Review Article - (2022) Volume 10, Issue 10
Syndromes Associated to Cleft Lip and Palate: A Review
Vinus Shivlani*, Priyanka Niranjane, Ranjit Kamble and Pratiksha Lakhe
*Correspondence: Dr. Vinus Shivlani, Department of Orthodontics and Dentofacial Orthopedics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of medical sciences (Deemed to be University) Sawangi (Meghe), Wardha, Maharashtra, India, Email:
Abstract
Cleft lip and palate is the most common birth defect involving the Orofacial region caused due to atypical embryonic development. It is a congenital anomaly which is characterised by the splits in the face and within the oral cavity of the child. There are various syndromes reported in the literature that are related to cleft lip and/or palate. Further, in this review article the most commonly occurring syndromes related to Orofacial cleft will be enlightened in along with their salient features. These syndromes are broadly categorized on the basis of their mode of inheritance as autosomal dominant and autosomal recessive syndromes.
Keywords
Cleft lip and palate, Syndromes, Congenital
Introduction
Any inborn error in morphogenesis is presented by a congenital structural defect in the body which may involve one or more systems. The one such most frequently encountered congenital defect in children is presence of cleft lip and palate [1]. The line of cleft begins at the lateral part of upper lip then runs through philtrum to the alveolus between lateral incisor and canine. The cleft anterior to incisive foramen is the cleft of primary palate. The median labial cleft is of rare occurance. It develops due to deficiency or absence of globular process of median nasal process. It may vary in severity from a slight notch in vermilion border to the deficiency of the middle part of the nose [2]. The defect can be unilateral or bilateral. Recent studies suggests that, female shows greater incidence of an isolated cleft palate, whereas, cleft lip associated with cleft palate is common in male. There are numerous factors that contribute to development of this congential anomaly. It is believed that cleft lip and palate develops as a combination of genetic and environmental factors. The other cause is some medications like anticonvulsant drugs taken by mother during pregnancy may develop orofacial defect in the child. There are numerous other factors which contribute in development of cleft. These include Vitamin deficiency particularly folic acid and vitamin A deficiency, circulating substances like Alcohol, toxins. Physical, emotional, traumatic stresses during pregnancy, lack of inherited developmental force, mechanical disturbances in which size of tongue may prevent fusion of palatine shelves and defective vascular supply to the area are the other causative factors. Despite various clinical and experimental investigations, the exact cause is still unknown; however genetic reason is still the most important single factor. There are broadly two categories of cleft syndromic and non-syndromic cleft. Syndromic cleft is presence of additional developmental deformities other than cleft example hypodontia, lip pits etc. whereas the non-syndromic cleft have no other developmental defect other than cleft.
There are various problems associated with cleft which includes-Speech difficulty, increased risk of ear infection and hearing loss, difficulty in eating, dental problems, esthetic concern which causes psycological disturbance for both parent and the child. A comprehensive and multidisciplinary approach involving medical as well as dental health care in association with speech pathology, otolaryngology, audiology, genetics, nursing care, mental health and social medicine plays a major role in management of cleft patients. Evidence of an important entity that is occurance of cleft lip and palate in association to various syndromes has been a prime consideration. There are numerous syndromes which are associated with this orofacial defect and are greatly discussed.
Literature Review
Objectives
• To review the syndromes associated with cleft lip and/or palate.
• To review etiologic factors and clinical signs associated with the various syndromes.
• To discuss the associated complications with the syndromes (Figure 1).
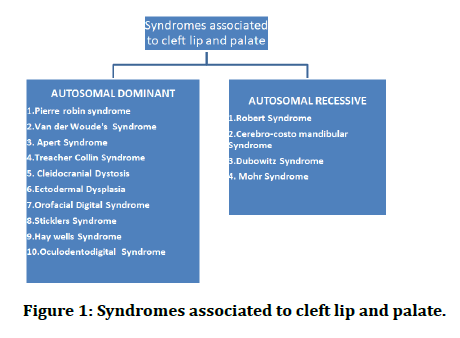
Figure 1: Syndromes associated to cleft lip and palate.
Autosomal dominant
Pierre robin syndrome
Etiology: The Pierre Robin syndrome is due to mutations in chromosomes 2, 4, 11, or 17. Some studies says that alterations in gene SOX9 or KCNJ2 (on chromosome 17) causing this syndrome [3].
