Review Article - (2021) Volume 9, Issue 12
Temporary Anchorage Devices: An Insight
Aravindaksha Rao, Deepak C, Kritika A and Deenadayalan P*
*Correspondence: Deenadayalan P, Department of orthodontics, SRM Kattankulathur Dental College and Hospital, Chennai, India, Email:
Abstract
The aim of this review was to categorize and document the various improvements and research conducted on the temporary anchorage device in the orthodontic practice. The various aspects discussed in the article include the structure and design of the miniscrew, the sites of insertion, the indications and contraindications, and the newer methods of utilising mini screws for anchorage purposes in orthodontic practice. The use of TADs as a mainstay in the field of orthodontics is quickly gaining traction. The field is diverse and requires a thorough understanding to allow practitioners to utilize the equipment to its fullest capacity.
https://maviyolculuk.online/
https://mavitur.online/
https://marmaristeknekirala.com.tr
https://tekneturumarmaris.com.tr
https://bodrumteknekirala.com.tr
https://gocekteknekirala.com.tr
https://fethiyeteknekirala.com.tr
Keywords
TAD’s, Miniscrew, Anchorage, ImplantIntroduction
Osteoarthritic Anchorage control is deemed as one of the most important factors in the success of orthodontic treatment. Anchorage, is defined as the resistance to unwanted tooth movement, and is the prerequisite for orthodontic treatment of skeletal and dental malocclusions. The role of anchorage control in orthodontic treatment has been appreciated since the 18th century. Realizing the limitations of moving teeth against other teeth used for anchorage, Angle introduced ideas such as the use of occlusal, occipital and stationary anchorage.
Intraoral and extraoral anchorage devices have been devised to provide suitable results. The extraoral appliances cannot be used for 24 hours a day as they tax the patient. On the other hand, strict dependence on the intra oral areas, usually dental units do not offer any significant advantage, except the fact that patient cooperation is less critical, therefore, it is important to have absolute anchorage that prevents reactive forces which might incur undesirable tooth movements.
A device that is temporarily fixed to bone for the purpose of enhancing orthodontic anchorage either by supporting the teeth of the reactive unit or by eliminating the need for the reactive unit altogether, and that which is subsequently removed after use, is called a temporary anchorage device (TAD). Most commonly used TADs in orthodontics are the mini implants.
Implant
Implantation is defined as the transfer of nonliving material into a biologic system. Implants are classified as endosteal, subperiosteal, or transosseous, depending on the area of implantation (Fig.1).
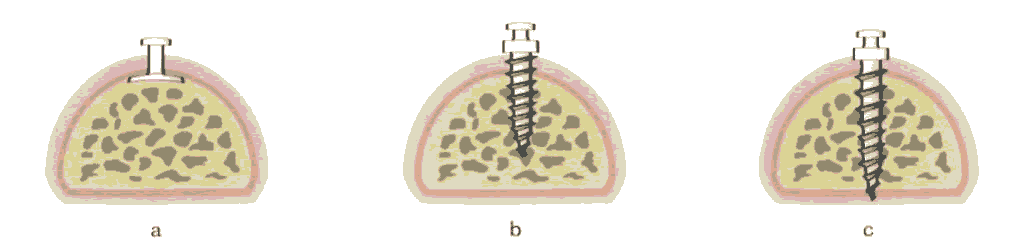
Figure 1: (a) The subperiosteal implant is placed under the periosteum and rests on the bone surface without penetrating it; (b) The endosteal implant is partially submerged and anchored within the bone; and (c) The transosseous implant penetrates the bone completely. Endosteal implants are most commonly utilised in the field of orthodontics.
Biocompatibility: The first ever successful clinical TAD was placed in 1983, when Vitallium screws were used to treat a patient with an overbite, by Creekmore and Eklund, Today, TADs are being used for restorative procedures, as well as in many camouflage procedures that previously required orthognathic surgery. A study conducted by Jeffrey Birg and Michelle Wheater in 2015, was performed in a cell culture of human gingival fibroblasts cells, to evaluate the biocompatibility of five commercially available orthodontic miniscrews / temporary anchorage devices. They demonstrated long-term biocompatibility of miniscrews/ temporary anchorage devices with gingival fibroblasts and non-cytotoxic composition of the devices to oral cells.
