Research - (2019) Volume 7, Issue 2
The Relationship between Spiritual Well-being and Family Cohesion in Patients with Thalassemia Major
Yaghoob Madmoli1, Malihe Salimi2, Mostafa Madmoli3, Narjes Davoodi1, Fatemeh Rostami4, Reza Heidari-Soureshjani5 and Najime Yousefi6*
*Correspondence: Najime Yousefi, Gerash Amir-al-Momenin Medical and Educational Center, Gerash University of Medical Sciences, Gerash, Iran, Email:
Abstract
Introduction: This study was conducted to investigate the relationship between spiritual well-being and family cohesion among people with thalassemia Major.
Methods: This cross-sectional study was conducted on 101 patients with thalassemia major of Dezful Large Hospital in 2015. Data were collected by three questionnaires: demographic data, Standard Spiritual Well-being Scale by Daaleman and Frey and Moos Family Cohesion Scale. The data was analyzed using SPSS version 18 statistical test, Pearson correlation and linear regression with a significance level of p<0.05.
Results: The average score of spiritual well-being and self-efficacy subscales were 9.66 ± 34.58 and 9.66 ± 14.68, respectively; which indicates the average level of these variables. Linear regression test results also showed that there was a statistically significant (p<0.05) relationship between spiritual well-being and family cohesion (B=0.25) and between selfefficacy and family cohesion (B=0.24); but there was no significant relationship between life scheme and family cohesion (B=0.16) (p=0.10).
Conclusion: In this study it was observed that a significant direct correlation exists between spiritual well-being and family cohesion. The role of the family as the main supportive institution against the challenges of life is undeniable. Hence, by increasing the level of spiritual well-being of the patients some steps can be taken to promote the cohesion of patients’ families in order to decrease their spiritual and physical problems.
Keywords
Spiritual well-being, Spirituality, Family cohesion, Thalassemia major
Introduction
Thalassemia is a chronic disease [1], caused by the lack or deficiency of one or more polypeptide chains of hemoglobin, which is transmitted generation to generation [2]. The most severe form of this hematological disorder is beta thalassemia major [3,4]. The World Health Organization (WHO), introduced thalassemia as the most common chronic genetic disorder in 60 countries [2] that Iran is at of the high risk areas for the disease [3]. So that, according to the World Health Organization, 4 percent of the population of country is carriers of thalassemia and the number of patients with beta thalassemia major in Iran in 2013 were estimated more than 30 thousand people, while in a populated country like America it is less than 1000. Also, annually approximately 800 people are added to the population of patients with thalassemia [5].
Several reports worldwide indicate that life expectancy in patients with thalassemia is increased considerably and mortality rates significantly decreased with the help of available treatments [6-8]. However, social and psychological problems affect the quality of life in patients and their caregivers [8], more than 80% of people with Thalassemia Major (BTM) suffer from mental disorders [1,9], which produces a wide range of serious clinical and psychiatric challenges for patients and their families [10]. Among the complications caused by the disease that affects patients’ life include changes in bone, short stature, mental retardation [11,12], enlarged liver and spleen, heart failure [13-15], lack of physical growth and fertility [6] and premature death; that not only their physical performance is affected [11], but these can also affect their emotional and social performance [3].
Mental fatigue, well-being and educational performance issues [16], difficulties in playing social roles in society, the inability to raise a family [6], decreased self-esteem, reduced academic achievement [17], weak performance and ultimately low quality of life are the other problems caused by this disease [18]. In these patients, in addition to increased levels of stress [17] including physical and emotional stress, a significant financial stress also affects their families [19]. The patients suffering from BTM are faced to many challenges in which the role of families in providing different types of social support is of considerable importance [20]. This disease can make too much psychological burden for patients and their families [11,21]. Emotional distress, anxiety, fear, problems in dealing with the feelings of patients and its subsequent effects on the normal functioning of the family, are the common problems in families with thalassemia children [9,22].
