Case Report - (2020) Volume 8, Issue 2
The Significance of Oral Radiology for Early Detection of Gardner Syndrome: A Case Report
Saliha Akcay Koprucu1*, Saadettin Kayıpmaz2, Omer Said Sezgin2 and Arif Mansur Cosar2
*Correspondence: Saliha Akcay Koprucu, Specialist in Oral Diagnosis and Maxillofacial Radiology, Turkey, Email:
Abstract
Gardner syndrome is a rare disease with autosomal dominant inheritance characterized by the presence of polyposis coli, multiple osteoma, and mesenchymal tumour in the skin and soft tissue. This study aims at presenting a case of Gardner syndrome together with clinical and radiographic features. A 40 year-old male patient with the chief complaint of toothache was admitted to the Oral and Maxillofacial Radiology Clinic of KTU Faculty of Dentistry. Panoramic radiography obtained from the patient showed the indications of osteomas, which were then supported by the subsequent cone beam computed tomography. The patient was referred to Gastroenterology Clinic with a prediagnosis of Gardner syndrome. After carrying out colonoscopy, polyposis coli were detected. In case of presence of multiple osteomas on patient’s radiographies, it is highly substantial to undertake a GIS examination for Gardner syndrome to search for polyposis coli which necessitates a surgical treatment plan, since polyposis coli is a characteristic feature of Gardner syndrome and has a high malignant potential.
Keywords
Adenomatous polyposis coli, Jaw, Gardner syndrome, Osteoma
Introduction
Gardner syndrome is a hereditary disease characterized by multiple osteoma, multiple enostosis, epidermoid cyst, subcutaneous desmoid tumor and intestinal polyps [1]. This syndrome was first identified in 1951 by Gardner, who demonstrated the correlation between colorectal adenomas, desmoid tumors, bone and soft tissue tumors and colonic polyps prone to malignant degeneration [2].
Familial adenomatous polyposis (FAP) is an autosomal dominant inherited disease characterized by multiple adenomatous polyps in the colon and rectum. In addition to colonic polyps, Gardner syndrome is a different type of familial adenomatous polyposis coli, which is prone to cancers, desmoid tumors, osteomas, epidermoid cysts, various soft tissue tumors, thyroid and periampullary cancers. Even though patients with this syndrome are generally asymptomatic, they may have complaints such as bleeding, diarrhea, abdominal pain and mucous discharge. The diagnosis can be made by means of endoscopy, analysis of extra-intestinal properties and genetic tests [3].
The majority of patients with Gardner syndrome have a family history. On the other hand, 25% of cases may be the first in the family with a new dominant mutation occurring [4]. One of the most significant characteristics of this syndrome are intestinal polyps which are mostly localized in the gastrointestinal tract [5]. Starting to ocur during puberty but developing mostly in the second or third decade of life, the incidence of malignant transformation of these intestinal polyps is approximately 5% in puberty, while it is 100% in patients above 50 years of age [6,7]. The presence of osteomas is essential for the diagnosis of Gardner syndrome. They are most commonly observed in the mandible, but may also occur in the head, paranasal sinuses and long bones [8]. Dental anomalies including multiple impacted- or unerupted teeth, hypodontics, supernumerary teeth, odontoma and dentigerous cysts may be observed in 30% of patients with Gardner's syndrome [9]. Epidermoid cysts are the most frequently observed cutaneous manifestation of Gardner syndrome and may develop multiply in the face, extremities or scalp in 50-60% of patients [10].
The aim in this article was to present a case of Gardner syndrome together with its clinical and radiographic features in order to withdraw attention to its manifestation in the mouth and put emphasis on oral diagnosis for its presence.
Case Description
A 40 year old male patient who had no diseases in his medical and family history was admitted to our clinic with the chief complaint of tooth pain in his right lower jaw. Clinical examination of the patient helped detect a wide-surface amalgam filling and vertical percussion sensitivity in his mandibular right first molar tooth. Panoramic and periapical radiographs revealed insufficient canal treatment in this tooth and a radiolucent area in its periapical.
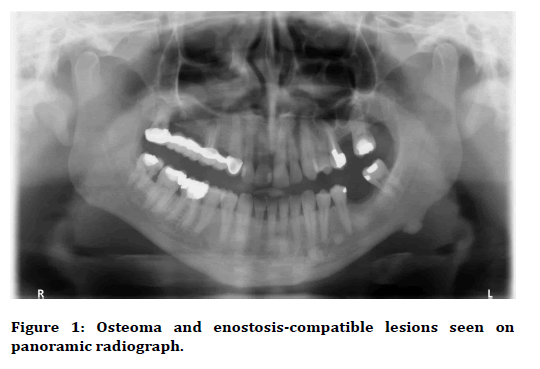
Panoramic image helped observe homogenous radiopaque lesions with regular boundaries in the lower left molar region. In addition, other radiopaque lesions were observed close to the apex of the left mandibular canine, in between the roots of the left mandibular first and second premolar teeth, and distally to the apex of the mandibular left second premolar tooth (Figure 1). The latter lesions were observed to be compatible with idiopathic osteosclerosis.