Osseointegration: Complete osseointegration of screws used in orthodontic applications complicates the removal process and is considered a disadvantage. Most of these devices minimize the development of bone promoting soft tissue attachment as they are manufactured with a smooth surface, under ordinary conditions. A study has been done by Chaddad in 2008, who tried to modify miniscrew- implant surface and evaluated the clinical performance and the survival rate of machined titanium (MT) versus sandblasted, large grit, acid-etched (SLA) mini- implants under immediate orthodontic loading. Although the correlation between the implant surface characteristics and the rate of success was not statistically significant, the survival rate of the SLA miniimplants in this investigation was higher compared with the MT group (93.5% to 82.5%).The conclusion reached was that survival rates of immediately loaded miniimplant were not influenced by surface characteristics. Torque value more than 15 Ncm recorded at the time of insertion appears to be one of the critical variables for mini-implant survival under immediate loading.
Primary Stability of Miniscrew Implants
Some factors influencing stability are:
• Device features: length, diameter, thread shape, thread pitch, thread design, thread type, cutting flute, construction material
• Operator/surgical technique-related factors
• Patient characteristics: cortical bone thickness.
Design and Structural Characteristics
Length
The threaded portion of the mini implant is referred to as the length, which can vary from 4 to 15 mm. An increase in maximum insertion torque, removal torque and pullout resistance can be achieved by an increase in mini implant length. Mini implant lengths of 5 mm and more do not affect primary stability, because these greater lengths of mini implants will be entering medullary bone.
The thickness of soft tissue at site of insertion must also be taken into account, along with a bone support of 5-6mm, during the selection of mini implant length. The ideal length of a mini implant is 9 mm, as this is thought to cause less stress on the surrounding bone than shorter mini implants and has less risk of damage to neighbouring anatomical structures than longer mini implants. From a clinical standpoint, a mini implant of 4-6 mm can be inserted into the majority of intraoral sites.
Diameter
The diameter of the mini implant is directly proportional to the primary stability of the implant. The larger surface area allows for the force to be distributed, thereby reducing the pressure on the bone at insertion site.
Biomechanical yield, implantation success and fracture resistance are most influenced by diameter rather than length of implant. Stable results have been observed in implants of diameter 1.5-2.3 mm in maxilla and mandible & a significant loss of anchorage has been observed when mini implants with diameters of less than 1.2 mm were used. The ideal diameter is probably between 1.3 and 1.5 mm.
there is a risk of unwanted root contact when mini implants of diameters greater than 2 mm are used, as the mean inter- radicular space is generally between 2.5 mm and 3.5 mm.17The mini implants with a 1.3 mm diameter have shown a success rate of 88.6%, which is not particularly high but needs to be weighed against the lesser risk of iatrogenic damage.
Implant Placement
The success of Implant is dependent on the identification of site for placement of orthodontic miniscrew implants (MIs)for various reasons, including primary stability, the biomechanics to apply, the protection of neighboring anatomical structures, and patient comfort.
Several anatomical sites for the insertion of miniscrew implants have been proposed
Implant Site:
Implant sites are selected according to the treatment plan, the biomechanics, and the quality and quantity of the bone. The following locations are only few of the many available implant sires in the oral cavity (Table 1).
Table1: implant sites of maxilla and mandible.
| Maxilla | Mandible |
|---|---|
| Paramedian or mid-sagittal region of the hard palate(Fig.2a) | Retromolar area |
| Zygomatic buttress of the maxilla (Fig.2b) | Buccal cortical (shelf) area (Fig.5a) |
| Area below the anterior nasal spine (Fig.3a) | Symphysis or parasymphysis area (Fig.5b) |
| Maxillary tuberosity | Edentulous alveolar ridges (Fig.6a) |
| Edentulous alveolar ridges (Fig.3b) | Interradicular spaces, both buccal and lingual (Fig.6b) |
| Interradicular spaces, both buccal and lingual (Fig.4a &4b) |
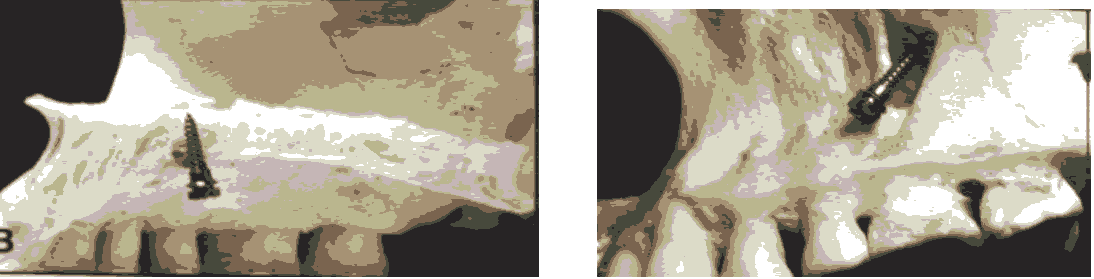
Figure 2: (a) Mid-Sagittal Region; (b) Zygomatic buttress.