Having a child with this disease may disrupt family dynamics and cohesion [23] Therefore, psychological support aimed at reducing emotional distress by parents, and strengthened coping strategies for everyday life’s cohesion is required [24]. According to surveys, patients who received more social support from family and other people have had less depression [25,26]. Spiritual wellbeing is an important aspect of human health that the integrated relationship between internal forces and is determined by features like stability in life, peace, balance and harmony and a sense of connection and intimacy with God [27].
As a humanistic dimension of the individual, spirituality has an effective role in improvement and meeting the spiritual needs of patients and their families. Thus, it has gained increasing attention as an essential element of clinical care [28]. In case of disease, spiritual matters make a person to seek meaning and purpose of life, followed by increased spiritual needs [29]. Spiritual wellbeing is the core of human health, and fostering and promoting spiritual well-being can be a way of coping with the disease [30]. Research shows that religious beliefs may affect the overall health or coping with a disease [31,32]. Research conducted by Aydinok et al., showed that family awareness and psychological support leads to better compatibility of patients and reduces depression, obsession and paranoia [33]. Also, according to Kwong et al., the family functioning and social support can have many impacts on emergence of mental disorders or mental health of thalassemia patients [34].
Strengthening the spiritual dimension on the one hand reduces the symptoms of the disease and on the other increases a person's ability to adapt, it also improves mental health and helps to reduce feelings of hopelessness and depression and improves social performance [35]. Mcnulty et al. in a study among patients with multiple sclerosis (MS) found that spiritual beliefs and faith were helpful in coping with the disease [36]. Adegbola’s study showed that the spiritual wellbeing of patients with sickle cell anemia is directly related to their quality of life [37].
Considering the effects of spirituality and dynamism and cohesion of the family in improving the symptoms, and due to the limited research done in this area, the present study was conducted to investigate the relationship between spiritual well-being and family cohesion in patients with thalassemia major in Dezful in 2015.
Materials and Methods
This study is a descriptive analytical study that was conducted after obtaining the relevant permissions from ethics committee of Dezful University of Medical Sciences (DUMS-121) and the informed consent of patients with thalassemia referred to thalassemia major ward of Large Hospital of Dezful. Attainable sampling on eligible patients was used to select the participants. Overall, 125 patients referred to the center that 101 people participated with satisfaction in this study. Inclusion criteria included: patient satisfaction to participate, full awareness about the aims of the project, being literate, and having at least one record of hospitalization. And the exclusion criterion was incomplete questionnaire. Data collection tools included demographic questionnaire, Daaleman and Ferry Spiritual Index of Well-being (SIWB) [38] and Moos Family Cohesion Scale [39].
Demographic questionnaire included age, sex, body mass index, ethnicity, education level, occupation, marital status, monthly income, hospitalization record, and medication usage. SIWB scale is developed by Daaleman et al. [38] to measure the spiritual well-being and is the most famous spiritual well-being assessment scale and contains 12 questions that are designed based on Likert scale of five options. Total scores range from 12 to 60, the higher scores indicate higher spiritual well-being. It consists of two subscales of "self-efficacy" and "life scheme". Each subscale consists of 6 questions. A minimum of 12 and maximum of 60 points are possible that scores between 12 and 24 indicate low spiritual well-being of individuals, and scores between 24 and 36 represent average spiritual well-being and scores more than 36 show high spiritual well-being. In the initial measurement, Cronbach's alpha for the total scale, selfefficacy subscale and life scheme were 0.91, 0.86, and 0.89, respectively [38]. Family Cohesion Scale by Moos et al. [39] includes 9 questions. The range of scores are on two scales of completely true (0) and completely false (1). Reverse items of the questionnaire include items 1, 3, 4, 6, 8 and 9. The points are summed to calculate the total scores of people. The higher score indicates higher cohesion and coherence in a family environment. The minimum possible score was 0 and the maximum was 9 where the scores between 0 and 3 represent lower family cohesion, scores between 3 and 5 show average family cohesion, and score higher than 5 shows good family cohesion.
