Research - (2019) Volume 7, Issue 5
The Effect of Sleep Deprivation on Heart Rate Variability in Shift Nurses
Muzeyyen Arslan1,2, Menizibeya O Welcome3* and Senol Dane3
*Correspondence: Menizibeya O Welcome, Department of Physiology, College of Health Sciences, Nile University of Nigeria, Nigeria, Email:
Abstract
Background: There is inconsistency in heart rate variability (HRV) reported among shift workers. We aim to investigate the effects of sleep deprivation on HRV in shift work nurses.
Methods: Fifty one healthy female nurses participated in this study. HRV was evaluated at 9 a.m. in two successive days before and after shift work at 24 hours following the initial HRV evaluation. The Power Lab 26T (ADInstruments, Australia) was used to record ECG was. Analysis of signals was performed using the MLS310/7 HRV Module of Lab Chart® software.
Results: Compared to baseline, shift work resulted in significant decrease in high frequency, total power, SDNN, and pNN50, with concomitant increase in low frequency/high frequency ratio.
Conclusions: Sleep deprivation can disrupt the autonomic control of heart rhythm and predispose to cardiovascular morbidity and mortality.
Keywords
Sleep deprivation, Shift work, Non-shift work, Cardiac rhythm, Heart rate variability
Introduction
Health care workers are involved in a 24-hour lifesaving activity, a critical function of clinics and hospitals worldwide [1]. Consequently, health personnel are required to work in a rotating fashion, day and night. Nurses are key players in this 24-hour work rotation. Thus disorder of bodily functions that affect these health workers due to pattern of work rotation, accordingly, will affect the quality of care especially when a considerable number of nurses are affected [1,2].
Statistical data indicate that approximately 20 percent of the global workforce is engaged in work rotation (shift work) [3]. Depending on the geographical region, however, the percentage of shift workers can reach 39% [4]. Over the past few decades, accumulating data have steadily shown increase in the percentage of the workforce engaged in shift work [1-4].
Evidences indicate that shift work, and in particular, night shift, constitutes one of the major factors that induces disruption of circadian rhythm [1,2,5]. Circadian rhythm disruption is responsible for sleep-wake disorders, impaired alertness, and fatigue, which increase human errors, consequently, causing drug administration errors with resultant decrease in the quality of patient care [1,2,5]. Furthermore, disorder circadian rhythm can predispose the health care personnel to work-related injuries [1,2], increase job-related stress [6], thereby reducing job satisfaction [1,2]. Compared with day workers, night workers develop cardiovascular disease problems and complications (e.g. hypertension, ischemic stroke), gastrointestinal disorders (gastritis, dyspepsia, indigestion, etc.), poor reproductive outcomes (e.g. miscarriage, preterm delivery) [1,2], insomnia [7], mental health problems (anxiety, depression, paranoid disorders etc.) [2], cancers [1,2,8], back pain, menstrual disorders [1], and thus, significantly decreased productivity [9].
Shift work disorder has been recently distinguished as a separate clinical syndrome that is characterized by impairment of the circadian rhythm, leading to insomnia, narcolepsy, fatigue, and disordered alertness [2]. The prevalence of shift work disorder is estimated to occur in 18-60% of the workforce [1]. Several research investigations using the 5th Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [2] have confirmed a high prevalence of shift work disorder among the workforce [1,7,10]. Indeed, based on DSM- 5 assessment, shift work disorder reportedly occurs in 5-44% of the workforce, depending on the work rotation [10].
Undoubtedly, there is a growing body of literature data on the health problems associated with shift work. Unfortunately, however, little is known about the changes associated with the cardiovascular system after the night shift. Though previous studies have shown that medical shift workers more frequently experience cardiovascular diseases and hypertension [1,2] compared to medical non-shift workers, specific changes in cardiovascular system that results from shift work, in particular night shift have not been fully explored. Relatively recently, Lin et al. [11] reported a substantial increase (by 2.7%) in cardiovascular mortality in night shift nurses compared to non-shift ones. Regrettably, however, the pathophysiological mechanisms associated with night shift disorders have not been fully unraveled. Importantly, knowledge about these mechanisms may be helpful in planning or scheduling of work rotation, and also, therapeutic strategies of shift work and related disorders. Moreover, knowledge garnered from results of studies on the mechanisms of shift work disorders can aid in effective planning of intervention programs that will be directed towards improvement of sleep quality. In addition, results of such investigations can also serve as essential driving force in development of guidelines on protection of shift workers from cardiovascular consequences.
