Research - (2021) Volume 9, Issue 7
To Compare and Assess Dynamic Hip Screw and Proximal Femur Nail in Intertrochenteric Femur Fracture
Vivek Amritbhai Patel, Chintan Bharatbhai Sheth*, Sangeen Bhundiya, Sangeen Bhundiya, Saurabh Rajeshbhai Patel, Adarsh Vishnubhai Patel and Deep Manojbhai Pavani
*Correspondence: Chintan Bharatbhai Sheth, Department of Orthopaedics, Gujarat Adani Institute of Medical Sciences, India, Email:
Abstract
Introduction: Intertrochanteric fractures of femur are one of the commonest musculoskeletal injuries in patients of above sixty years age group because of trivial fall and osteoporotic nature of bones. Different studies have been showing controversial results between Dynamic Hip Screw & intramedullary fixation devices historically. Aim: Aim of our study is to compare functional and clinical outcome of dynamic hip screw (DHS) and intramedullary proximal femoral nail (PFN) in intertrochanteric femur fractures. Material & Methods: Our study included (n=50) patients with intertrochanteric fracture of femur from which (n=25)50% patients operated with DHS and other (n= 25)50% patients operated with PFN. In our study average age of patient was 63years. Most common mode of injury was trivial fall and 54% patients were female. There were (n= 28)56% stable & (n= 22) 44% unstable fractures out of 50 intertrochanteric fractures. Results: Mean duration of surgery, blood loss during surgery and length of incision were less in PFN group than DHS group. Fluoroscopy time is higher in PFN group than DHS group. Postoperative shortening was more in DHS group and postoperative range of motion was better in PFN group. Union time is faster in PFN group. Malunion was seen in (n=5) 20% patients of DHS group while there were (n=2)8% cases of malunion in the PFN group. Wound infection was seen in (n=3) 12% patients in the DHS group and in (n=1)4% patient in the PFN group. Conclusion: At the end of the study we came with the conclusion that in stable intertrochanteric fracture DHS & PFN had similar results but in case of unstable fracture PFN was significantly better in terms of functional and clinical outcomes.
Keywords
Intertrochanteric, Fracture, Proximal femoral nail, Dynamic hip screw
Introduction
Intertrochantric femur fractures are commonest hip fracture in elderly population. It accounts for approximately half of hip fracture. Incidence of intertrochanteric fracture has been increasing with rising age of modern population due to advancement of technology in medical field [1,2]. In elderly population commonly intertrochantric fracture results from simple fall however in younger individual high energy trauma is commonest mode of injury for intertrochantric fracture. Incidence of intertrochantric fracture is around two times more in female as compared to male due to more predisposition of female gender to osteoporosis. It is one of the commonest causes of significant morbidity & mortality in the geriatric society which increases the overall financial burden on the family & non productiveness at the country. Management aim of these fractures should be the faster rehabilitation with early union time.
There are two primary options for fixation of these type of fracture (a) Extra medullary fixation (ex. DHS) and (b) Intramedullary fixation (ex. GAMMA nail, PFN) [3,4].
DHS (Dynamic hip screw) is extramedullary load sharing device and long procedure and it has gained widespread acceptance in these types of fractures [5-9]. However intramedullary implants have a biomechanical advantage10 of smaller distance between weight bearing axis and the implants.
AO/ASIF introduce PFN (Proximal femoral nail) in 1996 and it became more popular implant for intertrochantric fracture because it has biomechanical advantages like being load bearing device, shorter lever arm, being axial, greater implant length. Addition of anti-rotation hip screw proximal to main lag screw given which is significant advantage over DHS. Although mechanical failures are also seen with PFN [10-12] and PFN is also little bit costlier than DHS, still there are many benefits with PFN over DHS.
Dynamic Compression devices works on the principle of controlled collapse the fracture site & are commonly used for Intertrochanteric fractures as name Dynamic Hip Screw (DHS) & Proximal femoral nail (PFN) is an intramedullary nail device which works on the principle of fracture relatively static & anti-rotation support [13,14].