In terms of correlation reliability, the researcher obtained the reliability of this questionnaire as 0.86 using testretest and 0.78 through internal consistency [40]. To analyze the data SPSS software version 18 and independent t-tests, ANOVA, Pearson correlation and linear regression were used.
Results
The sample included 101 patients with beta thalassemia major with an average age of 5.4 ± 23.22 years. Among these, 60.4% were male and the rest were female; and 82.2% were single, and the rest were married. Table 1 shows the demographics of the sample.
| Item | Percent (%) | Relation with spiritual well-being | Relation with family cohesion | |
|---|---|---|---|---|
| p-value | p-value | |||
| Sex | Male | 60.4 | 0.07 | 0.44 |
| Female | 39.6 | |||
| Marital status | Single | 82.2 | 0.31 | 0.1 |
| Married | 17.8 | |||
| Place of residence | Urban | 66.3 | 0.69 | 0.95 |
| Rural | 33.7 | |||
| Level of education | Illiterate | 2 | 0.83 | 0.58 |
| Under diploma | 41.6 | |||
| Diploma | 38.6 | |||
| Associate degree | 3 | |||
| Graduate and post graduate | 14.9 | |||
| History of hospitalization | Yes | 61.4 | 0.28 | 0.71 |
| No | 38.6 | |||
| History of surgery | Yes | 39.6 | 0.21 | * 0.02 |
| No | 60.4 | |||
| Blood type | A+ | 32.7 | 0.15 | 0.41 |
| A- | 1 | |||
| B+ | 23.8 | |||
| B- | 1 | |||
| AB+ | 5.9 | |||
| AB- | 0 | |||
| O+ | 35.6 | |||
| O- | 0 | |||
Table 1: Demographic characteristics of patients with beta-thalassemia
Table 1 also shows that none of the demographic variables has a statistically significant relationship with spiritual well-being as well as family cohesion (p>0.05).
The average score of spiritual well-being and self-efficacy subscales were 9.66 ± 34.58 and 9.66 ± 14.68, respectively; which indicates the average level of these variables. The mean score of life scheme subscale is 19.8 that indicate its high level. The mean score of family cohesion is 4.63 that is at the average level (Table 2).
| Variable | Categories | N (%) | Mean and SD |
|---|---|---|---|
| Spiritual well-being | Low | 15.8 | 34.58 ± 9.66 |
| Average | 45.6 | ||
| High | 38.6 | ||
| Self-efficacy | Low | 44.6 | 14.68 ± 6.71 |
| Average | 22.7 | ||
| High | 32.7 | ||
| Life scheme | Low | 10.9 | 19.8 ± 5.84 |
| Average | 30.7 | ||
| High | 58.3 | ||
| Family cohesion | Low | 30.7 | 4.63 ± 1.81 |
| Average | 38.6 | ||
| High | 30.7 |
Table 2: Distribution of spiritual well-being, self-efficacy, life scheme and family cohesion in patients with beta-thalassemia
Surgery record and family cohesion has a statistically significant relationship (p=0.02). Thus, those who had surgery had less family cohesion. Other statistical relationships are shown in Table 1.
Linear regression test results also showed that there was a statistically significant (p<0.05) relationship between spiritual well-being and family cohesion (B=0.25) (p=0.009) (Figure 1) and between self-efficacy and family cohesion (B=0.24) (p=0.01); but there was no significant relationship between life scheme and family cohesion (B=0.16) (p=0.10).