Heart rate variability (HRV) is a key indicator of functions of the cardiovascular system. HRV is normally measured through time-depended measures obtained from an electrocardiogram. HRV is a phenomenon of variation in beat-to-beat time interval of the heart [12]. HRV can provide useful information about indicators of disease or warnings about imminent heart disease [12]. A couple of authors have indicated that autonomic nervous system (ANS) imbalance, assessed by HRV, is related to cardiovascular diseases. Notably, ANS affects the development of hypertension, coronary artery disease, heart failure, and sudden death. Emerging data indicate that HRV may be related to life expectancy and disorders that affect other organs and systems of the body [13]. Thus, HRV variables can be used for clinical evaluation for patient risk stratification of cardiovascular diseases.
HRV changes in nurses, working day and night shifts have not been reported. We, therefore, conducted this study to investigate the effects of night shift on HRV in nurses.
Methods
Ethical compliance
The present study was conducted in line with the 1964 Helsinki Declaration and its amendments. The concerned authorities gave permission to carry out the study before the nurses were approached.
Participants
The participants of this study were apparently healthy nurses who worked in Turgut Ozal University, Medical Faculty Hospital, Ankara, Turkey. The study was conducted from January 2016 to June 2016. Potential participants for the study were contacted through the hospital nursing register. The phone contacts of all nurses working in different departments of the hospital (wards of general surgery, orthopedics, neurosurgery, emergency department, general medicine, neurology unit, metabolic medicine, cardiovascular medicine, rehabilitation medicine, gastroenterology, and cardiology) on shift duties were retrieved and they were informed about the study one week before commencement. Only those involved in shift work were included in the study. In addition, fresher’s and low experienced workers were not included in the study so as to completely avoid interference with working time as this group of workers require a higher level of attention concentration on their duties. Before commencement of the study, all participants voluntarily gave written informed consent after the aims and objectives of the study had been explicitly explained to them. The confidentiality and anonymity of all participants were maintained. Altogether, fifty-one (n=51) nurses (age range 25–40 years, average age: 29.39 ± 5.32 years) voluntarilygave consent for participation in the study. Their past medical history was used to determine the absence or presence of chronic illnesses and other habits. All participants were non-smokers, without any overt cardiovascular, respiratory, metabolic or sleep disorders, and were not taking any medication at the time of this study.
Participants were requested to follow a standard diet without alcohol, coffee, tea or chocolate a day before the study and until the end of the entire experiment.
Heaviness of night shift of the participants
As a routine in the hospital, the nurses involved in this study had 2-3 night shifts and 2-3 day shift work per week in an alternating order. The night shifts are usually moderate as work is distributed among the nurses in each ward: documentation, care coordination, administration of drug, evaluation of patient and monitoring of vital signs of the patients on specified (regular) regular intervals, and where necessary, carry out feeding of patients, palliative care, among others. During night shift, nurses travelled about 1-2.5 (average of 2) miles.
Procedure
On the first day of the experiment, participants had no night shift and were asked to adhere to at least 7-8 hours of night sleep. At 9:00 a.m. of the following day after night sleep, ECG (HRV) recording was performed for each participant in a lying position. The HRV was recorded for duration of 15 minutes in a quiet room, after 15 minutes of acclimatization, which was meant to stabilize the parameters of ANS. The respiratory rate was counted in all participants as certain ECG indices may be affected by respiration. The participants were allowed to carry out their usual daytime and night routine. During the study, we ensured that there was not interference between data collection and the professional duties of the staff. Participants were allowed to sit on a chair when not operative but never to stay supine. A second ECG (HRV) recording was performed the second day at 9.00 a.m. after night shift.