Figure 1: Osteoma and enostosis-compatible lesions seen on panoramic radiograph.
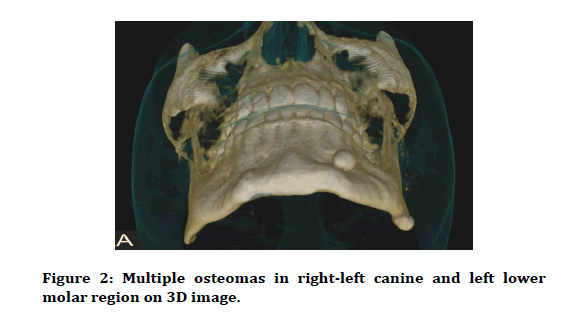
These findings were further supported by cone-beam computed tomography images that indicated the presence of well-circumscribed radiopaque lesions with stalk in the apex of the left mandibular canine tooth and in the left mandibular molar region. Of these, the former was 8 × 5 × 8 mm sized, had a compatible internal structure with bone cortex and was localised on the vestibule side of the bone cortex of the lesion in the apex as attached to the cortex, and the latter was 10 X 6 X 9 mm in size and was observed to have developed from the cortex to the inferior. It was determined that the radiopaque lesions in the left mandibular first premolar and first molar interdental region were enostoses located in the trabecular bone inside the cortex, adhering to the cortex and fused with the trabecular structure. Additionally, a radiopaque lesion, consisting of cortical and spongious bone approximately, 6 mm in width and adhering to the cortex, was observed in the vestibule of the bone cortex in the mandibular right canine tooth region (Figure 2). All of these lesions were thought to be multiple osteomas, and the patient and his family were questioned for gastrointestinal pathologies and no symptoms were detected. The patient was then consulted to Gastroenterology clinic with suspicion of Gardner syndrome.
Figure 2: Multiple osteomas in right-left canine and left lower molar region on 3D image.
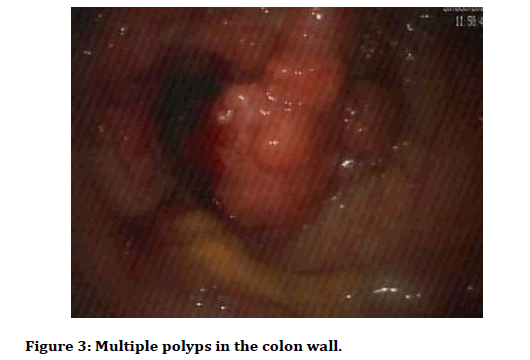
Being larger and dense in the rectum, partially narrowing the lumen, eroded, adenomatous, small ones being usually stalked, while the larger ones sessile and folded numerous dimunitive polyps were detected in all colon segments with colonoscopy. They were found to be getting sparse towards proximal, with mucosa being completely normal (Figure 3).
Figure 3: Multiple polyps in the colon wall.
There was a relative increase in the size and number of polyps observed starting of the proximal of the transverse colon. Numerous polyps were found at the anal canal level. Polyposis coli were reported as a result of histopathological examination of the biopsy performed following the polypectomy of two small stalked polyps. The patient was also consulted to Endocrinology, Ophthalmology and Dermatology clinics. However, no pathology was found in the related examinations. The patient underwent total colonectomy with the diagnosis of Gardner syndrome and he died at the age of 45, five years after the diagnosis, despite all required medical and surgical treatment.
Discussion
Gardner syndrome is a rare genetic disease characterized by the presence of polyposis coli, multiple osteoma, and mesenchymal tumour in the skin and soft tissue. Osteoma and enostoses observed in this syndrome often develop before intestinal polyps and usually occur in the mandible, maxilla, frontal and sphenoid bones [1]. Starting to occur during puberty but developing in the second and third decades of life, polyps are one of the most important characteristics of Gardner syndrome and can be observed in the gastrointestinal tract and in any area other than the oesophagus. The risk of malignant transformation of these polyps is very high for patients after the age of 50 years [5]. Therefore, on radiographic detection of osseous lesions in Gardner syndrome, early identification of polyps before malignant differentiation is of utmost importancy.
In the case presented herein, multiple osteomas were detected in the mandible during the radiographic examination that we preformed and polyposis coli were determined following colonoscopy and histopathology. Even though osteomas are mostly seen in the mandible, they may also be seen in long bones, head and paranasal sinuses. These osteomas are characterized by a round or oval radiopaque mass adhering to a broad base [11]. Enostosis is observed in almost all of the FAP patients with osteoma, and exostoses may be observed in approximately one-third of these patients [12]. In some patients, osteomas may not be present, but the presence of five or more dense bone areas remarks the presence of familial multiple polyposis syndrome [1]. Enostoses are often observed in the premolar-molar region [13].