Clinical features
• Pierre Robin syndrome is a classical triad of Glossoptosis, micrognathia and upper respiratory obstruction. The syndrome is commonly associated with Cleft Palate.
• Clinically, the small and incompletely developed mandible ultimately causes the upper airway obstruction [2].
• Micrognathia can clinically be diagnosed as underdeveloped mandible with shorter mandibular length and greater mandibular angle.
• Glossoptosis is characterized by abnormal positioning of the tongue in the direction of pharynx.
• Cleft Palate is commonly characterized by U-shaped palate and rare occurrence of V-shaped palate is evident.
Complications: The major problems in Pierre Robin Syndrome are due to blockage in upper respiratory tract. The other complications include respiratory difficulty, difficulty in feeding. The long term complications include hypoxic injury, cerebral impairement, cor pulmonale, pulmonary hypertension and hypoxaemia.
Van der woude’s syndrome
Van der woude syndrome is a syndromic cleft and a rare congenital malformation. It is inherited by autosomal dominant mode. Familial inheritance is verified in cases with bilateral lip pits.
Etiology: The most common etiologic factor for development of Van der woude syndrome is the failure of complete fusion of palate and lips at around 30-45 days of postconception.
Clinical features
• Clinical variation of cleft has a range from unilateral to bilateral cleft and cleft lip associated with cleft palate or isolated cleft palate.
• The presence of lower lip pit is another important entity. The classical type of lip pit is bilaterally present pits on either side of midline. There may be presence of unilateral or a median pit which shows incomplete expression of the trait.
• Presence of hypodontia, ankyloglossia, narrow arched palate is other clinical findings.
Complication
• Presence of rare limb abnormalities.
• Presence of congenital brain abnormalities.
• Presence of congenital Heart defects.
Apert syndrome
Apert Syndrome is rare congenital disorder which is a type of acrocephalodactyly (type 1) [4].
Etiology: It represents autosomal dominant inheritance due to alterations in fibroblast growth factor receptor gene. It is rare syndrome and is seen in 1 in 65,000 babies.
Clinical features: It is characterized by craniofacial deformities, acrcephaly, hyperteleorism, and flattened nose.
The oral manifestations include, high-arched palate, maxillary hypoplasia, crowding in teeth, delayed dentition, ectopic teeth, abnormal arrangement of teeth, and crowding in teeth. Pseudoprognathism is sometimes associated with this syndrome [5].
Complications
• A rare occurance of internal organ disorders which includes renal, cardiac, gastrointestinal and genitourinary systems.
• Hemivertebra, cortical defects, ventriculomegaly, and vertebral malsegmentation may occur.
• Upper respiratory tract disorders, sleep apnea, and several mental disorders are seen in association [6].
Treacher collin syndrome
Treacher collin syndrome is the craniofacial defect with autosomal dominant type of inheritance. It has major symptoms of cleft palate and hearing loss.
Etilogy: The major etiologic factors for this syndrome involves mutations in TCOF1 (80% cases), POLR1C, or POLR1D gene. It is believed that these genes play important role in the growth of bones and other tissues in face [7].
Clinical features
• It is characterized by Hypertelorism, downward slanting of lower palpebral fissure, malformation of external ears, parrot beak nose.
• Oral manifestations include dysplasia or aplasia of minor salivary glands, Hypoplasia of zygomatic bone or maxilla, underdeveloped mandible, teeth agenesis and discolouration.
Complications
Treacher collin syndrome may cause severe eye abnormalities which may cause vision loss. It may also cause delay in motor and speech development.
Cleidocranial dystosis
Cleidocranial dystosis is a predominantly autosomal dominant syndrome which is primarily characterized by dysplasia of bone and teeth.
Etiology: It is a familial syndrome caused due to alterations in Core Binding Factor Alpha (CBFA) gene on chromosome 6p218. If a parent has this condition then there are 50:50 chances that the child will be born with similar defect. Also there are equal chances of its occurance in boys and girls [8].
Clinical features
• It is characterized by premature closing of section between front and sides of skull.
• Underdeveloped or total absence of collar bone is a characterstic feature.
• The child has a short stature and wide nasal bridge (hypertelorism).
• The oral manifestations involves presence of high arched palate, presence of cleft, delayed shedding of primary teeth, delay in appearance of permanent teeth, malocclusion, supernumerary teeth and sometimes cyst in oral tissue.
Complications: These individuals are at an increased risk for developing upper respiratory tract infections, severe problems like hearing loss, recurrent ear infections and sinus infections.
