Research - (2021) Volume 9, Issue 4
To Study and Analyze Transversalis Fascia Repair with Tension Free Onlay Mesh Repair in all Direct Hernias
Pon Jeeva Mathan D and Bhaskaran PK*
*Correspondence: Bhaskaran PK, Department of General Surgery, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, India, Email:
Abstract
Hernias have been a subject of interest since the dawn of surgical history. The history of hernia repair is the history of surgery. To study and analyze transversalis fascia repair with tension free onlay mesh repair in all direct hernia.
Keywords
Inguinal hernia, Femoral hernia, General surgery
Introduction
An inguinal hernia is defined as a protrusion of abdominal contents through a defect in the abdominal wall of the groin. Although no exact figures are available, a prevalence varying from 10% to 15% in adults in the Western hemisphere has been estimated, with a male to female ratio of 12:1. Although the incidence of inguinal hernia rises with age, relatively young people are affected: an incidence between 5 and 8 % in patient 25 to 40 years of age has been reported. Inguinal hernia repair is the most frequently performed surgical procedure. In the United States approximately 700.000 procedures are performed annually, and in the Netherlands 25.000. Consequently, inguinal hernias not only affect individual patients but also have a great impact on society. Failure of inguinal hernia repair leads to increased patient discomfort, reoperations, and sick-leave, and therefore may result in a considerable economic burden [1-10].
Materials and Methods
All patients undergoing direct hernia repair in SBMCH Chennai from February 2015-October 2016.
Inclusion criteria
All direct Hernia patients getting to admit in Sree Balaji Medical College for a period of February 2015 to October 2016.
Exclusion criteria
Femoral Hernia, Emergency Hernia Indirect Hernia, Recurrent Hernia, All Other Types of Hernias Allergy to Prolene.
Methods and Collection of Data
Patient data collection and evaluation
Data will be collected from all patients attending SBMCH general surgery OPD and admitted in department of general surgery and undergoing hernia repair The patient will be evaluated and followed up according to protocol Detailed history of patient will be entered in proforma Patient is investigated and evaluated for any other co morbidities Patient will be informed about surgical procedure and informed written consent will be taken .Once patient is operated, the patient is observed for complications Patient is then followed up according to protocol.
Patient data collecting regarding
Demographic data such as age, race, gender as well as co- morbid conditions such as chronic obstructive pulmonary disease, congestive heart failure, previous myocardial infarction, diabetes, hypertension, prostatism and chronic cough were collected. The type of anaesthesia for each patient were recorded. Information about the size and type of each hernia was collected. Operative times (skin incision to skin closure) were recorded for each repair. Intra operative complications including iatrogenic vessel and nerve injury and as well as anaesthesia related complications were recorded. Any postoperative complications such as cord and vessel injury, seroma, haematoma, urinary retention, wound infection, and stiffness of abdominal wall were documented. Patients were followed up till date.
Follow up
Patients will be followed up at 1, 3 and 6 months of surgery after discharge for any recurrence or development of complications.
Results
The study period was from Sree Balaji Medical College & Hospital, Chennai-44. between the period of 2015 February and 2016 October. The age ranged from 20 -80 years, the mean age being 45.8 years. Maximum cases were above the age of 40 years. There were 50 males and 10 females, the male: female ratio being 5:1 (Table 1 and Figure 1).
| S. No | N=60 | |
|---|---|---|
| Mean age | 45.8 in Years | |
| 1 | Sex | |
| Male | 50 | |
| Female | 10 | |
| 2 | Types | |
| Inguinal | 59 | |
| Femoral | 1 | |
| 3 | Sites | |
| Right | 48 | |
| Left | 10 | |
| Bilateral | 2 | |
| Recurrent Hernia | 0 |
Table 1: Patient characteristics.
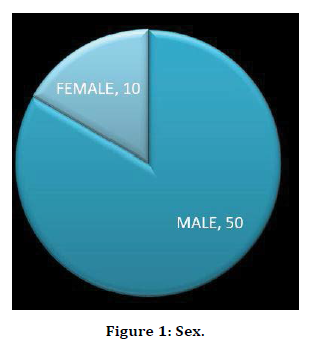
Figure 1. Sex.
