Research - (2019) Volume 7, Issue 2
The Evaluation of the Average of Horizontal Angle of the Condylar in the Axially Plan in Patients with Degenerative Joint Disease of the Temporomandibular Joint (DJD of the TMJ)
F Ezoddini Ardakani1, Yaser Safi2 and Mahjube Entezar-e-ghaem1*
*Correspondence: Mahjube Entezar-e-ghaem, Faculty of Dentistry, Department of Oral and Maxillofacial Radiology, Shahid Sadoughi University of Medical Sciences, Iran, Email:
Abstract
Introduction: The temporomandibular joint (TMJ), like other joints, is exposed to a variety of injuries and, as a result it affects the DJD (Degenerative Joint Disease). DJD is the most common disease associated with joints, which is diagnosed by observation of some clinical symptoms associated with bone changes using computer tomography imaging (CT). CBCT is one of the most suitable methods for dental purposes. Considering the occurrence of condylar morphological changes in DJD and its observation in CBCT images, in this study, the mean of horizontal condyle angle in the axillary plane in TMJ was investigated using CBCT images.
Materials and Methods: In this retrospective cross-sectional study, 80 CBCT images of 40 patients with bilateral DJD (group A) and control patients with no DJD-affected (group B) choose from the archives of CBCT images of patients referred to the private radiology center. The CBCT images of the patients were evaluated by on demand software in the axial view, the coronal plane was drawn perpendicular to the midsagittal plane, and angle between the long axis of the condylar and the coronal plane was considered as the horizontal condyle angle. The mean of angles in both control and patient groups was compared using t-test.
Results: The results of this study showed that there is no significant difference between the horizontal angle of the right and left condyles in group A (patients who are affected by DJD disorder) and B (people who are not affected by DJD disorder). It was also shown that the mean of horizontal condyle angle between the groups A (DJD) and B (Non-DJD) was not significantly different between men and women on both sides. In the present study, the mean of horizontal condyle angle in both sides was investigated in the age group of 18 years-34 years and 35 years-74 years. The results showed that the mean of horizontal condyle angle was not significantly different between the age groups.
Conclusion: The horizontal condyle angle was not significantly different between the two groups with DJD and the nonaffected group. Additionally, there was no significant difference between patients and non-patients in any of the sex and age groups.
Keywords
Horizontal condyle angle, Degenerative joint disease, Temporomandibular joint, Cone beam computed tomography
Introduction
Temporomandibular Joint is a unique and complex joint in the human body due to its anatomical and functional characteristics. The anatomical morphology of the TMJ's skeletal structure undergoes remodeling over the lifetime. Condyle of mandible is one of the major skeletal components of TMJ and one of the growth regions of the mandible at the age of growth. Therefore, its morphological appearance undergoes changes throughout life. Condylar morphology is a bony prominence characterized by an upper and oval bilateral convex surface in an axillary plan, so that the anterior-posterior (lateral) length is typically shorter than the medio lateral (frontal) width [1]. For example, the condylar size and its anterior-posterior angles increase in childhood as the age grows and its shape changes from round to oval. The multidimensional structure of condylar becomes somewhat smooth. However, studies have shown that congenital radiographic abnormalities are more likely to increase with age, and the prevalence and severity of degenerative changes are higher in older people [1]. In addition to physiological conditions, other factors, such as DJD disease, can lead to condylar remodeling. Local DJD is an inflammatory disorder [2] characterized by signs include joint degeneration, bone proliferation, and joint degeneration with bone erosion while the formation of a new bone in the articular surfaces (osteophyte) and in the subchondral region (sclerosis) indicates bone proliferation [3]. TMJ structures can be displayed using panoramic transcranial radiographs, CT, TMJ tomography, CBCT, MRI and arthrography. CT is an optional method to examine the cortical bone contour and TMJ dynamics, although CT is costly and requires a high dose of radiation. Cone-beam computed tomography (CBCT) is less costly and less radioactive. The CBCT provides a three dimensional visualization of maxillofacial minerals with minimal distortion and can be used to detect multiple bone changes. The CBCT provides the most detail with excellent precision of bone structures [1].
