as well as palpation of the testis, until 1970. Such methods were not sufficient due to the gross scrotal contents as well as tenderness swelling resulting in low specificity and sensitivity despite the clinician’s best-efforts [2]. Solography’s widely portable, easily available, relatively inexpensive, with no radiation hazard, noninvasive, safe, repeatable and can be performed easily. Furthermore, no patients notice discomfort and it can also be performed on an outdoorbasis [3]. As scrotum is considered as one of the significant structure, it is essential to investigate the scrotal symptoms in patients using ultrasound on a routine basis. Furthermore, the scrotal ultrasound has become so advanced that this imaging method is the first-line investigation for evaluation of scrotal contents. The scrotal disease associated morphologic changes can be visualized excellently with the help of high frequency transducers that are used in the grey scale sonography. The parenchymal blood flow characteristics as well as visualization of morphology is allowed by the colour flow imaging. Moreover, the testicular scintigraphy is greatly replaced by the sonography, as these permit examination of patients having suspectedtorsion [1-3]. Ultrasound plays a significant part in the triage of patients having scrotal swelling as the evaluating clinician generally has a diagnostic dilemma. In acute scrotal pain, evaluation with ultrasound is considered as the preferred imaging modality due to its lack of ionizing radiation, repeatability, accessibility, speed as well as portability [1]. Moreover, same clinical manifestations are seen in various disease processes, such as mass, swelling or pain. For the proper management, these pathologies must be differentiated accordingly. The relative stiffness of the tissue can be determined by a new method that is known as Ultrasound elastography. Depending on the tissue’s physical properties the tissue compliance is determined. Ophir et al. [3] proposed this technique which primarily includes quasistatic elastography as well as dynamic elastography. These two techniques are mainly differentiated by tissues’s mechanical excitation. Quasistaticel elastography induces quasistatic compression in the tissue that causes the displacement or deformation of the tissues which can be tracked through various techniques through digital image processing . Digital signaling is used for the reflecting the tissues’ relative stiffness. Presently, the liver disease, thyroid disease and breast space- occupying lesions are studied with it, whereas there its application in scrotal lesions examination is very rare [4-11]. In dynamic ultrasound elastography the acoustic radiation forces originates the excitation in the tissues that emits the acoustic pulses which are longitudinally focused as short duration pulses in the direction of ROI (Region of Interest); then the local tissues displacement are reflecte dastheradiation forces, finally gray scale is used to express thes train amplitude differences, which then reflects the tissue stiffness directly [4]. In this study we evaluate the role of ultrasonogram in scrotal pathologies and compared with ultrasound elastography.
Materials and Methods
A descriptive study was performed with 50 patients between October 2017 and October 2019 (period of two years) who were referred to the department of Radiology at Sree Balaji Medical College and Hospital, Chennai for clinical USG scrotal examination due to symptoms suggestive of scrotal pathologies ( pain, swelling, infertility , trauma, lower abdominal discomfort).
Inclusion criterion
The study includes
✓ All the male patients suspected clinically to have scrotal pathologies between from 2 years and above.
✓ All the patients undergoing male infertility workup.
Exclusion criterion
The study excludes
✓ Children of age < 2 years due to practical difficulties in performing the procedure.
✓ Patients with linguistic difficulties in understanding the informed consent.
Method of collection of data
Patients referred to the department of radiology clinical symptoms suggestive of scrotal pathologies (pain, swelling, infertility, trauma, lower abdominal discomfort) were reviewed. A total number of 50 cases were taken for this study. After a brief history and physical examination of patient was done. The entire patient underwent conventional B- mode ultrasound examination and subsequently followed by ARFI / shear wave elastography. Both the testis was examined separately using 9 MHz linear 9L4 probe. Study was done using Siemens ACUSON S 2000 ultrasound sys- tem Siemens Medical Solutions, Mountain view, CA, USA with Virtual Touch tissue quantification software. Frame rate of 14 frames per second, soft tissue thermal index TIS of 0.8. bone thermal index of TIB of 1.2, and mechanical index of 1.6. On gray scale B-mode ultrasound the features of scrotal pathologies were first evaluated followed subsequently by elastography.
ARFI
In ARFI elastography, the displacement produces shear waves in orthogonal planes to the direction of displacement. The velocity of the shear wave so produced can be measured by ultrasonic beams calculating the phase difference between two points on the waveform. This is achieved by placing a region of interest (ROI) in close proximity to the tissue being displaced (Figure 1). Thus, the elastic modulus of a particular tissue can be calculated (high for hard tissues, low for soft tissues).