Out if the 60 patients studied, 17(28.3%) were coolie by occupation. Right sided inguinal hernia was the most common site involved in 48 (80%) patients followed by the left in 10 (16.6%) patients and trunk in 2 (3. 33%) patients (Figure 2).
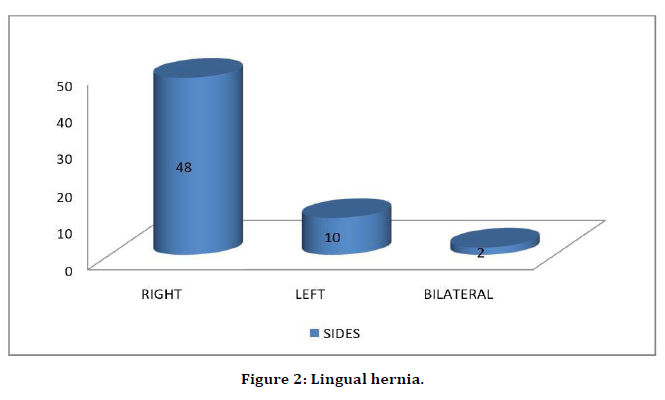
Figure 2. Lingual hernia.
Intraoperative complication such as injury to ilioinguinal nerve in 10 cases (16.6%). inferior epigastric injury is seen in 2 cases (3.3%). Diathermy burns is seen in 3 cases (5%) (Table 2 and Figure 3).
| S.no | Complications | No. of cases (n=60) |
|---|---|---|
| 1 | Injury To VAS | 0 |
| 2 | Nerve injuries | 10(16.6%) |
| 3 | Visceral injury | 0 |
| 4 | Epigstric vessel injury | 2(3.33%) |
| 5 | Diathermy burns | 3(5%) |
Table 2: Intraoperative complications.
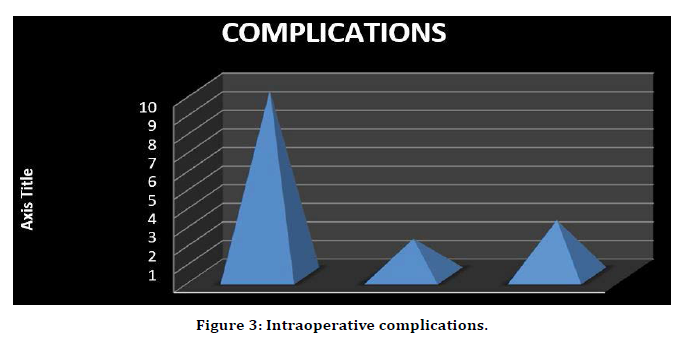
Figure 3. Intraoperative complications.
Clinical outcome after a week wound complication such as seroma is seen in 15 cases (25%) hematoma is seen is 2 cases (3.33%), mesh infection is seen in 1 case (1.66%). Scrotal complications such as hematoma is 2 cases (3.33%), cord edema is seen in 5 cases (8.33%). Urinary retention is seen in 20 cases (33.3%) (Table 3, Figures 4 and 5).
| S.No | Complication types | Types | No of cases |
|---|---|---|---|
| 1 | Wound complications | Seroma | 15(25%) |
| Hematoma | 2(3.33%) | ||
| Infection | 1(1.66%) | ||
| 2 | Scrotal complications | Hematoma | 2(3.33%) |
| Edema | 5(8.33%) | ||
| 3 | Urinary retention | 20(33.33%) |
Table 3: Types of complications.
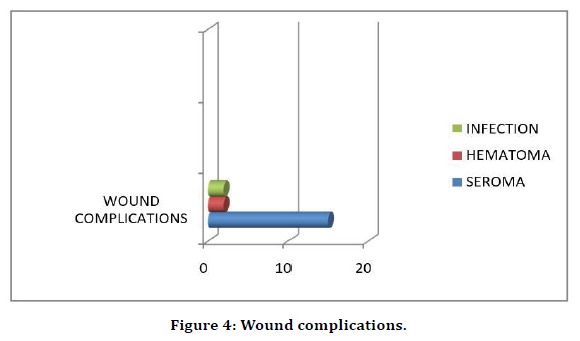
Figure 4. Wound complications.