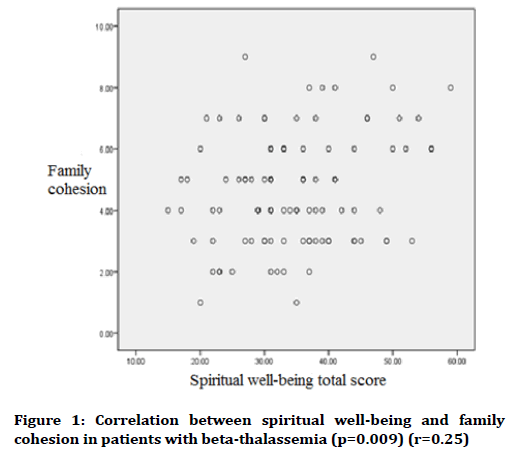
Figure 1. Correlation between spiritual well-being and family cohesion in patients with beta-thalassemia (p=0.009) (r=0.25)
Discussion
Spirituality is one of the important dimensions with a high impact on people’s lives and it includes many personal and social functions [41]. Spiritual achievements in health care have a huge appeal because research has confirmed its potential effect in the prevention, response to or recovery of disease [42]. The total score of spiritual well-being in patients with BTM was obtained as 34.58 ± 9.66 that shows an average level of spiritual well-being in the patients, meanwhile the level of spiritual well-being in dialysis patients is low (13.21) [43]. However, Balboni et al. state high level of spiritual well-being in patients with advance cancer [44].
In this study, self-efficacy subscale score was 14.68 which indicate the average level of this variable. While Sheibani et al. point out the low level of self-efficacy in adolescents with thalassemia [45]. Family cohesion’s mean score was 4.63 which are at the average level that indicates the need to more institutions which increase family cohesion for patients [9].
In this research, family cohesion has been at an average level. Children with thalassemia compared to healthy children have lower quality of life in all aspects that affect the family cohesion [16]. Other studies also support the low quality of life of these children that is the result of factors such as family income, family education regarding the view toward the thalassemic patients that improve patient’s performance [9].
The present study aimed to investigate the relationship between spiritual well-being and family cohesion in patients with thalassemia major. It was observed that a significant correlation exists between spiritual well-being and self-efficacy with family cohesion and patients who had higher spiritual well-being also experienced higher self-efficacy, coherence and family cohesion. In this regard, the study by Viola et al. in Italian Never-Employed Young Adults in 2017 showed that significant positive correlation exists between spiritual well-being and selfefficacy [46]. de Mamani et al. study found that promotion of spirituality will strengthen family cohesion and their compatibility [47]. Mohammadi et al. study on young people with thalassemia major [48] and Adegbola’s study in on patients with sickle cell anemia [37] showed that spiritual well-being increases by higher quality of life of patients. Balboni et al. study on patients in the final stages of life also showed that patients who had higher mental health had less feelings of hopelessness [49]. However, Bussing et al. study on patients with cancer showed moderate correlations between spiritual well-being and quality of life [50]. These results could be evidence of a significant relationship between spiritual well-being and various aspects of human life. Spiritual beliefs are an important part of family life in all communities [41].
Spiritual well-being is an ambiguous and complex process of human evolution that provides a harmonious relationship between internal forces [51]. In this study, the total score of spiritual well-being in patients with thalassemia was obtained 9.66 ± 34.58, indicating a moderate level of spiritual well-being in these patients. Patients had moderate spiritual well-being in Mohammadi et al. study on young people with thalassemia major, Nsamenang et al. study on patients with multiple sclerosis [48,52]. While, Ebrahimi et al. found that the level of mental health in hemodialysis patients was low (10.20), respectively [43] and in a study by Balboni et al. on patients with advance cancer, a high level of mental health was reported [44]. In the present study, no significant relationship between sex and spiritual well-being was found (p=0.07) that is in line with Bussing et al. [50]. In the present study, no significant relationship between education and spiritual well-being was found. However, the study by Hasanshahi et al. concluded that teaching spirituality is an important factor in promoting spiritual well-being [41].