Ectodermal dysplasia
Etiology: The major etiologic factor for ectodermal dysplasia is mutation in cell signal process involved in induction and development of ectodermal structures and their interaction with mesodermal structures are responsible for development of clinical features of the disorder [9].
Clinical features
• It presents classical features of hypohydrosis, hypotrichosis, hypodontia.
• The supraorbital and frontal bosses are prominent.
• Reduced sweating and xerostomia are evident.
• Sparse and curly hair with absence or malformation of eyebrows.
• The major oral manifestations include malformation of teeth, cleft lip, presence of peg laterals, anodontia and prone to caries.
Complications: The individuals with ectodermal dysplasia may develop complications like febrile seizures, potential brain damage, recurrent pneumonia, asthma and frequent hospitalization [9].
Oro-facial digital syndrome
Etiology: This is a rare group of hereditary disorder with X-linked dominant male lethal pattern affecting oral cavity, face and digits. The first case was reported in 1941. The major etiologic factor is mutation in OFD1 gene which encodes for basal body OFD1 protein.
Clinical features
• The disorder presents with several phenotypic variants.
• General signs include digital anomalies: brachydactyly, syndactyly, polydactyly.
• Facial features include frontal bossing, euryopia, hypoplasia of nasal cartilages, zygomatic hypoplasia.
• The oral manifestations include pseudocleft of midline of upper lip, cleft palate, tongue hamartomas, supernumeraries and hypoplasia.
Complications: The additional findings related to this syndrome include pancreatic, hepatic and/or ovarian cyst. Moreover the child may also have hearing defecfs.
Sticklers syndrome
Etiology: Sticklers syndrome is mainly caused due to alterations in genes responsible for collagen formation which are the building block of many types of connective tissues.
Clinical features
• The clinical findings include visual deformities like myopia and retinal detachment [10].
• Facial features include flattening of midface and nasal bridge in addition to facial asymmetry.
• The oral manifestations include submucosal cleft palate and micrognathia.
• The associated joint deformities include bony enlargement of joint, joint hypermobility and hip joint deformity [11].
Complications: Potential complications of Sticklers syndrome include hearing loss, Ear infections, feeding difficulties, breathing difficulties, blindness, cardiac problems, and dental problems.
Hay wells syndrome
This syndrome is also called as ankyloblepharonectodermal dysplasia-cleft lip and/or palate syndrome (AEC) syndrome.
Etiology: This is caused by alterations in TP63 (Tumor protein 63) gene which affects the protein (P63) synthesis which thereby affects the development of organs derived from ectoderm. This includes skin, hair, nails, and mucous membrane of mouth and glands of skin
Clinical features
• Common symptoms of this syndrome includes fusion of upper and lower eyelids by abnormal fibrous strands of tissue, mild to moderate skin erosions, abnormal hair growth and cleft lip and/or cleft palate.
• Other features involve abnormalities of nails, abnormal hair color, limb and dental malformation.
Complications: These include oroauditory abnormalities involving recurrent otitis media, canal stenosis contributing to hearing loss, and delay in speech development [12].
Oculodentodigital syndrome
It is also termed as Oculotdentoosseous Dysplasias (ODOD).
Etiology: This is caused by alterations in connexin 43 gene GJA1. It shows autosomal dominant pattern of inheritance and there are 50% chances of occurance of syndrome in the child if the parent is affected with the same [13].
Clinical features
• The syndrome presents with a typical facial appearance and shows variable eye, tooth and digits involvement.
• Dental deformities include hypodontia, enamel hypoplasia, premature loss of teeth, selective missing tooth and Taurodontism.
• Ocular deformities involve small cornea, short opening between the eyelids, glaucoma and cataract.
• The tibia, fibula and femur have increased length; the major bones of arms (humerus, radius, and ulna) are broad, abnormal finger shape, bent fifth finger, syndactyly of 4th and 5th fingers [13].
Complications: The complications include hearing loss, bowel dysfunction, and rare occurance of neurogenic bladder, ataxia, and cardiac deformities.
Autosomal recessive
Robert syndrome: It is a rare genetic defect with recessive mode of inheritance which affects diverse group of people and is spread worldwide.
Etiology: The mutation in ESCO2 gene on chromosome 8p21 is responsible for development of clinical manifestation of Robert Syndrome.