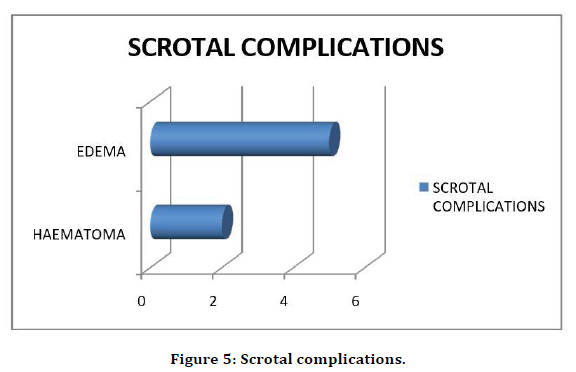
Figure 5. Scrotal complications.
Patient was able to resume to work to look after the household works in 50 cases within 3 days. They can resume to enjoy the usual life within 6 days in 48 cases. Able to do works with interests in 8 days within 44 days (Table 4 and Figure 6).
| S. No | No of cases | No of days | |
|---|---|---|---|
| 1 | Able to look after house | 50 | 3 |
| 2 | Able to enjoy usual life | 48 | 6 |
| 3 | Able to enjoy usual interests | 44 | 8 |
| 4 | Able to return to paid employment | 40 | 12 |
Table 4: Clinical outcome.
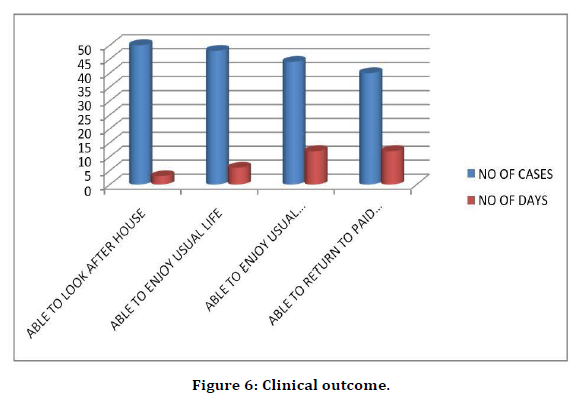
Figure 6. Clinical outcome.
Patient was able to return to normal paid employment within 12 days in 40 cases. After regular follow up for one year the following things are being observed. Recurrence of hernia is seen in 1 case which is 1.66%. New contralateral hernia is seen in 4 cases which is 6.66% Chronic pain is seen in 10 cases which is 16.66%. The mortality rate was nil (0%) (Table 5 and Figure 7).
| S.NO | Outcome | |
|---|---|---|
| 1 | Recurrence of hernia | 1(1.66) |
| 2 | New contraleral hernia | 4(6.66) |
| 3 | Testicular atrophy | 0 |
| 4 | Wound sinus | 0 |
| 5 | Chronic pain | 10(16.66) |
Table 5: Clinical outcome at one year.
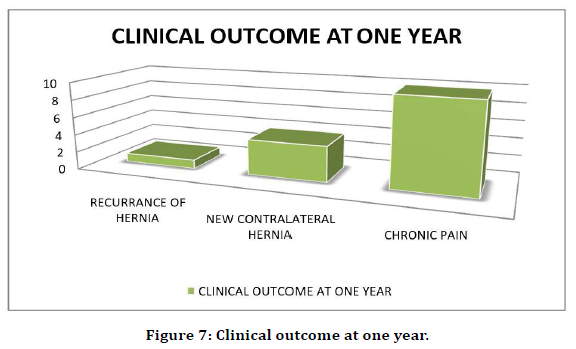
Figure 7. Clinical outcome at one year.