Materials and Methods
Our study was done in (N=50) patients of intertrochantric fracture at Gujarat Adani institute of Medical Sciences, Bhuj, Gujarat from October 2018 to October 2020.All the patients operated by senior orthopaedic surgeon. Informed and written consent have been taken of all patients to be included in the study. This study was approved by Institutional Ethics Committee. Ethical committee Approval letter No: GAIMS/IEC/ APPROVAL/40/2018. Inclusion criteria: Skeletally mature patients (age >18), only closed fracture, time <2 weeks. Exclusion criteria: Skeletally immature patients, compound fracture, pathological fracture, any other associated injury or fracture.
All patients with intertrochantric fracture were hemodynamically stabilized. X ray pelvis with both hip anteroposterior view and full femur anteroposterior view and lateral view were taken. All routine workup for surgery was done. Traction was applied to patients till surgery. All surgery was done over traction table under image intensifier guidance.
Decision for type of operation was based on surgeon’s choice. All patients had similar antibiotic coverage post operatively. Suture removal was done between 12 to 17 days. All patients were followed up weekly till 1 month and then every monthly till 6 months and every 3 months till 12 months.
Assessment of patients and comparison were done in terms of duration of surgery, total amount of blood loss, time of union, early and late complications, timing of early mobilization and full weight bearing. Clinical and radiological assessment was done at end of 12 months using Harris hip score.
Observation And Results
Our study consists of 50 patients from which 62% patients were aged more than 60 and 38% aged below 60 years. In our study 54% were female and 46% were male. Most common mode of injury was trivial fall in 76 % cases; other 24% cases result from high velocity trauma.
Malunion was seen in 20% of the patient in DHS group while there was 8% malunion in the PFN group. Wound infection was seen in (n=3) patients in DHS group and in (n=1) patient in PFN group. In two patients screw back out was seen in DHS while only in one patient screw back out was seen in PFN group.
All patients in our study had radiological union at end of 6 months. Mean time of fracture union was less in PFN group than DHS group with 11.84 weeks in PFN group while 12.4 weeks in DHS group. There was significantly better mean postoperative range of motion (flexionextension) in PFN thanDHSwith89.4 degree mean in DHS group and 101.4 degree mean in PFN group. Significantly less limb length shortening was seen in the PFN group as compared to the DHS group with a mean of 1.18cms in the DHS group and 0.62cms in the PFN group.