DJD (Degenerative Joint disease] is observed with 8%-16% prevalence in the population. The prevalence of this disease increases with age [3,4]. Among the common diseases, the prevalence of DJD is 31.7% (the most common articular disease) and its prevalence is 68.3% among female with articular disorders [5]. A variable combination of analysis and proliferation usually occurs, but usually one of them is more. Degeneration is more common in acute illness, while in chronic disease it is more proliferative. When a force exceeds the ability to fit into the joint, the DJD is created. Although factors such as acute trauma, increased clearance and other malignant factors are also important. Joint internal derangement may be considered as an etiologic factor, but there is a controversy about this [6,7]. DJD can occur at any age, but the risk of developing it also increases with age. DJD is more common in female than males. The disease may be asymptomatic, or patients may complain of signs and symptoms of disorder in TMJ function including pain when touched and moving, joint sound (crepitus), move limitation and muscle spasm. The onset of symptoms may be sudden or gradual. Symptoms may disappear spontaneously and only occur in recurrence episodes. Some studies have reported that the DJD is finally extinguished and symptoms are disappeared or significantly reduced in severity in chronic illness [6,7].
In radiographic images, the joint space may be narrow or disappear when the patient's mouth is completely closed (the teeth are in the occlusion). Previous remodeling symptoms, such as flattening and subchondral sclerosis, may be caused. However, degenerative changes may cause these symptoms to disappear. Lack of cortex or erosion of condylar articulated levels or temporal components (or both) are DJD specification [6,7]. In some cases, the radiolucent areas are rounded, small with regular margins as well as variable density in the profound articulated levels. These lesions are called Ely cyst [6,7]. With the continuing illness, bone proliferation occurs in the articulated levels, which increases the area of the articular surface. This new bone is called osteophyte. In severe cases of DJD, the fossa glenoid may be enlarged vastly, due to the erosion of the posterior slope of the articular prominence and the condyle size is likely to be significantly reduced. The above factors cause the condylar deformation so that the mandible head moves forward and upper to the abnormal anterior position. These factors lead to an open anterior bite [6,7]. Lim et al. examined the patients' condylar with degenerative disorders by panoramic imaging and TMJ panoramic. CBCT imaging was not used in this study [7,8].
Honey et al. reported that CBCT was more reliable than panoramic and TMJ linear tomography for the examination of condylar cortical erosion [9,10]. Winocur et al. tried to detect DJD disorder by clinical symptoms and panoramic imaging, and no CBCT imaging was used [11,12]. Nasseh et al. investigated the joints with TMJ disorder from coronal and sagittal vision in CBCT images, and the examination of the axial profile, especially in terms of horizontal angle, was not carried out [12,13]. Imanimoghaddam et al. compared the bone changes induced by aestheartrate with the disc displacement in CBCT in the axial, sagittal, and coronal view. In this study, the angular variations of the condylar were not investigated [14,15]. Kaimal used panoramic and MRI to examine a joint with DJD disorder and CBCT imaging was not used [16,17]. Al-Rawi et al. examined the CBCT image of 70 people 38 males and 32 females with an average age of 26.4 years of which 35 people had TMD and 35 others were not affected to assess the condylar spatial locations by several parameters. Their results showed that the parameters of the upper space of the joint, the lateral space of the joint, the distance between the A-P and the M-L of the Condylar were significantly different in males and females of the both groups. They also reported that the condylar angle in the axial view in males and females in the patient group was smaller than the control group [18]. Koç evaluated CBCT images of 50 patients aged 25 years-76 years old to compare the horizontal angle of the condylar between the adenotulous and dentulous, as well as the relationship between this parameter with age and gender. The results of this study showed that the gender of patients, dental conditions, and age had no effect on the horizontal angle of the condylar [19]. Despite the description of the CBCT's abilities to evaluate TMJ bone changes, so far, few studies have been conducted using this technique to evaluate temporomandibular changes in the relationship of condylar morphological changes associated with DJD disease. Therefore, the purpose of this research was to assess the mean of the condylar horizontal angle in the axial plan of CBCT images of people with DJD (Degenerative Joint Disease) in the temporomandibular joint.