Height and weight measurement
The participants’ height and weight were measured with the aid of a floor type RGZ-120 weighing machine, having a dimension of 900 × 350 × 305 mm and weight of 24 kg. During recording, participants were requested to keep their bags, shoes, and other load interfering objects. Height and weight measurements were carried out simultaneously according to the manufacturer specifications.
HRV
ECG recording was performed with PowerLab26T (AD Instruments, Australia) with the HRV Module of the Lab Chart® software (MLS310/7). Briefly, in accordance with the standard Einthoven triangle, three adhesive ECG electrodes were placed on the right wrist and right and left legs. The digital signals (ECG) were filtered by the software to exclude artifacts before HRV analysis (Figure 1).
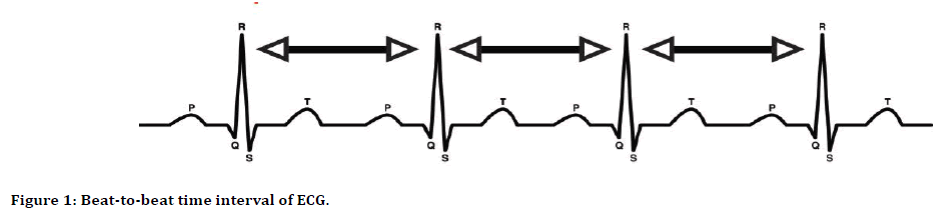
Figure 1: Beat-to-beat time interval of ECG.
Time and frequency domains of HRV parameters were analyzed using (1) VLF: Very Low Frequency spectral power (0.003–0.04 Hz), (2) LF–Low Frequency Spectral power (0.04– 0.15 Hz), (3) HF: High Frequency Spectral Power (0.15–0.4), (4) LF/HF: Ratio between Low and High Frequency Components, (5) Total power sum of VLF, LF, and HF, (6) Normal-to-normal R-R intervals (NN), (7) Standard deviation of all NN intervals (SDNN) or R-R of normal sinus beats, (8) Standard deviation of average NN intervals (SDANN), (9) Square root of the mean squared differences of successive NN intervals (RMSSD), (10) Ratio of the number of NN50 intervals and the number of all NN intervals (pNN50), where NN50 is the number of pairs of adjacent NN intervals differing by more than 50 ms [14,15]. The frequency domains HRV parameters are VLF, LF, HF, LF/ HF, and total power. The time domains HRV parameters are SDNN, SDANN, RMSSD, NN50, and pNN50 [14,15].
LF is a marker for sympathetic effects, but reflects both sympathetic and parasympathetic activity on HRV [14,15]. LF reflects resting baroreceptor activity [15], but part of LF variability may be due to unspecified factors [14]. HF isused to indicate the level of activity of the parasympathetic nervous system. The HF is also called the respiratory band [14] because it corresponds to the HRV related to the respiratory cycle. The LF/HF ratio is an estimate of balance of sympathetic to parasympathetic nervous system activity i.e. sympatho-vagal balance [16]. A high LF/HF ratio indicates dominance of the sympathetic division of ANS, while a low LF/HF ratio indicates parasympathetic dominance [14,15]. VLF is a possible marker of sympathetic activity; however, its physiological origin is not fully understood [14,15]. VLF may be due to the activities of the cardiac intrinsic nervous system or sympathetic effects on the heart’s activities [16]. Research suggests that VLF may be related to influences of humoral factors of the renin-angiotensin system, thermoregulation [17] or metabolism on HRV [18]. VLF can be used to evaluate depression [19], and may be associated with dysregulation of circadian rhythms and energy metabolism in fatigue. Low VLF power is associated with fatalities due to arrhythmia [16]. Total power reflects global HRV [20].
The SDNN index is formed from both sympathetic and parasympathetic activities. It is the “gold standard” for stratification of cardiac risk especially if the recording is made for a period of 24 hours [14,15,17,20]. SDNN value below 50 msis unhealthy, 50–100 ms indicates compromised health, and above 100 ms is healthy [17,20]. SDNN well correlates with LF, VLF and total power [20]. The original and importance of the SADNN index is not clear. RMSSD reflects parasympathetic activity on the heart [14,15]. It is the major time-domain measure that provides a quantitative estimate of the parasympathetic influences on the heart [16]. pNN50 is associated with activity of the parasympathetic nervous system. It is correlated with the RMSSD and HF band power [17,20].Data analysis.