Conclusion
According to findings it can be concluded that spiritual well-being has a significant role in consistency and cohesion of families of patients with thalassemia major. Given that the health care of these patients impose heavy costs on families and having children with such a disease in the family influences family cohesion, it is suggested that public health officials plan training programs to strengthen the spiritual well-being of these patients and their families, because by increasing the levels of spiritual well-being of the patients they take steps to promote family cohesion which has a significant role in reducing the patient's mental and physical problems. Meanwhile, family cohesion, and spiritual well-being of these individuals play an important role in predicting their efficacy. Therefore, health system planners should pay special attention to developing educational programs for these patients.
The major limitation of this study was to collect data at one period of time, excluding the illiterate and the limited number of previous studies on patients with thalassemia major. To further explore the relationship between spiritual well-being and the family cohesion it is recommended that more studies are done in this area.
Acknowledgments
Researchers express their appreciation and thanks to the patients with thalassemia, nurses and personnel of Thalassemia major ward, authorities of Dezful Large Hospital, deputy and personnel of Dezful University of Medical Sciences.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Naderi M, Hormozi MR, Ashrafi M, et al. Evaluation of mental health and related factors among patients with beta-thalassemia major in South East of Iran. Iran J Psychiatry 2012; 7:47-51.
- Baghianimoghadam MH, Sharifirad G, Rahaei Z, et al. Health related quality of life in children with thalassaemia assessed on the basis of SF-20 questionnaire in Yazd, Iran: A case-control study. Cent Eur J Public Health 2011; 19:165-9.
- Yengil E, Acipayam C, Kokacya MH, et al. Anxiety, depression and quality of life in patients with beta thalassemia major and their caregivers. Int J Clin Exp Med 2014; 7:2165-72.
- Madmoli Y, Akhaghi DS, Beiranvand R, et al. An epidemiological and clinical survey of patients with β-thalassemia in Dezful in 2015. IRJE 2017; 13:145-52
- Madmoli Y, Beiranvand R, Korkini N, et al. Comparison of health-related quality of life in beta thalassemia major and healthy people in Dezful in 2015. IJNR 2016; 11:9-16.
- Haghpanah S, Nasirabadi S, Ghaffarpasand F, et al. Quality of life among Iranian patients with beta-thalassemia major using the SF-36 questionnaire. Sao Paulo Med J 2013; 131:166-72.
- La-Nasa G, Caocci G, Efficace F, et al. Long-term health-related quality of life evaluated more than 20 years after hematopoietic stem cell transplantation for thalassemia. Blood 2013; 122:2262-70.
- Safizadeh H, Farahmandinia Z, Nejad SS, et al. Quality of life in patients with thalassemia major and intermedia in Kerman-Iran (IR). Mediter J Hematol Infect Dis 2012; 4:e2012058.
- Ayoub MD, Radi SA, Azad AM, et al. Quality of life among children with beta-thalassemia major treated in Western Saudi Arabia. Saudi Med J 2013; 34:1281-6.
- Salama H, Hussein H, Al-faisal W, et al. Health-related quality of life in transfusion-dependent thalassemia major patients and associated factors in Dubai, UAE, 2011. Middle East J Psychiatr Alzheimers 2014; 5:3-10.
- Thavorncharoensap M, Torcharus K, Nuchprayoon I, et al. Factors affecting health-related quality of life in Thai children with thalassemia. BMC Blood Disord 2010; 10:1-10.
- Ali SS, Tarawah AM, Al-Hawsawi ZM. Comprehensive patient care improves quality of life in transfusion dependent patients with β-thalassemia. Saudi Med J 2015; 36:575-9.
- Lyrakos GN, Vini D, Aslani H, et al. Psychometric properties of the specific thalassemia quality of life instrument for adults. Patient Prefer Adherence 2012; 6:477-97.
- Amoudi AS, Balkhoyor AH, Abulaban AA, et al. Quality of life among adults with beta-thalassemia major in western Saudi Arabia. Saudi Med J 2014; 35:882-5.
- Tari K, Valizadeh AP, Abbaszadehdibavar M, et al. Thalassemia an update: Molecular basis, clinical features and treatment. Int J Biomed Public Health 2018; 1:48-58.