Materials and Methods
In this retrospective cross-sectional study, 40 CBCT images of patients with bilateral TMJ degenerative Joint disease (osteoarthritis) and 40 CBCT images of people without this disorder (totally 80 condylar in each group) who were referred to a private clinic were investigated. Sampling was done through simple random sampling method. The group with DJD was named as Group A and the group that was not affected was named as Group B or control group. The two groups were attempted to be identical in terms of age and gender. Group A included 24 males and 16 females with age range of 18 years-73 years old and Group B included 16 males and 24 females with age range of 18 years-70 years old. Patients in group A referred to facial surgeon due to TMJ dysfunctional clinical symptoms such as pain in the touch and movement, cryptosus, muscle limitation and muscle spasticity. The surgeon referred patients to a private clinic for CBCT imaging for accurate diagnosis. Two radiologists examined the archives individually, and DJD was detected if they observed the signs include erosion of the condyle, osteophytes, subchondral sclerosis and subchondral cyst in the coronal and sagittal and 3D views. Images approved by both radiologists were selected as samples. The patients had bilateral DJD disorder as a sample.
Group B patients included patients who were referred by the ENT specialist to examine the problem of facial sinuses. These patients did not have DJD symptoms in the 3D, coronal, and sagittal images. This group was considered as the control group. Both the condyles of these individuals were irrelevant to the DJD disorder.
The inclusion criteria of the study were:
1. Patients aged 18 years old or older (for the development of TMJ joint corticalization)
2. Patients without systemic, metabolic, and developmental diseases
3. Patients without pathological lesions involving the condylar such as a tumor or synovial chondromatosis (listed because of an outbreak)
4. Bilateral condylar disorder with DJD in the affected group
5. Aggregation of degenerative joint disease by two radiologists
In this study, the CBCT imaging device was used with the commercial brand of Sordex Scanora 3D, made in Finland (Helsinki) with a FOV of 7.5 cm in 10 cm and a 200 micron voxel size. The exposure condition is 90 kVp and the intensity is 8 mA. The exposure time of the device for images was 16 seconds.
CBCT images were considered using the Ondemand software in the axial view with the maximum length of mandible condylar medio lateral as the condylar long axis. The plan that connects ANS Landmark to the PNS with the sagittal Plan in the axial view was considered as the midsagittal plan (Figure 1).
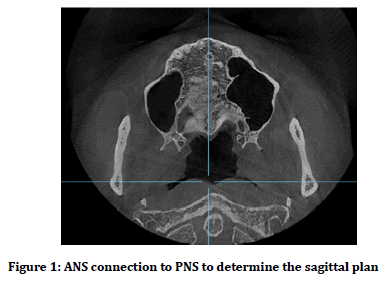
Figure 1. ANS connection to PNS to determine the sagittal plan
The coronal plan was drawn in the axial plane perpendicular to the midsagittal plane. The horizontal angle of the condylar in the axial plane was considered as the angle between the long axis of the condylar and the coronal plane (Figure 2).