At the end of 6 months based on Harris hip score excellent to good results were seen in 88% of patient in PFN group and 60% of patients in DHS group (p= 0.012).
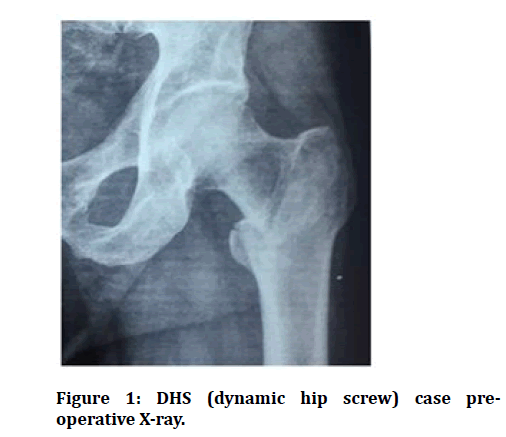
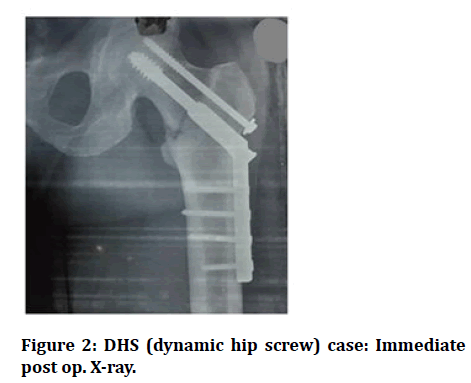
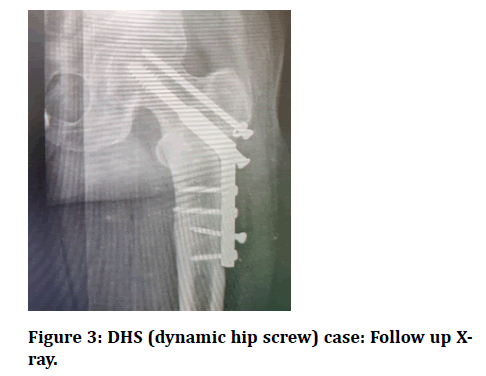
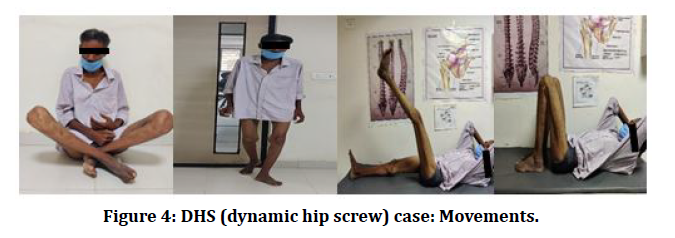
Out of 16 stable fractures 13 had excellent to good outcome, while out of the 9 unstable fracture7 had fair to poor outcome in the DHS group. Out of 12 patients with stable fracture 11 patients had excellent to good functional outcome in PFN group while out of 13 patients with unstable fracture11 patients had excellent to good functional outcome (Tables 1 to Table 4) and (Figures 1 to Figure 8).
Table 1: Types of fractures.
| Type of fracture | Method of Fixation | Total | |
|---|---|---|---|
| DHS | PFN | ||
| T1 | 2 (8.0%) | 1 (4.0%) | 3 (6.0%) |
| T2 | 14 (56.0%) | 11 (44.0%) | 25 (50.0 %) |
| T3 | 7 (28.0%) | 9 (36.0%) | 16(32%) |
| T4 | 2 (8.0%) | 4 (16.0%) | 6 (12.0%) |
| T5 | 0(0.0%) | 0(0.0%) | 0(0.0%) |
| Total | 25(100.0%) | 25(100.0%) | 50 (100.0%) |
Table 2: Various parameters.
| Parameter | DHS | PFN | |||||
|---|---|---|---|---|---|---|---|
| N | Mean | SD (STD. Deviation) | N | MEAN | SD (STD. Deviation) | P value | |
| Length of incision (cm) | 25 | 15.76 | 1.45 | 25 | 7.96 | 0.93 | 0.0001 |
| Duration of surgery(min) | 25 | 85.2 | 10.55 | 25 | 67.2 | 9.79 | 0.0001 |
| Fluoroscopy time (minutes) | 25 | 56.4 | 3.68 | 25 | 67.2 | 9.79 | 0.0001 |
| Blood loss (ml) | 25 | 406 | 56.49 | 25 | 126 | 32.65 | 0.0001 |
| Postoperative shortning (cm ) | 25 | 1.18 | 0.62 | 25 | 0.62 | 0.52 | 0.0011 |
| Postop range of movement(degree) | 25 | 89.4 | 9.82 | 25 | 101.4 | 12.29 | 0.0004 |
| Time of fracture union (weeks) | 25 | 12.4 | 1.71 | 25 | 11.84 | 1.42 | 0.2 |
Table 3: Functional outcome v/s method of fixation (stable fracture).
| Results | Method of Fixation | Total | |
|---|---|---|---|
| DHS | PFN | ||
| Excellent | 4(25.0%) | 3 (25.0%) | 7 (25%) |
| Good | 9 (56.2%) | 8 (66.66%) | 17 (60.71%) |
| Fair | 2 (12.5%) | 1 (8.33%) | 3 (10.7%) |
| Poor | 1 (6.25%) | 0 (0.0%) | 1 (3.5%) |
| Total | 16 (100.0%) | 12 (100.0%) | 28 (100.0%) |
c2=0.227, p=0. 97(nonsignificant)
Table 4: Functional outcome v/s method of fixation (unstable fracture).