The data obtained were stored in Microsoft Excel 2010 and analyzed using Statistical Package for the Social Sciences (SPSS) version 18 (SPSS Inc., Chicago, IL, USA). The data had a normal distribution and the Student t-test was used to determine differences between HRV variables recorded before and after shift work. The value for statistical significant was set at p˂0.05.
Results
Table 1 shows the age, height, weight and duration of work experience of the nurses that participated in the study.
| Parameters | Mean ± SD |
|---|---|
| Age | 29.39 ± 5.32 years |
| Height | 1.62 ± 0.07 meter |
| Weight | 64.12 ± 13.69 kg |
| Duration of average work experience | 3.56 ± 1.34 years |
Table 1: Means and standard deviations of the age, height, weight and duration of the participants.
The respiration rate of the nurses was 17.22 ± 3.87 before shift work and 18.04 ± 7.91 after shift work (t=0.52). The SDNN (ms), pNN50 (%), variability of NN intervals (≤ 0.4 Hz) (total power) (ms2) and HF were significantly decreased after shift work (sleep deprivation) compared to their corresponding values before shift work (SDNN: t=2.52, p=0.02; pNN50: t=3.11, p=0.003; total power: t=2.43, p=0.03; HF: t=2.89, p=0.01, respectively) (Table 2). LF/HF ratio was statistically increased after shift work (t=2.16, p=0.04). All other HRV parameters– SDANN, RMSSD, maximal NN intervals, minimal NN intervals, mean NN, pulse rate (1/minute), VLF band power (ms2) and LF band power (ms2) after shift work were not statistically different, compared to the values obtained before shift work (Table 2).
| Parameters | Before shift work | After shift work | t | p |
|---|---|---|---|---|
| Maximum NN (ms) | 1101.86 ± 254.82 | 1309.24 ± 361.81 | 3.41 | 0.001 |
| Minimum NN (ms) | 640.12 ± 48.77 | 621.53 ± 121.71 | 1.01 | NS |
| Mean NN (ms) | 836.72 ± 78.36 | 841.09 ± 224.13 | 0.12 | NS |
| Pulse Rate (1/minute) | 71.97 ± 6.18 | 72.99 ± 9.85 | 0.56 | NS |
| SDNN (ms) | 72.35 ± 15.76 | 62.18 ± 11.56 | 2.52 | 0.02 |
| SDANN (ms) | 73.26 ± 44.71 | 64.14 ± 40.07 | 0.96 | NS |
| RMSSD (ms) | 73.19 ± 44.61 | 63.21 ± 3782 | 1.09 | NS |
| pNN50 (%) | 39.32 ± 24.41 | 23.43 ± 20.91 | 3.11 | 0.003 |
| Total Power (ms2) | 6017.62 ± 5030.21 | 3728.51 ± 3496.66 | 2.43 | 0.03 |
| VLF (ms2) | 1082.06 ± 159.79 | 1046.22 ± 267.25 | 0.78 | NS |
| LF (ms2) | 1439.89 ± 965.6 | 1040.66 ± 1365.08 | 1.57 | NS |
| HF (ms2) | 2485.82 ± 3103.02 | 985.07 ± 1289.08 | 2.89 | 0.01 |
| LF/HF | 1.76 ± 0.58 | 2.18 ± 0.92 | 2.16 | 0.04 |
| N/B: VLF: Very Low-Frequency Spectral Power (0.003–0.04 Hz); LF: Low-Frequency Spectral Power (0.04–0.15 Hz); HF: High-Frequency Spectral Power (0.15–0.4); LF/HF: Ratio Between Low and High Frequency Components; Total Power-Sum of VLF, LF, and HF;NN: Normal-to-Normal R-R intervals; SDNN: Standard Deviation of the NN intervals; SDANN: Standard Deviation of the averages of NN intervals in all 5 minute segments of the entire recording; RMSSD: Square root of the mean squared differences of successive NN intervals; pNN50: The percentage of difference between adjacent NN intervals that are greater than 50 ms. | ||||
Table 2: HRV parameters before and after shift work in nurses (n=51).