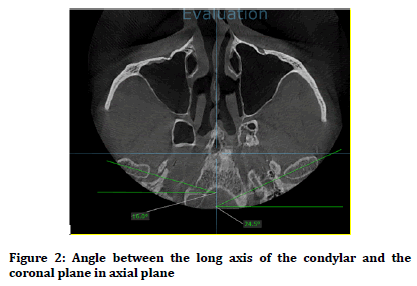
Figure 2. Angle between the long axis of the condylar and the coronal plane in axial plane
The main observer measured the horizontal angles of left and right condyles in groups A and B, 3 times within a week between each measurement. Each measurement step was separate from the preceding step, and the previous number was not seen. The average of these six numbers was calculated and considered as the horizontal angle of the condylar of each patient. In order to establish inter observer reliability in the study, 10 radiographs from each group were randomly selected by the second observer and the angles were calculated in the same way as the first observer. In the case of match between the observers, the numbers imported to the SPSS 22 software. In the case of non-conformance, the third observer measured these numbers, and the number nearest to the calculated number was close to the third observer. The mean angles were compared in both control and patient groups. Lee et al. method was used in measuring the angles [20]. The data were analyzed by SPSS software using appropriate parametric tests. Tables and indicators were prepared and statistical analysis was performed using t-test. It should be noted that the significance level in all tests was considered 0.05 and pvalue <0.05 was statistically significant.
Results
In this study, 80 CBCT images of 80 subjects in two groups of 40 (totally 80 condylar in each group) were studied. The first group (group A) was affected by DJD and the second group (group B) was not affected. A total of 40 CBCT images were selected by simple random sampling from the archives of CBCT images of patients in a private jaw and radiology clinic in Yazd. These images were related to male and female patients who had referred to the dentist (often maxillofacial surgeon) due to the complaints of having symptoms TMJ including pain when touched and moving, joint sound (crepitus), motor limitation, and muscle spasm and CBCT imaging of the temporomandibular joint was prescribed by the dentist. Confirmation of DJD in the condylar of these individuals was carried out by a prominent maxillofacial radiologist and a less experienced radiologist based on the radiographic symptoms of the disease (including remodeling symptoms such as flattening and subchondral sclerosis, osteophyte, Ely cyst). In addition, 40 other Cone-beam computed tomography (CBCT) were obtained from individuals in which DJD disease was not approved by a radiologist after examining CBCT radiography images. These people were usually referred by ENT specialists to examine their sinus problems.
The frequency distribution of individuals in terms of gender in group A (group of patients) was 24 male (60%) and 16 female (40%). Meanwhile, there were 16 male (40%) and 24 female (60%) in Group B. Also, the frequency distribution of the whole participants were 40 male (50%) and 40 female (50%). The relationship between the number of males and females of the two groups was tested by Chi-square test with a p-value as much as 0.074, which is not significant, indicating that the two groups were gender-identical.
The mean age of group A was 15.04 years ± 35.3 years. The minimum age for this group was 18 years and the maximum age was 73 years old. It should be noted that the age of 37 patients was examined from 40 patients (the age of three patients was not recorded in the data due to lack of completion of the case). However, the mean age in group B was 12.9 years ± 8.8 years. The minimum age for this group was 18 years, and the maximum age was 70 years old. T-test was used to examine the difference between the two groups in terms of age, which was not significant (p-value=0.435). In other words, the studied groups were similar in age.
The subjects in both groups were examined for the mean horizontal angle of the right and left condyles in the axial plan.
The upper limit of the horizontal angle of the right condylar in group B was 28 and its lower limit was 19.21 with a confidence level 95%. Meanwhile, upper limit of the horizontal angle of the right condylar in group A was 25 and its lower limit was 23.65 with a confidence level 95%. t-test was used to compare the difference between the two groups A and B in terms of mean horizontal angle of the right condylar and this difference was not significant for the two groups (p-value=0.672).
The upper limit of the horizontal angle of the left condylar in group B was 26.3 and its lower limit was 21.65 with a confidence level 95%. Meanwhile, upper limit of the horizontal angle of the left condylar in group A was 26.1 and its lower limit was 20.1 with a confidence level 95%.
t-test was used to compare the difference between the two groups A and B in terms of mean horizontal angle of the left condylar and this difference was not significant for the two groups (p-value=0.891).
Generally, the difference in horizontal angle of the condyle in the axial plan was not statistically significant for the two groups A and B, but some were more in unaffected subjects.