Inguinal hernia was seen in 59 cases and 1 case of femoral hernia Patients are usually associated symptoms as follows Constipation in 6 cases (10%), chronic cough is seen in 4 cases (6.66%), difficulty in passing urine is seen in 3 cases (5%). 10 cases are associated with smoking history Which is 16. 66%, and 20 cases doesn’t have any comorbidities (Table 6 and Figure 8).
| S. No | Associated symptoms | No of cases |
|---|---|---|
| 1 | No comorbidities | 20(33.33%) |
| 2 | Smoking | 10(16.66) |
| 3 | Constipation | 6(10%) |
| 4 | Chronic cough | 4(6.66) |
| 5 | Difficulty in micturition | 3(5%) |
Table 6: Associated symptoms.
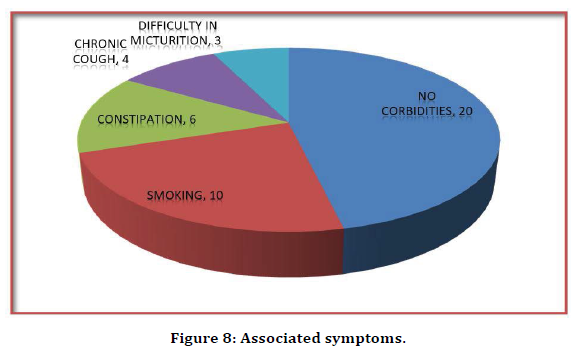
Figure 8. Associated symptoms.
Discussion
In this study–to study and analyze the transversalis fascia repair with tension free on-lay mesh repair in all direct hernia cases admitted in Sree Balaji medical college for a period of February 2015 to October 2016.
Advantages
Minimalise the recurrence rate- all hernia defect of the transversalis fascia Strengthening of the posterior wall Proper wound bed for mesh repair Push the peritoneum – look for femoral hernia underlying as association of underlying femoral hernia is 5%.
An indirect inguinal hernia begins with a small peritoneal sac at the deep inguinal ring, but for it to grow there must be a yielding or relaxation of the transversalis fascia and transverses abdominus aponeurosis above the deep inguinal ring. The fundamental rupture, relaxation or discontinuity in musculoaponeurotic structure in inguinal hernia occurs in the deeply placed transversus abdominus – transversalis fascial layer of the groin. Tissue based suture repair by different techniques (Bassini’s, Shouldice etc.) has remained the most conventional surgical treatment of inguinal hernia. These techniques shared many things in common such as excessive tension on the suture line as well as the neighboring tissues, a lot of dissection, trauma and undue operative time. These factors were found to be responsible for a number of recurrences, persistent pain after surgery and morbidity leading to an undue economic burden on the patient. 9 This led to the introduction of mesh repair in the late 1980’s with the concept of tension free repair of hernias. 10 Since then several studies have claimed improved results with mesh repair in terms of recurrence of hernia [11-15].
Conclusion
An inguinal hernia is defined as a protrusion of abdominal contents through a defect in the abdominal wall of the groin. Although no exact figures are available, a prevalence varying from 10% to 15% in adults in the Western hemisphere has been estimated, with a male to female ratio of 12:1. Although the incidence of inguinal hernia rises with age, relatively young people are affected: an incidence between 5 and 8 % in patient 25 to 40 years of age has been reported. Inguinal hernia repair is the most frequently performed surgical procedure. This study was a prospective study of transversalis fascia repair in all direct hernia. this study involved a single group of 60 patients with direct hernia admitted in sree balaji medical college and hospital, Chennai -44 between the period of February 2015 To October 2016.
This study ranges from The age ranged from 20 -80 years, the mean age being 45.8 years. Maximum cases were above the age of 40 years. There were 50 males and 10 females, the male: female ratio being 5:1 Out if the 60 patients studied, 17(28.3%) were coolie by occupation.
Right sided inguinal hernia was the most common site involved in 48 (80%) patients followed by the left in 10 (16.6%) patients and trunk in 2 (3. 33%) patients. Inguinal hernia was seen in 59 cases and 1 case of femoral hernia Patients are usually associated symptoms as follows Constipation in 6 cases (10%), chronic cough is seen in 4 cases (6.66%), difficulty in passing urine is seen in 3 cases (5%). 10 cases are associated with smoking history which is 16.66%, and 20 cases does not have any comorbidities.