- Kaheni S, Yaghobian M, Sharefzada GH, et al. Quality of life in children with β-thalassemia major at center for special diseases. Iran J Ped Hematol Oncol 2013; 3:108-13.
- Jain M, Bagul AS, Porwal A. Psychosocial problems in thalassemic adolescents and young adults. CHRON 2013; 4:21.
- Hoch C, Gobel U, Janssen G. Psychosocial support of patients with homozygous beta thalassemia. Klin Pediatrics 2000; 212:216-9.
- Atkin K, Ahmad WI. Family care‐giving and chronic illness: How parents cope with a child with a sickle cell disorder or thalassaemia. Health Soc Care Community 2000; 8:57-69.
- Toljamo M, Hentinen M. Adherence to self-care and social support. J Clin Nurs 2001; 10:618-27.
- Gollo G, Savioli G, Balocco M, et al. Changes in the quality of life of people with thalassemia major between 2001-2009. Patient Prefer Adh 2013; 7:231-6.
- Yahia S, El-Hadidy MA, El-Gilany AH, et al. Predictors of anxiety and depression in Egyptian thalassemic patients: A single center study. Int J Hematol 2013; 97:604-9.
- Mazzone L, Battaglia L, Andreozzi F, et al. Emotional impact in β-thalassaemia major children following cognitive-behavioural family therapy and quality of life of caregiving mothers. Clin Pract Epidemiol Ment Health 2009; 5:5.
- Anum J, Dasti R. Caregiver burden, spirituality, and psychological well-being of parents having children with thalassemia. J Religion Health 2016; 55:941-55.
- Reid V, Meadows-Oliver M. Postpartum depression in adolescent mothers: An integrative review of the literature. J Pediatr Health Care 2007; 21:289-98.
- Bai YL, Chiou CP, Chang YY, et al. Correlates of depression in type 2 diabetic elderly patients: A correlational study. Int J Nurs Stud 2008; 45:571-9.
- Jafari N, Farajzadegan Z, Zamani A, et al. Spiritual well-being and quality of life in Iranian women with breast cancer undergoing radiation therapy. Support Care Cancer 2013; 21:1219-25.
- Lemmer C. Teaching the spiritual dimension of nursing care: A survey of U.S. baccalaureate nursing programs. J Nurse Educ 2002; 41:482-90.
- Tiew LH, Creedy DK. Development and preliminary validation of a composite spiritual care-giving scale. Int J Nurs Stud 2012; 49:682-90.
- Ross L, Giske T, Van LR, et al. Factors contributing to student nurses'/midwives' perceived competency in spiritual care. Nurse Edu Today 2016; 36:445-51.
- Heo GJ, Koeske G. The role of religious coping and race in alzheimer’s disease caregiving. J App Gerontol 2013; 32:582-604.
- Schillings MK. Spiritual support as coping among Alzheimer's caregivers. Master's Thesis, Louisiana State University and Agricultural and Mechanical College 2012; 734.
- Aydinok Y, Erermis S, Bukusoglu N, et al. Psychosocial implications of thalassemia major. Pediatr Int 2005; 47:84-9.
- Kwong EW, Kwan AYH. Stress-management methods of the community-dwelling elderly in Hong Kong: Implications for tailoring a stress-reduction program. Geriatric Nurs 2004; 25:102-9.
- Zeighami MS, Tajvidi M. Relationship between spiritual well-being with hopelessness and social skills in Beta-thalassemia major adolescents. Modern Care J 2011; 8:116-24.
- Mcnulty K, Liveneh H, Wilson LM. Perceived uncertainty spiritual well-being and psychosocial adaptation in individuals with multiple sclerosis. Rehabil Psycho 2004; 49:91-9.
- Adegbola M. Spirituality, self-efficacy, and quality of life among adults with sickle cell disease. South Online J Nurs Res 2011; 11:5-12.