Discussion
The temporomandibular joint (TMJ), like other joints, is exposed to a variety of harmful processes. These damages can be the result of excessive use of TMJ or systemic disorders (such as rheumatoid arthritis, spondyloarthropathies, and gout). In spite of the type of mechanism that causes this damage, TMJ damage causes disorder in its activity (such as dynamic disorder or reduction and causing pain in the joint), which is referred to as DJD [21].
The prevalence of DJD in TMJ largely depends on the diagnostic criteria, the studied population, and the tools and parameters necessary to evaluate the TMJ [22]. Some studies have reported that the prevalence of the disease as much as 8% to 16% [3,22,23]. Other studies have shown that structural changes in TMJ can be found in 35%-94% of people with at least one symptom [7,24,25].
Research Diagnostic Criteria Committee for temporomandibular disorders (RDC/TMD) identified the first stage in the diagnosis of TMJ or DJD osteoarthritis in clinical symptoms such as decreased mandibular movement, joint pain, and joint sounds. The committee considers CT necessary for imaging bone changes including sub condylar cyst, bone loss, sclerosis, or osteophyte formation to confirm the diagnosis of the disease (at least one of these changes in radiographic images) [9,26]. Bone changes in DJD are more accurate in CT images. Despite the importance that CT images have in diagnosing DJD, the use of it among the dental community was not widely welcomed due to the high cost of this device, the high dosage imposed on the patient and the need for more 3D images in various fields, such as trauma, implants, bone pathological findings, etc. Replacing the method that has the physical and emotional comfort for patients is always a concern for dentists [12].
One of the methods that have attracted the attention of researchers in this field is the use of cone-beam computed tomography (CBCT). Compared with CT, CBCT is less expensive and less radioactive. The CBCT provides a three dimensional image of maxillofacial mineralized tissues with the least distortion, which can be useful in detecting bone changes. The CBCT provides the most detail with excellent precision of bone structures [1]. Therefore, the use of CBCT images in detecting the condylar morphological changes and the subsequent diagnosis of DJD can be important. Identifying these morphological changes in the condylar is a qualitative diagnostic criterion, and the need to use quantitative variables to examine bone changes and identify DJDs is felt.
One of the quantitative markers related to the condylar morphology is the horizontal angle of the condyle, which is referenced in the axial representation to the angle between the long axis of the condylar and the coronal plane perpendicular to the sagittal plane. As previous studies have shown, there are some clinical signs associated with TMJ disorders [27]. Accordingly, the horizontal angle of the condylar was evaluated using 80 images of the CBCT and the mean angles were evaluated between the two groups.
In a study by Lim et al. which evaluated the distribution of patients with degenerative disorders in the mandible condylar, and also evaluated the clinical features of these patients, it was shown that TMJ 607 panoramic images of TMD patients were divided into two groups DJD and non- DJD patients were 37% in the DJD group and 63% in the non-DJD group. In the group with DJD, the number of women (80.8%) was higher than the non-affected group (67.5%). The DJD group had a high incidence in the second and third decades [26]. As it is known, the above mentioned study shows the clinical distribution and distribution of DJD in both age groups and both sexes. In the present study, the aim was not to compare a quantitative parameter of condylar in DJD patients and compare it with those who were not involved in this disease. Accordingly, the design of the study was such that the effect of gender and age was not eliminated by choosing individuals in gender and age groups that did not have significant differences in distribution.
In another study in, Winocur et al. attempted to detect DJD impairment by clinical signs and panoramic imaging. In this study, they studied 372 patients with TMD. Panoramic radiography generally had no diagnostic value in 94.4% of cases and clinical symptoms in 90% of cases could not correctly identify DJD. This study raises doubts about the effectiveness of clinical symptoms and the use of panoramic radiography to diagnose DJD [11]. As the present study suggests, the use of advanced imaging methods such as CBCT seems to be more promising in assessing clinical features and recognizing the parameters involved in the disease in DJD patients. Accordingly, CBCT images were used to evaluate the desired parameter in this study.