| Results | Method of Fixation | Total | |
|---|---|---|---|
| DHS | PFN | ||
| Excellent | 1 (11.1%) | 4 (30.7%) | 4 (18.18%) |
| Good | 1(11.1%) | 7 (53.8%) | 11 (50%) |
| Fair | 5(55.5%) | 1 (7.6%) | 4 (18.18%) |
| Poor | 2(22.2%) | 1 (7.6%) | 3 (13.6%) |
| Total | 9 (100.0%) | 13 (100.0) | 22 (100.0%) |
p=0.04 (Significant)
Figure 1: DHS (dynamic hip screw) case preoperative X-ray.
Figure 2: DHS (dynamic hip screw) case: Immediate post op. X-ray.
Figure 3: DHS (dynamic hip screw) case: Follow up Xray.
Figure 4: DHS (dynamic hip screw) case: Movements.
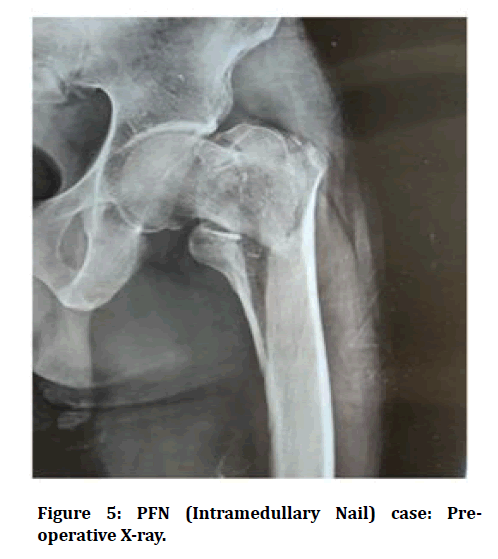
Figure 5: PFN (Intramedullary Nail) case: Preoperative X-ray.
Figure 6: PFN (Intramedullary Nail) case: Immediate postop. X-ray.
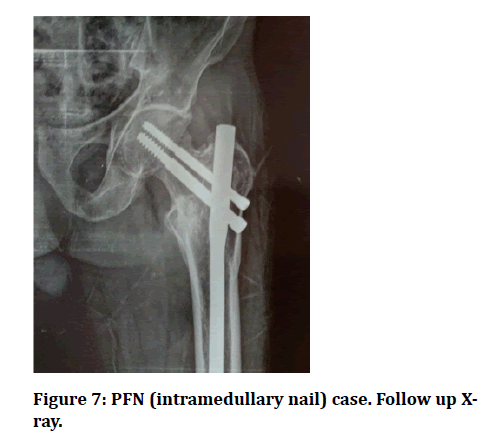
Figure 7: PFN (intramedullary nail) case. Follow up Xray.
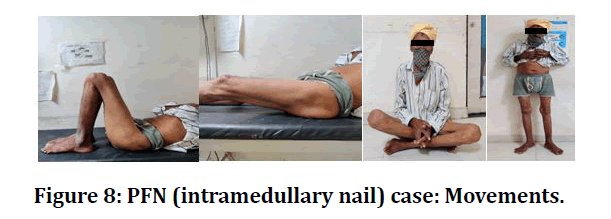
Figure 8: PFN (intramedullary nail) case: Movements.
Discussion
Our study consists of 50 patients with intertrochanteric fracture out of which 62% patients were aged more than 60 years. In our study 54% patients were female while in Dahl et al. [15] study 65% of patients were females, explained by the fact that female is more prone for the osteoporosis after menopause.