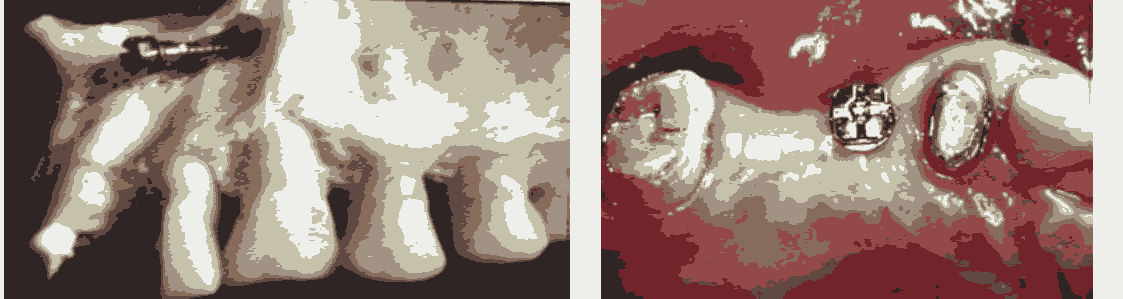
Figure 3: (a) Area below the ANS; (b) Edentulous ridges.
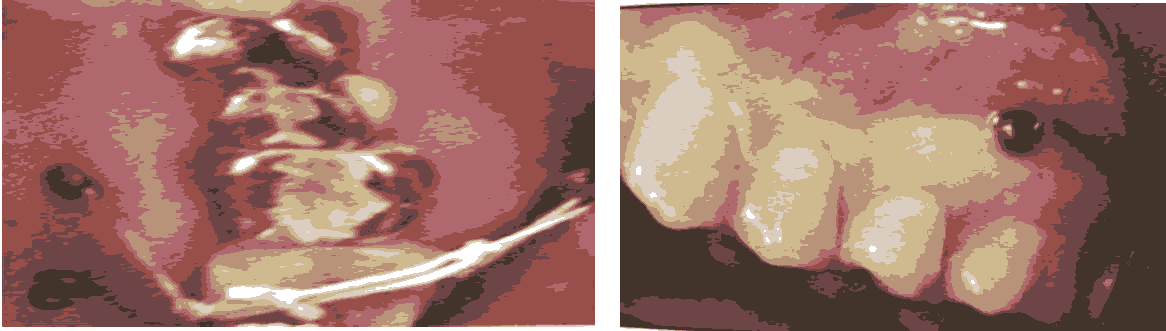
Figure 4: (a) Interradicular spaces (Buccal); (b) Interradicular spaces (palatal).
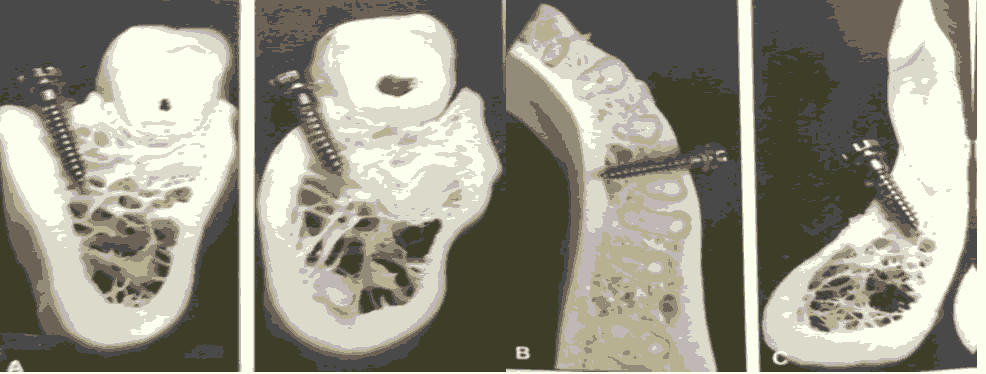
Figure 5: (a) Buccal Shelf Area Interradicular; (b) Symphysis Area.