In a study, Wiberg et al. showed that bilateral DJD (with a prevalence of 74%) had a higher prevalence compared to one-way (26% prevalence) [27]. In a similar study on bilateral DJD patients, Nasseh et al. examined joint TMJ disorders in the coronal and sagittal view of CBCT images. In their study, 160 TMJ patients (bilaterally in the form of 320 CBCTs) were normal in their study of TMJs in 147 cases, 83 had mild DJDs, and 42 had severe DJDs. 80 of these images had broadening in the mandibular head, and osteophyte was observed in 56 cases [13].
In the present study, the horizontal angle of the condyles on the left and right sides was studied in groups A (DJD) and B (Non DJD). In both studies, CBCT images were used to examine patients with DJD. In both studies, patients with DJD were bilateral, but the study by Nasseh et al. compared the incidence of this disorder to severity with regard to qualitative symptoms such as osteophyte and broadening Condylar head was examined, but in the present study, quantitative features such as the horizontal angle of the condylar were used to check this disorder. A study by Imanimoghaddam et al. compared bone changes in osteoarthritis with CBCT in axial, digital, and coronal lesions. In this study, 45 patients including 37 women and 8 men (aged 18 years-89 years) were studied. Patients were selected based on RDC/TMD criteria. CBCT images were evaluated in sagittal, coronal and axial images to evaluate bone changes including broadening, sclerosis, erosion and osteophyte formation. It was shown that osteochondroscopic osteochondrosis pattern varies with disk displacement. Most of these changes were concentrated in the various condyles [14]. In this study, the horizontal angle of the condyles on the left and right sides was studied in groups A (DJD) and B (Non DJD). This study, which was performed on DJD patients via CBCT images and also a study in Iranian society, was similar to the present study and showed that bone changes in DJD disease have an effect on the change in the condylar morphology, although in this study changes Condylar angles were not investigated but qualitative features such as osteophytes, sclerosis and erosion were investigated in patients with TMD.
Lee et al. studied CBCT images of 60 patients with osteoarthritis (with unilateral condylar involvement) and 43 non-affected individuals who did not have any condylar involvement (control group) [20]. Accordingly, in the Lee et al. study, CBCT images of patients included 60 images of joints involved in osteoarthritis and 60 images of non-involved joints. The CBCT images of the control group included 43 images of one of the joints (in the control group of both non-involvement joints). The mean horizontal angle of the condylar was evaluated in two levels: One case comparison of horizontal angles of condyles of one side of the control group and noninvolved joints in the patients with osteoarthritis was compared and it was shown that there was no significant difference between them [20]. The second level, conducted by Lee et al., was the comparison of mean horizontal angle of the condylar in the patient group between the involved and non-involved joints. The results showed that the mean horizontal angle of the condylar in the joint involved in osteoarthritis in the patients was significantly greater than non-involved joints [20]. In this study, the mean horizontal angle of the right and left condylar left in the group A (DJD) and B (Non DJD) were studied. Group A included both condyles in each sample with DJD disorder and Group B included both condyles in non-affected sample. It was shown that there was no significant difference between the values of this variable between the left and right condyles in each group Despite the similarity in terms of the technique used (using CBCT images, the measured parameter, and also the patients studied), the design of this study was different from the present study that challenge the comparison of the results of the two studies. Lee et al. included patients who were totally involved from only one side of the condylar [20]. However, in the present study, all patients on both sides of the condyles were involved with DJD. The result of this study were found similar to previous study with the difference that in the present study, the comparison of the horizontal angle of the condylar of both sides of the patients (both sides of the disease) was performed on both sides of the nonaffected group. The present study is similar in terms of the fact that the involved and non-involved joints in the DJD were studied. In other words, the simultaneous examination of involved and non-involved condyles only in a patient with DJD (not in two different patients) and the removal of spontaneous variables that may influence the parameters of the desired parameter in Lee et al. study has caused the horizontal angle of the condylar to be reported on the larger side. In other studies, with MRI techniques, it was shown that the horizontal angle of the condylar in patients with disk insertion is significantly higher [20]. The cause of the larger horizontal angle of the condylar in these studies is attributed to two possible causes. The first reason is the relatively large stretch that is found in patients with disk replacement. The second reason is the remodeling of disc replacement in patients [15,28]. The lack of significance of mean horizontal angle of the condyles in the two groups in the present study compared to the studies mentioned above, can also be due to the difference in the horizontal angle test technique (MRI in the above studies and CBCT in the present study), racial diversity, the criteria for entering a different study (these studies are related to patients with disk replacement and the present study was patients with bilateral DJD involvement) as well as the number of subjects studied in the study.