VTQ Elastography Imaging
VTQ is used to quantitatively assess the elasticity of the tissue by means of shear wave velocity (SWV). After identifying hard areas i.e the region of interest in strain elastography the ROI was placed over it to per- form shear wave elastography. The ROI was of fixed size 6mm x 5 mm and cannot be modified. The SWV was measured as velocity m/s value (range 0 – 9 m/s). Each time five measurements were taken at the region of interest and its median value is calculated and used for the study [8,2].
Statistical methods
Descriptive analysis was carried out by mean and standard deviation for quantitative variables, frequency and proportion for categorical variables. Data was also represented using appropriate diagrams like bar diagram, pie diagram and box plots.
Results
A total 50 (100) subjects involved in final analysis (Tables 1-3 and Figures 1-4).
Table1: Descriptive analysis of age in study population (N=50).
| Mean ± SD | 95% C.I | |||||
|---|---|---|---|---|---|---|
| Parameter | Median | Minimum | Maximum | Low | Up- | |
| er | per | |||||
| 33.72 | ||||||
| Age | ± | 33.5 | 5 | 67 | 29.54 | 37.9 |
| 14.71 | ||||||
Table 2: Descriptive analysis of testis volume (ml) in the study population.
| Testicular volume ml | frequency | Percentage |
|---|---|---|
| 12 – 18 | 97 | 97% |
| < 10 | 1 | 1% |
| >18 | 2 | 2% |
Table 3: Descriptive analysis of vascularity of bilateral testis / epididymis in the study population (N=100)
| Vascularity of Bilateral | ||
|---|---|---|
| Test /EPID | ||
| Frequency | Percentages | |
| Normal | 97 | 97.00% |
| absent | 2 | 2.00% |
| reduced | 1 | 1.00% |
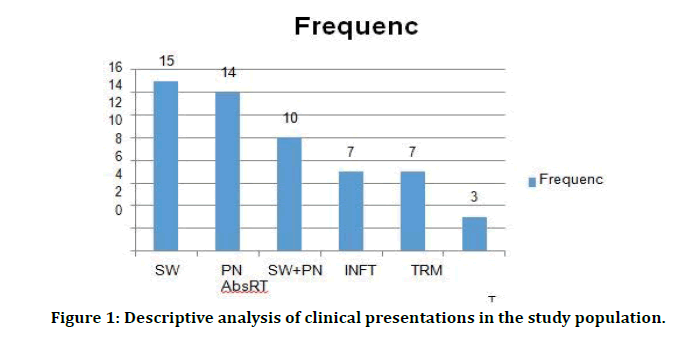
Figure 1: Descriptive analysis of clinical presentations in the study population.
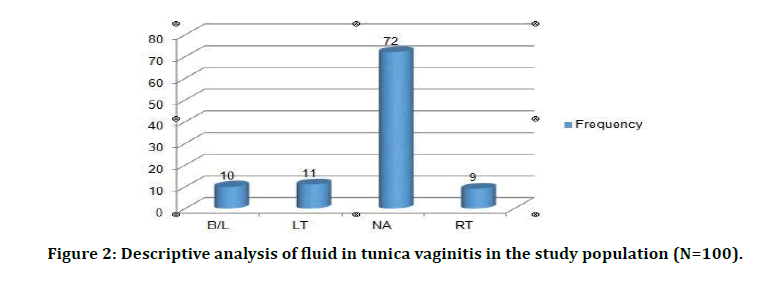
Figure 2: Descriptive analysis of fluid in tunica vaginitis in the study population (N=100).