Figure 6: (a) Edentulous Area; (b) Interradicular Space.
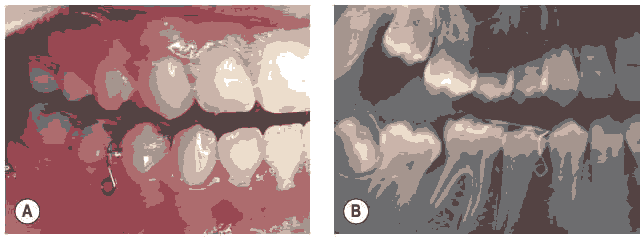
Figure 7: (a) Intraoral photograph after insertion of the device; (b) Diagnostic panoramic radiograph.
The X-Ray Pin:
A radiographic auxillary which has probing functions, it allows the marking of gingiva at the desired level for miniimplant insertion, this eliminates the need for laboratory procedures and wires. The X-ray pin is a very small auxiliary, fabricated from a SS alloy. It has a tapered conical shaft and a thickened ball-shaped head, ending in a point, for puncturing the gingiva (Fig.8,9).
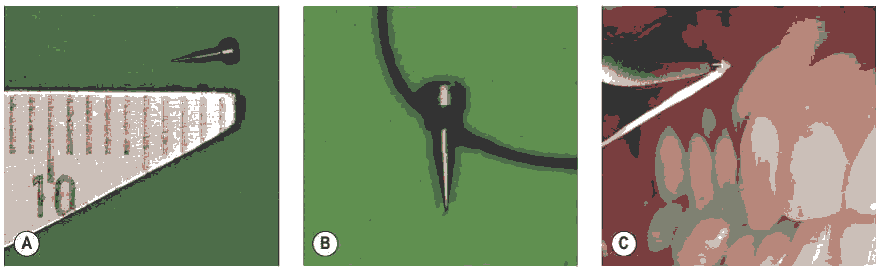
Figure 8: (a) The pin includes apuncture point, a conical shaft and a ball head (total length 3.5 mm; working length 2.5 mm, largest diameter 0.75 mm); (b) Securing of pin with dental floss; (c) Intraoral application of the pin at the predetermined point with Weingart plier.
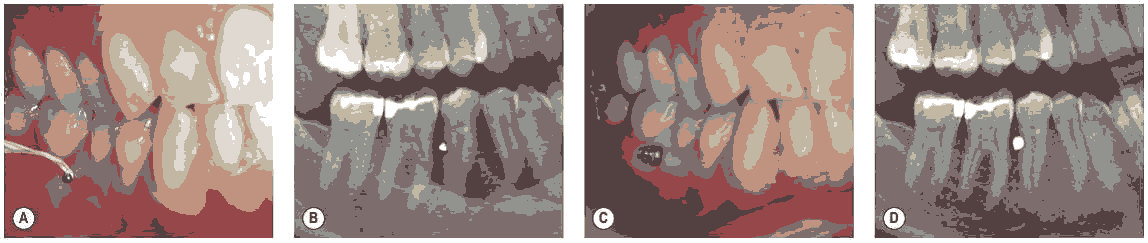
Figure 9: The use of X-ray pins for inter-radicular insertion of microscrew implants in the mandible. (a) Intraoral photograph showing the positioning of the pin; (b) Diagnostic panoramic radiograph showing the pin position and the bone availability of the insertion area; (c) Inserted MI; (d) Panoramic radiograph following mini implant insertion.
Precise Miniscrew Implant Insertion Technique:
Kim’s Stent is a device that comprises of positioning gauge and a direction guide.
Positioning Gauge
The positioning gauge is made up of a horizontal and a vertical arm, ligated to the first molar bracket,which helps to set the mesiodistal position of mini implant. The vertical arm helps with vertical portion of the positioning gauge, while the horizontal arm has five to eight pieces of wire acting as a gauge and welded at 1 mm intervals.