In this presented case, enostoses in the mandibular left lower region were observed in the premolar-molar region. Two of the osteomas were stalked and oval, while the other one had a broad base.
The clinical diagnosis of Gardner syndrome, sometimes known to be correlated with conditions such as papillary thyroid carcinoma, adrenal adenoma, colorectal adenocarcinoma, thyroid tumours, liver tumours, and less frequently congenital hypertrophy of the retinal pigment epithelium, can sometimes be difficult [14]. While some patients have only one or two anomalies, others may have all the characteristics of the syndrome. It is extremely difficult to diagnose Gardner syndrome in case of the absence of polyp or family information. Therefore, stomach, thyroid, teeth, jaw and eye examination should be performed on each individual with colorectal polyp. It is also recommended to evaluate APC and MYH mutations in the determination of Gardner syndrome despite the uncertainty of the level of diagnosis [15,16].
Conclusion
There were no findings detected other than multiple osteoma, multiple enostosis and polyposis coli in our case. Due to the possibility of the early diagnosis of this syndrome leading to life-saving treatment, it is of utmost importance to carry out the CBCT analysis in case of suspicion of such lesions on plain radiographs, to perform GIS screening for Gardner syndrome on detection of multiple osteoma, and to plan the necessary treatment for patients with polyposis coli.
References
- White SC, Pharoah MJ. Benign tumours of the jaws. Oral Radiology Principles and Interpretation. 6th Edn. St Louis: Mosby 2009.
- Bülow S, Berk T, Neale K. The history of familial adenomatous polyposis. Fam Cancer 2006; 5:213-220.
- Nandakumar G, Morgan JA, Silverberg D, et al. Familial polyposis coli: Clinical manifestations, evaluation, management and treatment. Mt Sinai J Med 2004; 71:384-391.
- Patel H, Rees RT. Unicystic ameloblastoma presenting in Gardner’s syndrome: A case report. Br Dent J 2005; 198:747-748.
- Half E, Bercovich D, Rozen P. Familial adenomatous polyposis. Orphanet J Rare Dis 2009; 4:22-29.
- Oner AY, Pocan S. Gardner’s syndrome: A case report. Br Dent J 2006; 200:666-667.
- Silva CA, MoraesPde C, Furuse C, et al. Gardner syndrome with no clinical family history. J Craniofac Surg 2009; 20:1186-1189.
- Gorlin RJ, Pindborg JJ, Cohen MM. Syndromes of the Head and Neck. 2nd Edn. New York: McGraw-Hill 1976.
- Madani M, Madani F. Gardner’s syndrome presenting with dental complaints. Arch Iran Med 2007; 10:535-539.
- Ascari-Raccagni A, Baldari U, Righini MG. Cutaneous symptoms of gardner's syndrome. J Eur Acad Dermatol Venereol 1999; 12:80–81.
- Bilkay U, Erdem O, Ozek C, et al. Benign osteoma with Gardner syndrome: Review of the literature and report of a case. J Craniofac Surg 2004; 15:506-509.
- Wolf J, Järvinen HJ, Hietanen J. Gardner’s dentomaxillary stigmas in patients with familial adenomatosis coli. Br J Oral Maxillofacial Surg 1986; 24:410–416.
- Offerhaus GJ, Levin LS, Giardiello FM, et al. Occult radiopaque jaw lesions in familial adenomatous polyposis coli and hereditary nonpolyposis colorectal cancer. Gasteroenterol 1987; 93:490–497.
- Juhn E, Khachemoune A. Gardner syndrome skin manifestations, differential diagnosis and management. Am J Clin Dermatol 2010; 11:117-122.
- Ben Lagha N, Galeazzi JM, Chapireau D, et al. Surgical management of osteoma associated with a familial Gardner's syndrome. J Oral Maxillofac Surg 2007; 65:1234-1240.
- Gu GL, Wang SL, Wei XM, Bai L. Diagnosis and treatment of gardner syndrome with gastric polyposis: A case report and review of the literature. World J Gastroenterol 2008; 1413:2121-3123.
Author Info
Saliha Akcay Koprucu1*, Saadettin Kayıpmaz2, Omer Said Sezgin2 and Arif Mansur Cosar2
1Specialist in Oral Diagnosis and Maxillofacial Radiology, Oral and Dental Health Hospital, Trabzon, Turkey2Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, Karadeniz Technical University, Trabzon, Turkey
Citation: :Saliha Akcay Koprucu, Saadettin Kayıpmaz, Omer Said Sezgin, Arif Mansur Cosar, The Significance of Oral Radiology for Early Detection of Gardner Syndrome: A Case Report, J Res Med Dent Sci, 2020, 8(2): 17-19
Received: 01-Feb-2020 Accepted: 28-Feb-2020