Discussion
Sleep is a physiological state required for maintenance of normal health and homeostasis. The vast majority of human beings spend about 30% of their lives asleep, accentuating the usefulness of sleep to human existence. Indeed, disruption of sleep-wake cycle pattern leads to considerable health consequences [21]. The data obtained from this study revealed that sleep deprivation is associated with sympatho-vagal imbalance and predominance of sympathetic over parasympathetic activity. This suggests that disruption of normal sleep-wake cycle is associated with dysregulation of cardiac rhythm.
The results of this present study are consistent with results of other studies. Wehrens et al. [22] reported high LF/HF ratio, and decrease in other parameters of HRV among shift workers compared with non-shift workers. Cebeci et al. [23] also reported decrease in indicators of HRV, excluding LF/HF ratio, after shift work in medical doctors. Tobaldini et al. [24] reported a predominantly sympathetic influence and decreased parasympathetic activity after a single night sleep deprivation, suggesting that the sympatho-vagal balance shifted towards a sympathetic predominance with acute sleep deprivation [25]. Despite the changes associated with LV/HV in our study, respiratory rate before sleep deprivation was not significantly different from the rate after sleep deprivation. A couple of researchers have shown that heart rate and respiratory rate are the most powerful factors that affect HRV indices. However, the contribution to changes in HRV by heart rate is far greater than respiratory rate [26]. Importantly different respiration rates have varying influence on HRV [27]. At lower respiratory rate (3-6 beats/ minute) the effect of respiration on HRV seems to be significant. However, respiratory influence on HRV becomes least significant at a respiratory rate of 14 breaths per minute [28]. Pitzalis et al. also reported frequency-dependent influence of respiration on HRV and observed minimal effects of higher respiratory rate on HRV [29]. On the average, respiratory rate in our study was 17-18 beats/minute. Within the range of this respiratory value, Schipke et al. did not notice any significant influence of respiration on time domain HRV indicators [27]. Similar results have been reported elsewhere [30,31]. But it appears that the effect of respiration, heart rate and other physiologic factors on HRV depends on health state of the individual [30,31]. Further research is required to elucidate the multiple factors and their mechanisms of influence on HRV. On the basis of LF/HF ratio, it can be suggested that shift work or sleep deprivation may cause an increase in cardiovascular morbidity and mortality by disrupting biological rhythm, which is responsible for the sympatho vagal imbalances. Indeed decreased heart rate variability, but increased LF/HF ratio (i.e. increased sympathetic and decreased parasympathetic tone on heart activity) has been associated with cardiovascular disease [32]. Indeed previous data reported by Harris et al. [33] and Lanza et al. [34] have shown that LF/HF ratio is a strong prognostic indicator of cardiac diseases and mortality.
However, some authors have argued that LF/HF ratio is not a good indicator of sympathovagal imbalances [35]. Therefore, it is important for future studies to address these inconsistencies in the literature.
The sympathetic and parasympathetic divisions of the ANS innervating the heart interact amongst themselves to regulate cardiac functions. The physiological state due to the sympathetic and parasympathetic activity can be described as “sympatho-vagal balance”. HRV parameters are indicators of sympatho-vagal balance or imbalance. Though the mechanisms of the interaction between these divisions of the ANS have not been completely unraveled, available scientific information indicate that sleep deprivation or shift work causes a multi-system impairment, likely resulting from disruption of circadian rhythm [7,25,32]. This is consequent to the hypothesis that circadian rhythm is an integral coordinator of homeostasis of almost all organs and systems of the body [7,21].