Direction Guide
The direction guide is ligated on to the second premolar bracket andindicates the direction of the mini implant insertion. The occlusal arm is the wire lying on the occlusal surface and is placed at the midpoint between the first molar & second premolar. It passes the contact point of the two adjacent teeth and approximates the proximal surface. The mini implant is inserted parallel to this occlusal arm. The horizontal angulation of the X-ray beam lies parallel to this occlusal arm. (Fig.10).
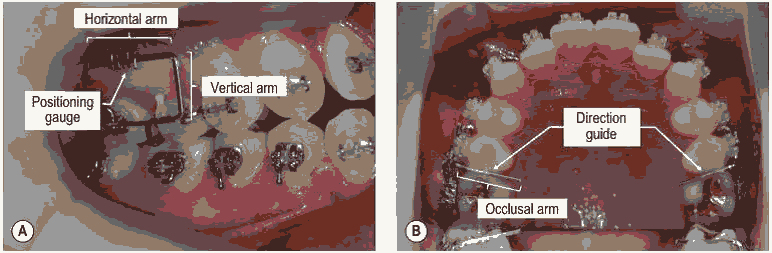
Figure 10: (a) The positioning gauge, which is ligated into the first molar bracket; (b) The direction guide, which is ligated into the second premolar bracket.
Grid Method:
Reddy KB, Kumar MP, Kumar MN (2008) developed a metal grid that can improve the accuracy of miniscrew placement in both the anterior or posterior segments of either arch. The grid is easily attached to the archwire to determine the ideal miniscrew position and is then disengaged after drilling, without the need for archwire removal and with no deformation of either the archwire or the grid. Its simple design permits easy fabrication, and the same device can be used for different patients if it is sterilized between uses (Fig.11).
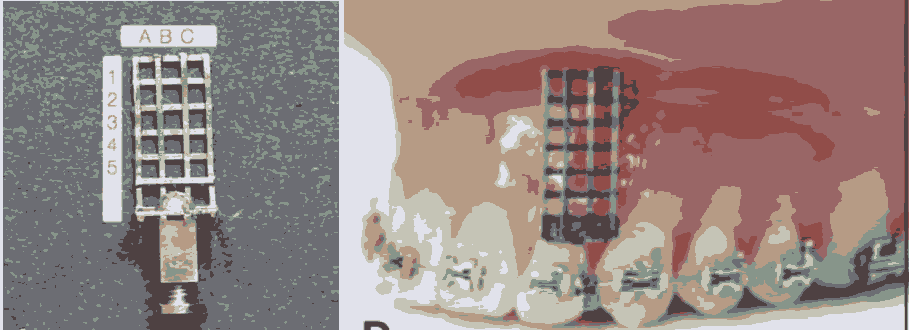
Figure 11: Implant placement by grid method.
A straight, rectangular .016" x .022" stainless steel wire is used to fabricate the miniscrew grid. A three - column grid, in which each cell measures about 1mm2is formed. The required length of the grid (generally, 5 - 6mm apical to the alveolar crest) is determined by the desired miniscrew insertion point.
Implant maintenance:
Multiple studies such as Kim WJ et al(2005), Miyawaki S et al(2003), HS Park et al (2006), Orenstein IH et al (1998), showed that the diameter of the screw of 1mm or less, inflammation of the peri-implant tissue and the high mandibular plane angle cases (ie, thin cortical bone) were associated with the mobility (i.e failure) of the micro-implant, thereby giving more emphasis to the implant maintenance by the patient.
Indications
Anchorage control, in orthodontic treatment, is essential for success. Dental implants can serve as firm anchorage units, due to the stability in the bone. They have been applied in the following situations.
1) Intrude/extrude teeth
• Intrusion of the posterior teeth
• Intrusion of over erupted maxillary molars.
• Intrusion of the maxillary anterior teeth in patients with vertical maxillary excess or excessive gingival display.
• Extrusion of impacted teeth.
2) Close edentulous spaces so prosthesis is not required27,28,29
• Unilateral or bilateral molar extraction sites closed by translating the adjacent teeth bodily without tipping.
• An edentulous area due to agenesis of premolars in which molar mesialization is indicated without loading the anterior teeth for anchorage.
3) Reposition malposed teeth.
Implants provide absolute anchorage for re-establishing proper anteroposterior (uprighting) and mediolateral positions for malposed molar abutment as a preprosthetic correction.