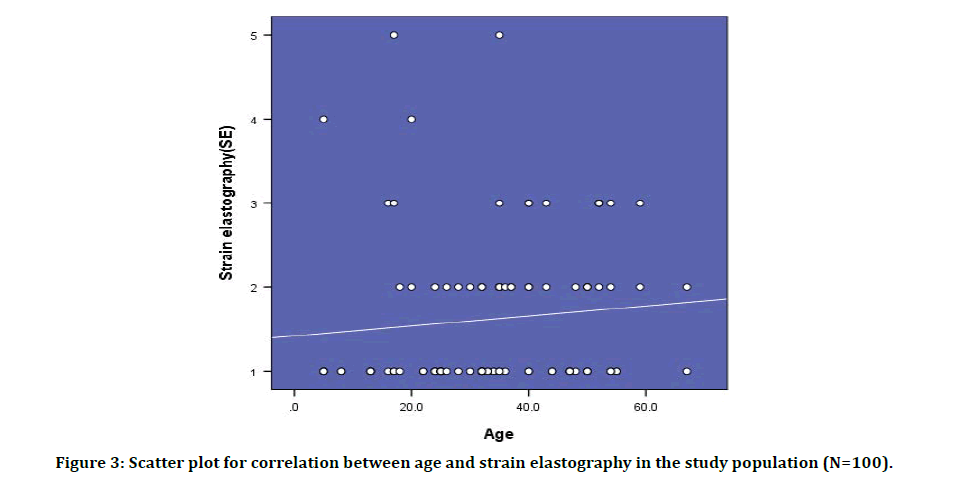
Figure 3: Scatter plot for correlation between age and strain elastography in the study population (N=100).
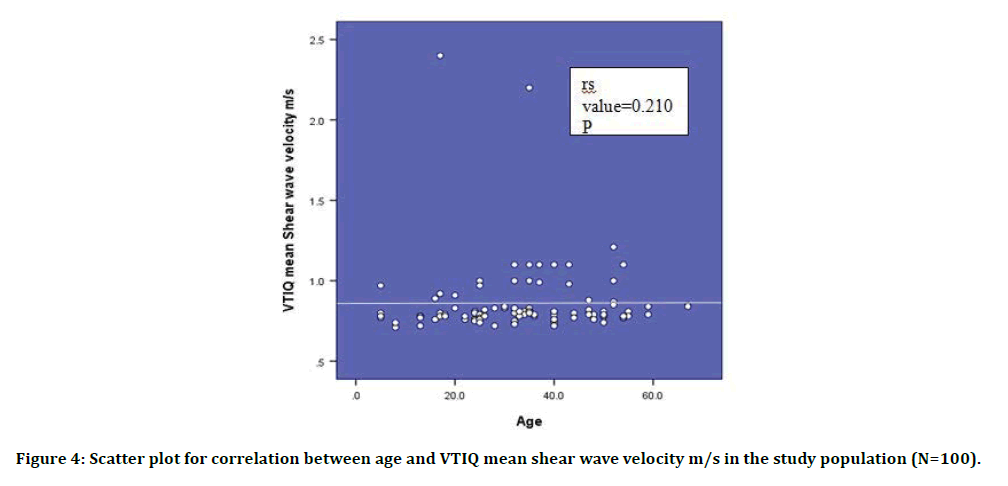
Figure 4: Scatter plot for correlation between age and VTIQ mean shear wave velocity m/s in the study population (N=100).
Discussion
The superficial location of the scrotal contents makes them ideally suited for sonographic examination. The development of high frequency, real time scanning techniques have increased the diagnostic accuracy in sonographic examinations of the scrotum. Scrotal ultrasound has reached a level of maturity that allows the technique to be considered as the first and only imaging examination necessary to evaluate the scrotal contents. In this study, we have examined 50 patients (100 testes) with high frequency ultrasound scan and ultrasound elastography, for detection of scrotal and testicular pathologies [12,13]. The age distributions of cases in this study are varied from 2 Years to 67 Years. Highest number of cases presented were seen in age group of 20 to 40 years (26cases–52%), followed by 41 to 60 years (14cases– 28%). Least number of cases was in age group above 60 years (1 case – 2%). The cases presented with various clinical presentations with frequency are, Commonest clinical presentation was combination of symptoms like, pain and scrotal swelling, as in 34 cases (34%), combination of pain, swelling and trauma in 17 cases (17 %) and infertility in 7 cases (12%)Swelling: 15 cases presented with swelling only (26.3%). Out of this, unilateral scrotal swelling noted in 9 cases (61%), bilateral in 6 cases (39%).Pain: 10 cases presented exclusively with only pain in scrotum (10%). Out of this, 6 cases presented with acute pain 60 %. Out of 10 cases of scrotal pain, 8 cases were on unilateral side (80%), 2 were on bilateral (20 %). Out of 8 cases of unilateral scrotal pain, 5 cases were on left side (63%), 3 cases were on right side (37%) [14-17]. The severity of scrotal pain was of varying degree, ranging from dull aching to very severe pain. Most of the acute onset scrotal pain, particularly those associated with fever had pain that was severe, where as those with insidious onset, without fever had a dull aching pain. Out of 23 cases of acute onset scrotal swellings, 7 cases (30%) had h/o trauma, 6 cases (26%) had h/o dysuria, 2 cases (8%) had h/o pain in lower abdomen [18,19]. Other associated symptoms include wound on scrotal skin 5 cases, redness of scrotal skin in 1case. Of three cases of acute epididymitis, we observed diffuse hypo- echogenicity with diffuse increase in vascularity, and increased size of epididymis. In the 9 cases with acute Epididymoorchitis, diffuse hypoechogenicity with diffuse increased vascularity was seen in 4 cases, 2 cases showed heterogenous echotexture, 3 cases had normal echotexture, 8 cases showed a diffuse increase in vascularity, one case showed focal increases in vascularity, and size of epididymiswas increased in 7 cases. Of the five cases of acute orchitis, we observed all five cases, on unilateral involvement, with two case on right side and three cases on left side.21 One case showed focal involvement, four cases showed diffuse involvement. On high frequency US sonography, focal involvement appeared as focal area of hypoechogenicity, four cases of diffuse involvement showed of 20 cases (40 testes) of inflammatory scrotal pathology, we noted acute epididymo-orchitis in 9 cases (45%). Of these, 11 % cases were bilateral involvement, 7 % cases were unilateral involvement. On Highfrequency US sonography, we observed diffuse increase in