Mean duration of surgery for DHS group was 85.2 min which was significantly higher than mean duration of surgery for PFN group (67.2 min) Baumgaertner et al. [16] also found that the surgical times were 10 per cent higher in the DHS group in their series. but the fluoroscopy timing was opposite in both groups, in case of DHS it was 56.4 minutes and in case of PFN it was 67.2 minutes which was longer than DHS.
Mean length of incision in patients of DHS group and PFN groups were found to be 15.67 cm and 7.96 cm respectively with p =0.0001. Due to longer incision and duration of surgery blood loss was higher in DHS group with average of 406 ml and lower in PFN group with an average of 126 ml which shows significant less blood loss in PFN group. This was comparable to the study conducted by Baumgaertner et al [16].
In our study, complications like Wound infection in 3 patients of DHS group was higher than PFN group due to longer operation time and longer incision. In PFN only 1 patient got wound infection and which was superficial infection only. Saudan et al. [17] also did not find any significant difference between the infection rates in the two groups in their series. screw cut-out occurs in 2 patients of DHS group while only in 1 patient of PFN group screw backout occurs. There was no implant cut out in the PFN group which was similar to the series by Menezes et al. [18].
Postoperative Range of Motion (flexion-extension) in DHS group was average 89.4 degrees while in PFN it was average 101.4 degrees which was higher than the PFN group. Postoperative shortening was also significantly higher in DHS group compare to PFN group.
Time of union was higher in the DHS group with average 12.4 weeks for union and 5 out of 25 patients fractures got malunion while in PFN group time of union was 11.8 weeks and only 2 patients got malunion out of 25. A comparison of time to union demonstrated no statistically significant differences between study groups.
Overall functional outcome was measured by Harris Hip Score. Excellent to good results were seen in 88% of patients in PFN group and 60% of DHS group. However, when we compared stable and unstable fracture separately, we found that in case of stable fracture there was no any significant difference in DHS and PFN groups (p value=0.97). While comparing unstable fractures we found that PFN was significantly better than DHS with around 85% patients of PFN group got excellent to good results while only 22% patients of DHS group got excellent to good results. In 2012, Kumar et al [19] carried out study of 50 case of intertrochanteric fracture Operated with PFN and DHS. The results suggestive that the DHS was tolerated well by young patients with stable fracture while PFN had a better outcome with osteoporotic patients and weak bone mass and reverse oblique fractures. In 2019, Hariharan Mohan et al [20] carried out study in 2019 for implant of choice for twopart intertrochanteric fracture. In this study, 54 patients with two parts intertrochanteric fractures were operated with PFN and DHS and functional outcome was calculated with Hip Harris score. At the end of study, they concluded that there is no significant difference between DHS and PFN in simple two-part intertrochanteric fracture. In 2018, Wen-Qiang Zhang et al [21] carried out meta-analysis of total 10 randomized controlled Trials of comparing the intramedullary nail and extra medullary fixation in treatment of unstable intertrochanteric fractures. Results show that intramedullary nail is better option for unstable intertrochanteric fracture with less complication and better functional outcome.
Conclusion
Our study shows that in stable intertrochanteric fractures both PFN and DHS have similar functional outcomes. But PFN is better alternative to DHS especially in the treatment of unstable intertrochanteric fractures and has significantly better functional outcome in terms of earlier restoration of walking ability due to early union and less complications but it is technically difficult procedure and requires more expertise. In addition, PFN requires shorter incision, less blood loss and shorter operative time. It has distinct advantages over DHS even in stable intertrochanteric fractures being a minimally invasive procedure. Hence in our opinion, PFN may be better than DHS for most of the intertrochanteric fractures.
Acknowledgements
This study is dedicated to all my patients, teachers & surgical team members.
Source of Funding
None.
References
- Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res 1990; 252:163–66.
- Kannus P, Parkkari J, Sievänen H et al. Epidemiology of hip fractures. Bone 1996; 18:57–63.