4) Treat partial edentulism.
Many posterior teeth are missing and the teeth must be moved in one direction, the use of implants is particularly helpful
5) Vertical malocclusion cases.
Micro-implant mechanotherapy is useful in patients with high mandibular plane angles or patients with a clockwise rotational growth tendency. Incorporating the mini-implant anchorage to control the tendency toward the bite opening and/or clockwise mandibular rotation is managed.
6) Correct undesirable malocclusion.
• Class I malocclusion with mild to moderate crowding cases are treated without extraction by group distalization of teeth. (en masse retraction)
• In the treatment of maximum anchorage retraction cases. (premolar extraction cases)
• Distalization of maxillary molars in correcting class II malocclusions without any deleterious side effects.
• Correcting class III anterior crossbite by retracting the entire mandibular arch.
7) Reinforce anchorage.
Palatal implants have been developed anchorage reinforcement. An endosseous orthodontic implant anchor system was placed in anterior palatal area and attached to the posterior teeth in class II malocclusion patients where extraction of premolars and retraction of anterior teeth is required.
8) Stabilization for teeth, with reduced bone support. Implants provide attachments for wires or other devices to positionally stabilize periodontally weakened teeth.
9) Provide orthopaedic anchorage.
Palatal expansion can be induced by means of palatal implants even in, partially edentulous patients or children with congenital diseases that result in facial developmental defects or missing teeth. In case of congenital anomalies, implants can promote orthodontic and orthopaedic therapy and accelerate jaw movement by sutural distraction.
Contraindications
1) Mixed dentition where developing permanent teeth will interfere with the placement of the miniscrews (US Food and Drug Administration has approved orthodontic miniscrews for adults and adolescents of age 12 and older only).
2) Midpalatal region of the growing patient, where the micro implants can restrict the horizontal growth of the maxilla.
3) In patients with systemic alterations in bone metabolism due to disease, medication, or heavy smoking.
Absolute Contraindications
• Severe systemic disorder. eg osteoporosis
• Psychiatric diseases. eg psychoses dysmorphobia Alcoholics drug abusers.
• Relative contraindications
• Insufficient volume of bone Poor bone quality
• Patients undergoing radiation therapy Insulin dependent diabetes
• Heavy smokers
Recent Advances
Bicortical Microimplant:
Jian-chao Wu et al in 2007 described bicortical microimplant with 2 anchorage heads. They used it for mesial movement of posterior tooth in the beagle dog. Single anchorage unit is provided by an implant, thus it lacks rotational control, this increases the friction force and extends the total treatment time.
A new bicortical microimplant with 2 anchorage units for applying bilateral forces was designed. The microimplants were of diameter 1.15 mm with 12 to 14 mm length, in a cylindrical shape with 1 slot on each head. Mesial displacement of posterior teeth without rotation in beagle dogs was achieved by bilateral orthodontic force. (Fig.12)
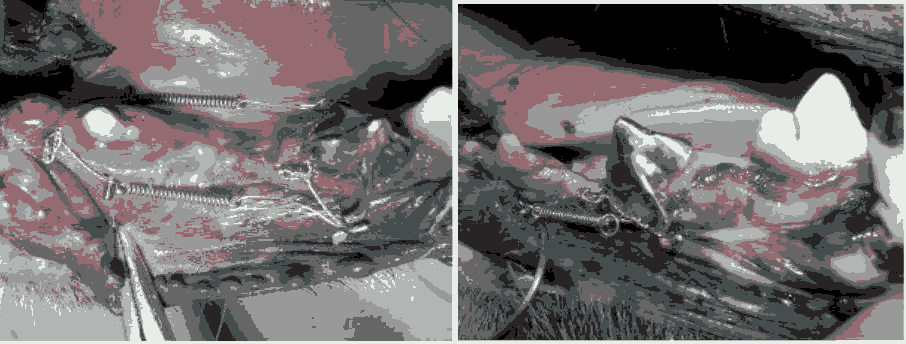
Figure 12: Bicortical Implant.
Resorbable Screws For Orthodontic Anchorage:
The ideal solution would be to use an implant which would serve the purpose of anchorage unit and be easily removable, or resorbed within the tissues.