Clinical features
• The major clinical manifestations involve symmetric underdeveloped limbs and craniofacial abnormalities.
• The limb abnormalities may vary from shortening to complete absence of the limbs which involves short arm bones, fused fingers and missing thumb.
• Craniofacial abnormalities involve exopthalmos, double orofacial cleft, hypertelorism, wide nasal bridge and micrognathia.
• The major feature in this involves tetraphocomelia in association with oligodactyly, radial aplasia or dysplasia.
• Systemic manifestations include presence of horseshoe shape kidney, hydronephrosis, ureterstenosis and persistent ductus arteriosus.
• Some rare features involve hydrocephalus, microcephaly and femoral tibial ankylosis [14].
Complications
• It has been observed that many patients are born with growth retardation and many die in early childhood.
• Also mental retardation is evident is several cases.
• Patients born with Robert syndrome present a high degree of orthopedic deformities.
Cerebro-costo mandibular syndrome
Etiology: The major etiologic factor for this syndrome is mutation in SNRPB, which codes parts of major spliceosome. It is found that these alterations cluster in alternatively spliced regulatory exon which ultimately results in alteration of SNRPB expression [15].
Clinical features
• The clinical manifestations involve combination of mandibular hypoplasia and gap in between the ribs which causes rib fracture.
• Other features involves tracheal cartilage abnormalities, elbow hypoplasia and spina bifidia.
• The major oral manifestation involves presence of cleft lip with palate and sometimes cleft of soft palate, high arched palate.
Complications: Patient presents with serious complications like
• Upper airway obstruction
• Language disorder
• Conductive hearing loss
• Mental retardation [15].
Dubowitz syndrome
Etiology: This syndrome is caused by alterations in NSUN4 in addition to LIG4 genes. Some others believe that this syndrome is caused by small additions of deletions in of DNA which are termed as micro duplications and micro deletions respectively [16].
Clinical features
• Patients present with a characteristic narrow or triangular shaped faces with sloping forehead.
• Dropping of upper eyelid, epicanthal folds covering inner corner of eye, telecanthus and hypertelorism, otitis media, hyperopia, cataract are other common features.
• Oral deformities involves narrow and high arched palate, crowded, missing or rotated teeth, delayed eruption of teeth, cleft palate, sub-mucous cleft palate, cleft uvula are mostly seen.
Complications: The major complications involves
• Growth retardation
• Altered speech and overall behavior changes like hyperactivity is observed.
• Feeding difficulties, food refusal, regurgitation are observed in various children [16].
• Problems with esophageal and gastrointestinal system.
• Other systemic complications involve cardiac abnormalities, neurogenic abnormalities and migraine headaches.
Mohr syndrome
It is also called as oral-facial-digital syndrome type 2. This disease was first diagnosed by Mohr in 1941 and is known to be a familial disease.
Etiology: This syndrome is caused by mutation in chromosome X, the gene is not yet identified for Mohr syndrome and diagnosis is done by typical clinical findings. This is a very rare syndrome with prevelance of 1/1000000 Worldwide.
Clinical features
• The individuals with Mohr syndrome presents characterstic feature of postaxial and preaxial polydactyly in hands and feet respectively [17].
• The oral findings include complete cleft palate with absence of uvula, absence of central incisors, micrognathia, high arched palate and polylobed tongue.
• The other features include lowset ears, epicanthic folds, bilateral hallucial triplication, hypertelorism, bifid nasal tip and congenital heart defects.
Complications
The individual affected may present with the following complications
• Transmission deafness
• mental retardation
• Tachypnea and other pulmonary complications [18]
Discussion
The global prevelance of congential cleft lip and palate serves a need for analysis of proper treatment modalities to the suffering infants [19]. Also the presented review emphasizes on the various syndromes that are reported to be related to this defect. The presented data classifies these syndromes on the basis of their mode of inheritance as autosomal dominant and recessive traits.
Apart from this, there are numerous other syndromes which are found to be related to orofacial cleft, these includes: Danky Walker syndrome, Popliteal pterygium syndrome, Turner syndrome, Blepharo-chelio-dontic syndrome, Nager's Acrofacial Dysosotosis, Mobius syndrome, Hallerman Streiff syndrome, Goldenhar's Syndrome, Beckwith Wiedemann syndrome and many more. In India, the prevelance of cleft lip with palate is 1.09 among 1000 births. A study provides an accurate survival report of 98.4% after a follow up period of 1 year. Thus, this deformity subjects to the multitude of treatment from early age [20-23].