Evidently, sleep deprivation causes disorder of synchronization of the supra chiasmatic nucleus and endocrine functions, which in turn leads to disorder of secretion of hormones such as serotonin, melatonin, noradrenaline, acetylcholine, corticosteroids, etc. These disorders in hormone secretion can ensue in disruption of cardiac rhythms, and other physiological processes [7,21,25,32,36]. Both acute and chronic sleep deprivation can alter inflammatory response by causing substantial decrease in anti-inflammatory cytokine production [36,37], disrupting the activities of natural killer cells [37] and neutrophil degranulation [38]. A study conducted in laboratory animals showed that sleep deprivation also increases oxidative stress and lipid peroxidation, which may underlie some of the negative health consequences of shift work or sleep deprivation [39]. Though we did not assess the changes associated with energy expenditure or metabolic indices in our study, previous works have reported substantial increase in energy expenditure during sleep deprivation [40]. However, contradictory data have been reported by Al Khatib et al. who identified increased energy intake with no effect on energy expenditure following sleep deprivation [41].
Calvin et al. reported similar findings [42]. The molecular pathways of energy metabolism associated with sleep deprivation are yet to be delineated, arguably, emerging results indicate that leptin and ghrelin concentrations [42–44]. For instance, Calvin et al. [42] did not find any change in leptin and ghrelin concentrations following sleep deprivation in adults, whereas Li et al. [45] reported a substantial change in lept in and adiponectin level following sleep deprivation in children and adolescents. It can be suggested, therefore, that the effect of sleep deprivation on cardio metabolic profile may be dependent, at least in part, on the age of the individual. Furthermore, the number of years of shift work can substantially affect these indices. Available data suggest that reference or benchmark duration of shiftwork associated with cardio metabolic derangement is 6 years [46]. However, Tanaka et al. reported a 17 year period as the reference duration for shift work to cause cardio metabolic disorder [47]. The participants in our study had only three and half years of accumulated duration of shift work. Whether reference duration of shiftwork associated with cardio metabolic derangement is 6 years or more, it can be undisputedly true that risk of disorders in energy metabolism due to sleep deprivation increases with increase in accumulated years of shift work [46–48]. Thus it is essential to pay special attention and continuously monitor the consequences of work rotation or sleep deprivation on cardio metabolic and HRV parameters..
While work diversification or time scheduling importantly contributes to betterment of work organization, and consequently, human life, there are potentially adverse health problems associated with such work organization. Hence, it is imperative to formulate measures and interventions aimed at mitigating the negative outcome of shift work on the health of the individual, and also, provide solutions for improved scheduling of working time with considerably reduced negative impact on the health of the individual.
Conclusion
Parameters of HRV (SDNN, pNN50, total power and HF) decreased, while ratio of low frequency/ high frequency (LF/HF) increased after shift work. The other HRV parameters (SDANN, RMSSD, maximal NN intervals, minimal NN intervals, mean NN, VLF and LF band power) obtained after shift work were not statistically different from to the values obtained before shift work. Thus, sleep deprivation can disrupt the autonomic control of heart rhythm (sympathovagal balance) and predispose to cardiovascular morbidity and mortality.
Conflict of Interest
None declared.
References
- Anbazhagan S, Ramesh N, Nisha C, et al. Shift work disorder and related health problems among nurses working in a tertiary care hospital, Bangalore, South India. Indian J Occup Environ Med 2016; 20:35–38.
- Ferri P, Guadi M, Marcheselli L, et al. The impact of shift work on the psychological and physical health of nurses in a general hospital: A comparison between rotating night shifts and day shifts. Risk Manag Healthc Policy 2016; 9:203–211.
- Parent-Thirion A, Biletta I, Cabrita J, et al. Sixth european working conditions survey – overview report. Luxembourg: Publications Office of the European Union 2016.
- Bae MJ, Song YM, Shin JY, et al. The association between shift work and health behavior: findings from the Korean national health and nutrition examination survey. Korean J Fam Med 2017; 38:86–92.
- Muecke S. Effects of rotating night shifts: literature review. J Adv Nurs 2005; 50:433–439.
- McVicar A. Scoping the common antecedents of job stress and job satisfaction for nurses (2000–2013) using the job demands-resources model of stress. J NursManag 2016; 24:112–136.
- Drake CL, Roehrs T, Richardson G, et al. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep 2004; 27:1453–1462.