size of epididymis with testicular size in 6 cases, normal size of epididymis and testis in 3 cases. There was heterogenous echotexture in 4 cases, hypoechogenicity in 2 cases, normal echogenicity in 3 cases. There was evidence of epididymal calcification seen in 3 case, testicular micro calcificationin2 cases. One case of associated scrotal filariasis also noted, which showed classical “scrotal filarial dance” on high frequency USG [20-22]. In our study, 12 patients non-inflammatory scrotal swelling (34%) were examined, out of which 8 cases (85%) presented with swelling only, and 4 cases (15 %) presented with swelling along with pain. In the 4 cases with scrotal swellings with associated pain, the pain was mild dragging with low intensity, enabling differentiation of inflammatory swellings and non-inflammatory swellings. Of 12 cases of noninflammatory scrotal swellings, 2 case were neoplastic lesions, remaining 10 cases were non neoplastic swellings. The 2 case of neoplastic swellings were germ cell tumour [23].The studies had a small sample size and random effects were not taken in- to account. Variation also may be due to the ultrasound machine, soft-ware and transducer being used. The mean shear wave velocity in normal testicular tissue to be 1.17 m/s. An explanation for this observed velocity of 1.17 m/s in normal testis compared to our mean of 0.76 m/s could be due to different ultrasound machines. Another study which investigated 60 normal males, found velocities in the center of testicles (0.90 m/s) to be significantly lower than the mean velocities of 1.15 m/s at the superior and inferior parts of the testicles, whether this can be applied to testis with tumors remains unknown [24]. Shear wave velocities between different ultrasound machines and transducers in a phantom and found the difference in mean shear wave velocities between three machines to be statistically significant (p ≤ 0.002). This necessitates a caution while using absolute cutoff values for comparison of measurements obtained from different ultrasound machines and transducers.
Conclusion
In the present study we conclude that the high resolution B mode ultrasonogram plays a major role in the evaluation and characterization of scrotal pathologies and its complications. In present study we highlighted the various inflammatory pathologies like acute epididymo orchitis, acute orchitis, acute epididymitis, focal orchitis, acute funiculitis and chronic epididymitis. Non inflammatory pathologies like hydrocele, Encysted hydrocele of cord, varicocele, testicular torsion, testicular microlithiasis and tumors. We also concluded that the use of elastography (VTIQ) to be an asset, since it does not use manual transducer compression and therefore the testis are not displaced during measurement. VTIQ is operator-independent. The main limitation of this single center study is that it was only possible to obtain three to five velocity measurements in each testicle due to the daily workflow in our radiology department. More measurements would have yielded more precise estimates. The use of elastography seems a promising method for the evaluation of testicular lesions. Additionally in the present study we have highlighted the elasticity of the testicular tissue in various scenarios like in normal tissue, in testicular elastography and in tumors using strain elastography (VTI) and shear wave elastography (VTQ).We also managed to predict that the outcome of evaluation is better when elastography is done along with the routine B- mode ultrasound in terms of characterization of the lesion and early diagnosis in case of testicular tumors.