Intraoperative complication such as injury to ilioinguinal nerve in 10 cases (16.6%). inferior epigastric injury is seen in 2 cases (3.3%). Dither my burns are seen in 3 cases (5%) Clinical outcome after a week wound complication such as seroma is seen in 15 cases (25%) hematoma is seen is 2 cases (3. 33%), mesh infection is seen in 1 case (1.66%). Scrotal complications such as hematoma is 2 cases (3.33%), cord edema is seen in 5 cases (8.33%). Urinary retention is seen in 20 cases (33.3%).
Patient was able to resume to work to look after the household works in 50 cases within 3 days. They are able to resume to enjoy the usual life within 6 days in 48 cases. Able to do works with interests in 8 days within 44 days. Patient was able to return to normal paid employment within 12 days in 40 cases.
After regular followup for one year the following things are being observed. Recurrence of hernia is seen in 1 case which is 1.66% Chronic pain is seen in 10 cases which is 16.66% The mortality rate was nil (0%).
Incidence of femoral hernia was studied, and we found a patient and repaired intraoperatively Time to return to normal activity was earlier and patient satisfaction level was good.
Funding
No funding sources.
Ethical Approval
The study was approved by the institutional ethics committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Kingsnorth AN, Gray MR, Nott DM. Prospective randomized trial comparing the shouldice technique and plication darn for inguinal hernia. Br J Surg 1992; 79:1068 –1070.
- Deysine M, Soroff HS. Must we specialize herniorrhaphy for better results? Am J Surg 1990; 160:239–241.
- Welsh DR, Alexander MA. The shouldice repair. Surg Clin North Am 1993; 73:451–469.
- Berliner SD, Wise L. Transversalis fascia hernioplasty. N Y State J Med 1980; 80:25–27.
- Berliner SD. An approach to groin hernia. Surg Clin North Am 1984; 64:197–213.
- Glassow F. The surgical repair of inguinal and femoral hernias. Can Med Assoc J 1973; 108:308–313.
- Obney N. Shouldice technique for repair of inguinal hernia. Bull N Y Acad Med 1979; 55:863– 866.
- Mansberger JA, Rogers DA, Jennings WD, et al. A comparison of a new two-layer anatomic repair to the traditional shouldice herniorrhaphy. Am Surg 1992; 58:211–212.
- Carbon RT. Evaluation of biodegradable fleece–bound sealing: History, material science, and clinical application. In: Lewandrowski KU, Wise DL, Trantolo DJ, et al. Tissue engineering and biodegradable quivalents: Scientific and clinical applications. New York: Marcel Dekker Inc 2002; 587 –650.
- Arslani N, Patrlj L, Kopljar M, et al. Advantages of new materials in fascia transversalis reinforcement for inguinal hernia repair. Hernia 2010; 14:617–21.
- Klosterhalfen B, Junge K, Klinge U. The lightweight and large porous mesh concept for hernia repair. Expert Rev Med Devices 2005; 2:103.
- Klosterhalfen B, Hermanns B, Rosch R. Biological response to mesh. Eur Surg 2003; 35:16–20.
- Junge K, Klinge U, Rosch R, et al. Decreased collagen type I/III ration in patients with recurring hernia after implantation of alloplastic prosthesis. Langenbecks Arch Surg 2004; 389:17–22.
- Sauerland S, Schmedt CG, Lein S, et al. Primary incisional hernia repair with or without polypropylene mesh: A report on 384 patients with 5 – year follow-up. Langenbecks Arch Surg 2005; 390:408–412.
- Cobb WS, Burns JM, Kercher KW, et al. Normal intraabdominal pressure in healthy adults. J Surg Res 2005; 129:231–235.
- Badylak S, Kokini K, Tullius B, et al. Morphologic study of small intestinal submucosa as a body wall repair device. J Surg Res 2002; 103:190–202.
Author Info
Pon Jeeva Mathan D and Bhaskaran PK*
Department of General Surgery, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Pon Jeeva Mathan D, Bhaskaran PK, To Study and Analyze Transversalis Fascia Repair with Tension Free Onlay Mesh Repair in all Direct Hernias, J Res Med Dent Sci, 2021, 9 (4):452-458.
Received: 20-Mar-2021 Accepted: 23-Apr-2021