Al-Rawi et al. also conducted a study in which CBCT images of 35 people with TMJ and 35 non-affected condylar spatial states were examined by several parameters, one of which was the measurement of horizontal angles Condyle. They showed that the angle of the condyle in the patient group was smaller than that of the control group [18]. However, in the present study, there was no difference between horizontal and horizontal angle changes between DJD and non-affected individuals. The present study was conducted on horizontal angle of view of the condylar, using CBCT and bilateral interaction of the present study, but the results of this study showed a significant difference between the two groups, which can be influenced by several factors: first, they are justifiable The smaller condylar angles in patients compared with those in the control group indicated that the condyles of patients were rotated inwards, and this also had an effect on reducing the angle of the condyle in the axillary plan [18]. Second, in the sample, the age range (73 years-18 years) was wider than the study (age 16 years-44 years).
Conclusions
The results of this research showed that the horizontal angle of the right and left condyles were not significantly different between the two groups A (DJD) and B (Non- DJD).
The horizontal angle of the left and right condyles in the group of women and in the men group was not significantly different, and also in the age group of 18 years-34 years and in the age group of 35 years to 74 years, there was a significant difference between the two groups A (DJD) and B (Non-DJD) There was no horizontal conical angle.
Recommendations
1. Examining the horizontal angle of the condylar in people who are unilaterally involved with the DJD and comparing this angle between the two involved and non-involved joints.
2. Conducting a similar study at the national level in order to obtain more accurate and curable results
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Mathew AL, Sholapurkar AA, Pai KM. Condylar changes and its association with age, TMD, and dentition status: A cross-sectional study. Int J Dent 2011; 2011.
- Kalladka M, Quek S, Heir G, et al. Temporomandibular joint osteoarthritis: Diagnosis and long-term conservative management: A topic review. Indian Prosthodont Soc 2014; 14:6-15.
- White SC, Pharoah MJ. Oral radiology-e-book: Principles and interpretation. Elsevier Health Sciences 2014.
- Ernberg M, Alstergren P. Clinical cases in orofacial pain. Oxford: Wiley Blackwell 2017.
- Gidarakou IK, Tallents RH, Kyrkanides S, et al. Comparison of skeletal and dental morphology in asymptomatic volunteers and symptomatic patients with bilateral degenerative joint disease. Angle Orthod 2003; 73:71-8.
- Salter DM. Degenerative joint disease. Curr Diagn Pathol 2002; 8:11-8.
- Braem K, Luyten FP, Lories RJ, et al. Degenerative joint disease. Ann Rheum Dis 2012; 71:722-8.
- Lin YC, Hsu ML, Yang JS, et al. Temporomandibular joint disorders in patients with rheumatoid arthritis. J Chin Med Assoc 2007; 70:527-34.
- Honey OB, Scarfe WC, Hilgers MJ, et al. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: Comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop 2007; 132:429-38.
- Koch BL, Hamilton BE, Hudgins PA, et al. Diagnostic imaging: Head and neck e-book. Elsevier Health Sciences 2016.
- Winocur E, Reiter S, Krichmer M, et al. Classifying degenerative joint disease by the RDC/TMD and by panoramic imaging: A retrospective analysis. J Oral Rehabil 2010; 37:171-7.