- Utrilla AL, Reig JS, Muñoz FM, et al. Trochanteric gamma nail and compression hip screw for trochanteric fractures: A randomized, prospective, comparative study in 210 elderly patients with a new design of the gamma nail. J Orthop Trauma 2005; 19:229-33.
- Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Systematic Rev 2010.
- Butt MS, Krikler SJ, Nafie S, et al. Comparison of dynamic hip screw and gamma nail: A prospective, randomized, controlled trial. Injury 1995; 26:615-8.
- Bridle SH, Patel AD, Bircher M, et al. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br 1991; 73:330-4.
- Goldhagen PR, O'Connor DR, Schwarze D, et al. A prospective comparative study of the compression hip screw and the gamma nail. J Orthop Trauma 1994; 8:367-72.
- Hoffman CW, Lynskey TG. Intertrochanteric fractures of the femur: A randomized prospective comparison of the gamma nail and the ambl hip screw. Australian New Zealand J Surg 1996; 66:151-5.
- Radford PJ, Needoff M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg Br 1993; 75:789-93.
- Anand J. The elements of fracture fixation. Churchill Livingstone, New York, NY, USA, 1997.
- Pires RE, Santana EO, Santos LE, et al. Failure of fixation of trochanteric femur fractures: clinical recommendations for avoiding Z-effect and reverse Z-effect type complications. Patient Safety Surg 2011; 5:1-6.
- Pavelka T, Matejka J, Cervenková H. Complications of internal fixation by a short proximal femoral nail. Acta Chir Orthop Traumatol Cech 2005; 72:344-354.
- Ahrengart L, Tornkvist H, Fornander P, et al. A randomized study of the compression hip screw and gamma nail in 426 fractures. Clin Orthop 2002; 401:209–22.
- Jensen JS, Michaelsen M. Trochanteric femoral fractures treated with McLaughlin osteosynthesis. Acta Orthop Scand 1975; 46:795–03.
- Dahl E. Mortality and life expectancy after hip fractures.ActaOrthop Scand 1980; 51:163-70.
- Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop 1998; 348:87–94.
- Saudan M, Lubbeke A, Sadowski C, et al. Pertrochanteric fractures: is there an advantage to an intramedullary nail? A randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral n ail. J Orthop Trauma 2002; 16:386-393.
- Menezes, Daniel FA, Gamulin A. Is the proximal femoral nail a suitable implant for treatment of all trochanteric fractures? Clin Orthop 2005; 439:221-227.
- Kumar R, Singh RN, Singh BN. Comparative prospective study of proximal femoral nail and dynamic hip screw in treatment of intertrochanteric fracturefemur. J ClinOrthop Trauma 2012; 3:28-36.
- Mohan H, Kumar P. Surgical treatment of type 31-A1 two-part intertrochanteric femur fractures: Is proximal femoral nail superior to dynamic hip screw fixation? Cureus 2019; 11:e4110.
- Zhang WQ, Sun J, Liu CY, et al. Comparing the intramedullary nail and extramedullary fixation in treatment of unstable intertrochanteric fractures. Scientific Reports 2018; 8:1-8.
Author Info
Vivek Amritbhai Patel, Chintan Bharatbhai Sheth*, Sangeen Bhundiya, Sangeen Bhundiya, Saurabh Rajeshbhai Patel, Adarsh Vishnubhai Patel and Deep Manojbhai Pavani
Department of Orthopaedics, Gujarat Adani Institute of Medical Sciences, Bhuj, Gujarat, IndiaCitation: Vivek Amritbhai Patel, Chintan Bharatbhai Sheth, Sangeen Bhundiya, Sangeen Bhundiya, Saurabh Rajeshbhai Patel, Adarsh Vishnubhai Patel, Deep Manojbhai Pavani,To Compare and Assess Dynamic Hip Screw and Proximal Femur Nail in Intertrochenteric Femur Fracture, J Res Med Dent Sci, 2021, 9(7): 219-224
Received: 27-Apr-2021 Accepted: 12-Jul-2021