Absorbable screws are made of a resorbable copolymer, a polyester derivative of L-lactic and glycolic acids. Poly Llactic/ polyglycolic acid (PLA/PLGA) copolymer degrades and resorbs in vivo by hydrolysis into L-lactic and glycolic acids which are then metabolized by the body. The material is non-toxic, non-irritating and 100% amorphous, metabolizing to carbon-di-oxide and water. The potential advantages of bioresorbable implants include less stress shielding of the bone that would be expected with metallic implants, less interference with modern imaging techniques, and elimination of the need for subsequent operations to remove the implant.
Biocompatibility:
Cutright in 1971 found excellent biocompatibility and slow biodegradation of PLA have been documented, since the first experiments: no inflammatory cell infiltrations have been reported, and foreign-body reactions were limited to around the implanted material.
Miller in 1977 Copolymers of PLA and PGA (PLGA) offer the capability of altering the degradation rate and mechanical properties of implants by changing the PLAPGA ratio, which offers the potential to develop sitespecific bone fixation and soft tissue-anchoring devices. Complete absorption of PLGA 75/25 has been reported in 220 days, PLGA 50/50 in 180 days, and PLGA 82/18 in 180-450 days.
Patients’ Perceptions
Lee et al in 2008 conducted a study to determine patient’s expectations, acceptance, and experience of pain with microimplant surgery compared to other orthodontic procedures. Authors found that unlike other orthodontic procedures, patients expected to experience a significantly higher level of pain with microimplant surgery than they experienced. The postoperative pain experienced decreased continuously from day 1 to day 7 for all orthodontic procedures. Most patients were satisfied with the microimplant surgery (76%) and would recommend it to a friend or family member (78%).
Patients tended to overestimate the pain anticipated with microimplant surgery. Patients accepted the surgery and recommended it to others.
Conclusion
Implants help the Orthodontist to overcome the challenge of unwanted reciprocal tooth movement. The Skeletal orthodontic anchorage obviates the need for significant patient compliance, particularly with regard to extraoral appliances, and allows more predictable treatment results. This also allows an overall decrease in the number of orthognathic surgery cases. Skeletal orthodontic anchorage is rigidly fixed to bone, molars can be moved in any direction without taxing anchorage and the occlusal plane can be controlled by orthodontists, without the need for surgery. The Skeletal orthodontic anchorage is quite effective biomechanics for adult patients, retreatment cases, and patients with complex orthodontic problems.
Contemporary orthodontic treatment requires a short treatment time and minimum patient co-operation while offering the maximum treatment efficiency. Conventional means of achieving orthodontic anchorage have a number of shortcomings like anchorage loss, cumbersome anchorage appliance and extensive patient compliance. These shortcomings are overcome by, microimplants (miniscrews) as skeletal orthodontic anchorage. Overall, TADs have expanded and improved the scope and envelope of orthodontic treatement.
References
- Angle, Edward Hartley. "The latest and best in orthodontic mechanism." Dental Cosmos 71 (1929): 409-421.
- Weinstein, Sam, Haack Donald C, Morris Liohtle Y, and Snyder Bruce B, et al. "On an equilibrium theory of tooth position." The Angle Orthodontist 33, no. 1 (1963): 1-26.
- Pilon, Jack JGM, Kuijpers-Jagtman Anne M, and Maltha Jaap C. "Magnitude of orthodontic forces and rate of bodily tooth movement. An experimental study." Am J Orthod Dentofac Orthop 110, (1996): 16-23.
- Daskalogiannakis, John, Miethke Rainer R, and McNamara James A. Glossary of orthodontic terms. Batavia, IL, USA: Quintessence Publ., 2000.
- Chaddad, Karim, Ferreira AndréF H, Geurs Nico, and Reddy Michael S. "Influence of surface characteristics on survival rates of mini-implants." Angl Orthodon 78, (2008): 107-113.
Author Info
Aravindaksha Rao, Deepak C, Kritika A and Deenadayalan P*
Department of orthodontics, SRM Kattankulathur Dental College and Hospital, Chennai, IndiaCitation: Aravindaksha Rao, Deepak C, Kritika A, Deenadayalan P Temporary Anchorage Devices: An Insight, J Res Med Dent Sci, 2021, 9(11): 1-6
Received: 01-Dec-2021 Accepted: 15-Dec-2021 Published: 22-Dec-2021