- Nojkov B, Rubenstein JH, Chey WD, et al. The impact of rotating shift work on the prevalence of irritable bowel syndrome in nurses. Am J Gastroenterol 2010; 105:842–847.
- Roth T. Shift work disorder: Overview and diagnosis. J Clin Psychiatry 2012; 73:9.
- Flo E, Pallesen S, Magerøy N, et al. Shift work disorder in nurses–Assessment, prevalence and related health problems. PLoS One 2012; 7:33981.
- Lin X, Chen W, Wei F, et al. Night-shift work increases morbidity of breast cancer and all-cause mortality: A meta-analysis of 16 prospective cohort studies. Sleep Med 2015; 16:1381–1387.
- Chu-Duc H, Nguyen-Phan K, Nguyen-Viet D. A review of heart rate variability and its applications. APCBEE Procedia 2013; 7:80-85.
- Ernst G. Heart-rate variability: More than heart beats? Front Public Health 2014; 5:240.
- Dantas EM, Sant'Anna ML, Andreão RV, et al. Spectral analysis of heart rate variability with the autoregressive method: What model order to choose? Comput Biol Med 2012; 42:164-170.
- Malik M, Bigger JT, Camm AJ, et al. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task force of the European society of cardiology and the North American society of pacing and electrophysiology. Circulation 1996; 93:1043-1065.
- Shaffer F, Mc Craty R, Zerr CL. A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability. Front Psychol 2014; 5:1040.
- Bernardi L, Valle F, Coco M, et al. Physical activity influences heart rate variability and very-low-frequency components in holter electrocardiograms. Cardiovasc Res 1996; 32:234–237.
- Friedman BH. An autonomic flexibility-neurovisceral integration model of anxiety and cardiac vagal tone. Biol Psychol 2007;74:185–199.
- Davydov DM, Shapiro D, Cook IA, et al. Baroreflex mechanisms in major depression. Prog Neuropsychopharmacol Biol Psychiatry 2007; 31:164–177.
- Shaffer F, Ginsberg JP. An overview of heart rate variability metrics and norms. Front Public Health 2017; 5:258.
- Moszczynski A, Murray B. Neurobiological aspects of sleep physiology. Sleep 2012; 30:963–85.
- Wehrens SMT, Hampton AM, Skene DJ. Heart rate variability and endothelial function after sleep deprivation and recovery sleep among male shift and non-shift workers. Scand J Work Environ Health 2012; 38:171-181.
- Cebeci S, Canbal M, Yuksel R, et al. The effect of sleep deprivation on heart rate variability in shift and non-shift physicians. Clin Invest Med 2015; 38:233-236.
- Tobaldini E, Cogliati C, Fiorelli EM, et al. One night on-call: sleep deprivation affects cardiac autonomic control and inflammation in physicians. Eur J Int Med 2013; 24:664-670.
- Tobaldini E, Nobili L, Strada S, et al. Heart rate variability in normal and pathological sleep. Front Physiol 2013; 16:294.
- Gąsior JS, Sacha J, Jeleń PJ, et al. Heart rate and respiratory rate influence on heart rate variability repeatability: effects of the correction for the prevailing heart rate. Front Physiol 2016; 7:356.
- Schipke JD, Pelzer M, Arnold G. Effect of respiration rate on short-term heart rate variability. J Clin BasicCardiol 1999; 2:92-95.
- Song HS, Lehrer PM. The effects of specific respiratory rates on heart rate and heart rate variability. Appl Psychophysiol Biofeedback 2003; 28:13–23.
- Pitzalis MV, Mastropasqua F, Massari F, et al. Effect of respiratory rate on the relationships between RR interval and systolic blood pressure fluctuations: A frequency-dependent phenomenon. Cardiovasc Res 1998; 38:332–339.
- Quintana DS, Elstad M, Kaufmann T, et al. Resting-state high-frequency heart rate variability is related to respiratory frequency in individuals with severe mental illness but not healthy controls. Sci Rep 2016; 6:37212.
- Jurak P, Halamek J, Vondra V, et al. Respiratory induced heart rate variability during slow mechanical ventilation. Wien Klin Wochenschrl 2017; 29:251–258.