Acknowledgement
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Dogra VS, Gottlieb RH, Oka M, et al. Sonography of the scrotum. Radiology 2003; 227:18-36.
- Meacham RB, Townsend RR, Rademacher D, et al. The incidence of varicoceles in the general population when evaluated by physical examination, gray scale sonography and color doppler sonography. J Urology 1994; 151:1535-8.
- Ophir J, Alam SK, Garra B, et al. Elastography: Ultrasonic estimation and imaging of the elastic properties of tissues. Proceedings of the institution of mechanical engineers, Part H. J Eng Med 1999; 213:203-33.
- Shiina T, Nightingale KR, Palmeri ML, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography, Part 1: Basic principles and terminology. Ultrasound Med Biol 2015; 41:1126–1147.
- Matsubayashi RN, Imanishi M, Nakagawa S, et al. Breast ultrasound elastography and magnetic resonance imaging of fibrotic changes of breast disease: correlations between elastography findings and pathologic and short tau inversion recovery imaging results, including the enhancement ratio and apparent diffusion coefficient. J Computer Assisted Tomography 2015; 39:94-101.
- Zhang Q, Xiao Y, Chen S, et al. Quantification of elastic heterogeneity using contourlet-based texture analysis in shear wave elastography for breast tumor classification. Ultrasound Med Biol 2015; 41:588-600.
- Ianculescu V, Ciolovan LM, Dunant A, et al. Added value of virtual touch IQ shear wave elastography in the ultrasound assessment of breast lesions. Eur J Radiol 2014; 83:773-777.
- Kantarci F, Olgun DC, Mihmanli I. Shear-wave elastography of segmental infarction of the testis. Korean J Radiol 2012; 13:820.
- Chen L, Freeman SJ, Gee AH, et al. Initial clinical experience of an ultrasonic strain imaging system with novel noise-masking capability. Br J Radiol 2010; 83:702-6.
- D’Anastasi M, Schneevoigt BS, Trottmann M, et al. Acoustic radiation force impulse imaging of the testes: A preliminary experience. Clin Hemorheol Micro 2011; 49:105–114.
- Patel K, Sellars ME, Clarke JL, et al. Features of testicular epidermoid cysts on contrast-enhanced sonography and real time tissue elastography. J Ultrasound Med 2012; 31:115-22.
- Thomas RD, Dewbury KC. Ultrasound appearances of the rete testis. Clin Radiol 1993; 47:121-124.
- Dogra VS, Gottlieb RH, Oka M, et al. Sonography of the scrotum. Radiol 2003; 22:18-36.
- Horstman WG, Middleton WD, Melson GL, et al. Color Doppler US of the scrotum. Radiographics 1991; 11:941-57.
- Burks DD, Markey BJ, Burkhard TK, et al. Suspected testicular torsion and ischemia: Evaluation with color doppler sonography. Radiology 1990; 175:815-21.
- Middleton WD, Siegel BA, Melson GL, et al. Acute scrotal disorders: prospective comparison of color Doppler US and testicular scintigraphy. Radiology 1990; 177:177-81.
- Luker GD, Siegel MJ. Color Doppler sonography of the scrotum in children. AJR. Am J Roentgenol 1994; 163:649-55.
- Caesar RE, Kaplan GW. Incidence of the bell-clapper deformity in an autopsy series. Urology 1994; 44:114-116.
- Middleton WD, Middleton MA, Dierks M, et al. Sonographic prediction of viability in testicular torsion: preliminary observations. J Ultrasound Med 1997; 16:23-7.
- Chan PT, Schlegel PN. Inflammatory conditions of the maleex- current ductal system. Part II. J Androl 2002; 23:461-469.
- Rajfer J, Walsh PC. Testicular descent: normal and abnormal. Urologic Clin North Am 1978; 5:223-35.
- Hardine R, David H. Bailey and loves short practice of surgery. CRC Press 2008.
- Luker GD, Siegel MJ. Color Doppler sonography of the scrotum in children. Am J Roentgenol 1994; 163:649-55.
- Lentini JF, Benson CB, Richie JP. Sonographic features of focal orchitis. J Ultrasound Med 1989; 8:361-365.
Author Info
Anish N and Prabakaran M*
Department of Radio Diagnosis, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Anish N, Prabakaran M, Ultrasonogram Evaluation of Scrotal Pathologies With Elastography, J Res Med Dent Sci, 2021, 9 (4):243-248.
Received: 20-Mar-2021 Accepted: 06-Apr-2021