- Westesson PL, Bifano JA, Tallents RH, et al. Increased horizontal angle of the mandibular condyle in abnormal temporomandibular joints: A magnetic resonance imaging study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1991; 72:359-63.
- Nasseh IB, Noujeim ME. TMJ radiographic changes in asymptomatic patients examined with CBCT. 17th Congress of the International Association of DentoMaxilloFacial Radiology 2009.
- Imanimoghaddam M, Madani AS, Talebzadeh MR, et al. The relationship between osseous changes of the temporomandibular joint and RDC/TMD groups in CBCT images. JDMT 2014; 3:151-7.
- Sülün T, Akkayan B, Duc JM, et al. Axial condyle morphology and horizontal condylar angle in patients with internal derangement compared to asymptomatic volunteers. CRANIO® 2001; 19:237-45.
- Kaimal S. Diagnostic accuracy of panoramic radiograph and MRI for detecting signs of TMJ degenerative joint disease. Thesis, University of Minnesota Digital Conservancy 2016.
- Samra DA, Hadad R. Midpalatal suture: Evaluation of the morphological maturation stages via bone density. Prog Orthod 2018; 19:29.
- Al-Rawi NH, Uthman AT, Sodeify SM. Spatial analysis of mandibular condyles in patients with temporomandibular disorders and normal controls using cone beam computed tomography. Int J Oral Implantol 2017; 11:99.
- Koç A. Comparison of the horizontal condyle angle of the dentulous and edentulous patients using cone beam computed tomography. Eastern J Med 2018; 23:254.
- Lee PP, Stanton AR, Hollender LG. Greater mandibular horizontal condylar angle is associated with temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol 2017; 123:502-7.
- Haskin CL, Milam SB, Cameron IL. Pathogenesis of degenerative joint disease in the human temporomandibular joint. Crit Rev Oral Biol Med 1995; 6:248-77.
- Helenius LM, Hallikainen D, Helenius I, et al. Clinical and radiographic findings of the temporomandibular joint in patients with various rheumatic diseases. A case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 99:455-63.
- Bayar N, Kara SA, Keles I, et al. Temporomandibular joint involvement in rheumatoid arthritis: A radiological and clinical study. CRANIO® 2002; 20:105-10.
- Bracco P, Debernardi C, Piancino MG, et al. Evaluation of the stomatognathic system in patients with rheumatoid arthritis according to the research diagnostic criteria for temporomandibular disorders. CRANIO® 2010; 28:181-6.
- Arvidsson LZ, Smith HJ, Flatø B, et al. Temporomandibular joint findings in adults with long-standing juvenile idiopathic arthritis: CT and MR imaging assessment. Radiology 2010; 256:191-200.
- Lim YK, Kim MJ, Kim YJ, et al. Distribution and clinical features of patients with degenerative change of the mandibular condyle. Korean J Orthod 2006; 36:402-11.
- Wiberg B, Wänman A. Signs of osteoarthrosis of the temporomandibular joints in young patients: A clinical and radiographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 86:158-64.
- Kurita H, Ohtsuka A, Kobayashi H, et al. Relationship between increased horizontal condylar angle and resorption of the posterosuperior region of the lateral pole of the mandibular condyle in temporomandibular joint internal derangement. Dentomaxillofac Radiol 2003; 32:26-9.
Author Info
F Ezoddini Ardakani1, Yaser Safi2 and Mahjube Entezar-e-ghaem1*
1Faculty of Dentistry, Department of Oral and Maxillofacial Radiology, Shahid Sadoughi University of Medical Sciences, Yazd, Iran2Department of Oral and Maxillofacial Radiology, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Citation: F Ezoddini Ardakani, Yaser Safi, Mahjube Entezar-e-ghaem, The evaluation of the average of horizontal angle of the condylar in the axially plan in patients with degenerative joint disease of the temporomandibular joint (DJD of the TMJ), J Res Med Dent Sci, 2019, 7(2): 152-158.
Received: 05-Mar-2019 Accepted: 16-Apr-2019