- Buccelatti E, Gilardi E, Scaini E, et al. Heart rate variability and myocardial infarction: systematic literature review and meta-analysis. Eur Rev Med Pharmacol Sci 2009; 13:299-307.
- Harris PRE, Stein PK, Fung GL, et al. Heart rate variability measured early in patients with evolving acute coronary syndrome and 1-year outcomes of rehospitalization and mortality. Vasc Health Risk Manag 2014; 10:451–464.
- Lanza GA, Cianflone D, Rebuzzi AG, et al. Prognostic value of ventricular arrhythmias and heart rate variability in patients with unstable angina. Heart 2006; 92:1055-1063.
- Billman GE, Huikuri HV, Sacha J, et al. An introduction to heart rate variability: Methodological considerations and clinical applications. Front Physiol 2015; 6:55.
- Redwine L, Hauger RL, Gillin JC, et al. Effects of sleep and sleep deprivation on interleukin-6, growth hormone, cortisol, and melatonin levels in humans. J Clin Endocrinol Metab 2000; 85:3597-3603.
- Irwin M, Thompson J, Miller C, et al. Effects of sleep and sleep deprivation on catecholamine and interleukin-2 levels in humans: clinical implications. J Clin Endocrinol Metab 1999; 84:1979-1985.
- Costa RJ, Smith AH, Oliver SJ, et al. The effects of two nights of sleep deprivation with or without energy restriction on immune indices at rest and in response to cold exposure. Eur J Appl Physiol 2010; 109:417-428.
- Gumustekin K, Seven B, Karabulut N, et al. Effects of sleep deprivation, nicotine, and selenium on wound healing in rats. Int J Neurosci 2004; 114:1433-1442.
- Hendrich A, Chow MP, Skierczynski A, et al. A 36-hospital time and motion study: how do medical-surgical nurses spend their time? Perm J 2008; 12:25–34.
- Al Khatib HK, Harding SV, Darzi J, et al. The effects of partial sleep deprivation on energy balance: a systematic review and meta-analysis. Eur J ClinNutr 2017; 71:614–624.
- Calvin AD, Carter RE, Adachi T, et al. Effects of experimental sleep restriction on caloric intake and activity energy expenditure. Chest 2013; 144:79-86.
- St-Onge MP. The role of sleep duration in the regulation of energy balance: effects on energy intakes and expenditure. J Clin Sleep Med 2013; 9:73–80.
- Morikawa Y, Nakagawa H, Miura K, et al. Effect of shift work on body mass index and metabolic parameters. Scand J Work Environ Health 2007; 33:45-50.
- Li L, Fu J, Yu XT, et al. Sleep duration and cardiometabolic risk among chinese school-aged children: do adipokines play a mediating role? Sleep 20017; 40:42.
- De Bacquer D, Van Risseghem M, Clays E, et al. Rotating shift work and the metabolic syndrome: A prospective study. Int J Epidemiol 2009; 38:848–854.
- Tanaka K, Sakata K, Oishi M, et al. Estimation of the benchmark duration of shiftwork associated with weight gain in male Japanese workers. Chronobiol Int 2010; 27:1895-910.
- Suwazono Y, Uetani M, Oishi M, et al. Estimation of the benchmark duration of alternating shift work associated with increased total cholesterol levels among male Japanese workers. Scand J Work Environ Health 2010; 36:142-149.
Author Info
Muzeyyen Arslan1,2, Menizibeya O Welcome3* and Senol Dane3
1Department of Public Health, Erasmus University Medical Center, Netherlands2Research Center Innovation in Care, Rotterdam University of Applied Sciences, Netherlands
3Department of Physiology, College of Health Sciences, Nile University of Nigeria, Nigeria
Citation: MuzeyyenArslan, Menizibeya O Welcome, Senol Dane, The Effect of Sleep Deprivation on Heart Rate Variability in Shift Nurses, J Res Med Dent Sci, 2019, 7(5):45-52.
Received: 06-Sep-2019 Accepted: 23-Sep-2019