- Daaleman TP, Frey BB. The spirituality index of well-being: A new instrument for health-related quality of life research. Ann Fam Med 2004; 2:499-503.
- Moos RH, Moos BS. Family environment scale manual and sampler set: Development, applications and research. Mind Garden, Inc., Palo Alto, CA 2009.
- Fok CCT, Allen J, Henry D, et al. The brief family relationship scale: A brief measure of the relationship dimension in family functioning. Assessment 2014; 21:67-72.
- Hasanshahi M, Amidi MM. The effects of education on spirituality through virtual social media on the spiritual well-being of the public health students of Isfahan University of medical sciences in 2015. IJCBNM 2016; 4:168-75.
- Koenig HG, Larson DB, Larson SS. Religion and coping with serious medical illness. Ann Pharmacother 2001; 35:352-9.
- Ebrahimi H, Ashrafi Z, Eslampanah GH, et al. Relationship between spiritual well-being and quality of life in hemodialysis patients. J Nurs Midwifery Sci 2014; 1:41-8.
- Balboni TA, Paulk ME, Balboni MJ, et al. Provision of spiritual care to patients with advanced cancer: Associations with medical care and quality of life near death. J Clin Oncol 2010; 28:445-52.
- Sheibani B, Parvizi S, Haghaani H, et al. The self-efficacy of adolescents with major thalassemia and its influencing factors in Bandar Abbas. Iranian J Pediatr Nurs 2015; 1:26-33.
- Viola MM, Musso P, Ingoglia S, et al. Relationships between career indecision, search for work self-efficacy, and psychological well-being in Italian never-employed young adults. Europe’s J Psychol 2017; 13:231-50.
- de Mamani AGW, Tuchman N, Duarte EA. Incorporating religion/spirituality into treatment for serious mental illness. Cogn Behav Pract 2010; 17:348-57.
- Mohammadi S, Tajvidi M, Ghazizadeh S. The relationship between spiritual well-being with quality of life and mental health of young adults with beta-thalassemia major. Sci J Iranian Blood Transfusion Org 2014; 11.
- Balboni MJ, Sullivan A, Amobi A, et al. Why is spiritual care infrequent at the end of life? Spiritual care perceptions among patients, nurses, and physicians and the role of training. J Clin Oncol 2013; 31:461.
- Bussing A, Ostermann T, Mattheiessen P. Adaptive coping and spirituality as a resource in cancer patients. Breast Care 2007; 2:5-7.
- Hajiesmaeili MR, Abbasi M, Safaiepour L, et al. Spiritual health concept in Iranian society: Evolutionary concept analysis and narrative review. J Med Ethics 2016; 10:77-115.
- Nsamenang SA, Hirsch JK, Topciu R, et al. The interrelations between spiritual well-being, pain interference and depressive symptoms in patients with multiple sclerosis. J Behav Med 2016; 39:355-63.
Author Info
Yaghoob Madmoli1, Malihe Salimi2, Mostafa Madmoli3, Narjes Davoodi1, Fatemeh Rostami4, Reza Heidari-Soureshjani5 and Najime Yousefi6*
1Student Research Committee, Dezful University of Medical Sciences, Dezful, Iran2School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
3Emergency Medical Technician, Dezful University of Medical Sciences, Dezful, Iran
4Student Research Committee, Shoushtar Faculty of Medical Sciences, Shoushtar, Iran
5Students Research Committee, Shahrekord University of Medical Sciences, Shahrekord, Iran
6Gerash Amir-al-Momenin Medical and Educational Center, Gerash University of Medical Sciences, Gerash, Iran
Citation: Yaghoob Madmoli, Malihe Salimi, Mostafa Madmoli, Narjes Davoodi, Fatemeh Rostami, Reza Heidari-Soureshjani, Najime Yousefi, The relationship between spiritual well-being and family cohesion in patients with thalassemia major, J Res Med Dent Sci, 2019, 7(2): 203-209.
Received: 20-Mar-2019 Accepted: 22-Apr-2019