Conclusion
Orofacial cleft features a ubiquitous stratification of the birth deformities and major health concern is witnessed in this regard 20. This cleft lip with palate is second most common congenital defect among infants, first being congenital heart defects. The prevalence of this congenital deformity is nearly 1:1000. This figure is nowadays more frequently seen in certain specific ethnic groups. This malformation can be either seen in isolation or may be seen combined with other syndromes affecting other major systems of body. The main etiologic factor for such congenital defects is proven to be genetic but some other important etiologic factors that occur frequently have been discussed briefly. These syndromes lead to certain severe systemic diseases that could hamper the normal physiologic processes of the body. Such severe additional malformations include respiratory complications like tachypnea, gastrointestinal disturbances, mental retardation and many more. The treatment modalities include a multidisciplinary approach to correct the defect and provide lifetime maintenance.
References
- Kasatwar A, Borle R, Bhola N, et al. Prevalence of congenital cardiac anomalies in patients with cleft lip and palate – Its implications in surgical management. J Oral Biol Craniofac Res 2018; 8:241–244.
- Shafer WG, Maynard KH and Barnet Ml, et al. A text book of oral pathology, 9th Edition. Saunders, Philadelphia. 1963; 768.
- Izumi K, Konczal LL, Mitchell AL, et al. Underlying genetic diagnosis of Pierre Robin sequence: retrospective chart review at two children's hospitals and a systematic literature review. J Pediatr 2012; 160:645-650.
- Bhatia PV, Patel PS, Jani YV, et al. Apert's syndrome: Report of a rare case. J Oral Maxillofac Pathol 2013; 17:294.
- Kumar GR, Jyothsna M, Ahmed SB, et al. Apert's syndrome. Int J Clin Pediatr Dent 2014; 7:69.
- Cohen Jr MM, Kreiborg S. Agenesis of the corpus callosum: Its associated anomalies and syndromes with special reference to the Apert syndrome. Neurosurg Clin N Am 1991; 2:565-568.
- Thomson A. Notice of several cases of malformation of the external ear, together with experiments on the state of hearing in such persons, Monthly. J Med Sci 1846; 7:420.
- Koch PE, Hammer WB. Cleidocranial dysostosis: review of the literature and report of case. J Oral Surg 1978; 36:39-42.
- Khan SA, Rukan A, Ullah A, et al. Homozygous variants of EDAR underlying hypohidrotic ectodermal dysplasia in three consanguineous families. Eur J Dermatol 2020; 30:408-416.
- Mohr OL. A hereditary sublethal syndrome in man. J Craniofac Surg 1941; 14:3-18.
- Stickler GP. Hereditary progressive arthroopthalmopathy. Mayo Clin Proc 1965; 40:433-455.
- Tadini G, Santagada F, Brena M, et al. Ectodermal dysplasias: The p63 tail. G Ital Dermatol Venereol 2013; 148:53-58.
- Jyotsna M, Madhu D, Altaf H, et al. Roberts-SC syndrome, a rare syndrome and cleft palate repair. Indian J Plast Surg 2008; 41:222-225.
- Al Kaissi A, Csepan R, Klaushofer K, et al. Femoral-tibial-synostosis in a child with Roberts syndrome (Pseudothalidomide): a case report. Cases J 2008; 1:1-4.
- McNicholl B, Egan-Mitchell B, Murray JP, et al. Cerebro-costo-mandibular syndrome: a new familial developmental disorder. Arch Dis Child 1970; 45:421-424.
- Tsukahara M, Opitz JM. Dubowitz syndrome: review of 141 cases including 36 previously unreported patients. Am J Med Genet 1996; 63:277-289.
- Berthold F, Fuhrmann W, Lampert F. Fatal aplastic anaemia in a child with features of Dubowitz syndrome. Eur J Pediatr 1987; 146:605–607.
- Mohr OL. A hereditary sublethal syndrome in man. J Craniofac Surg 1941; 13:321-326.
- Mallick R, Pisulkar SK, Reddy SG, et al. Assessment of Outcomes of Immediately Loaded Dental Implants in Orofacial Cleft Patients: Protocol for a Single-Arm Clinical Trial. JMIR Res Protoc 2021; 10:25244.
- Kasatwar A, Borle R, Bhola N, et al. Prevalence of congenital cardiac anomalies in patients with cleft lip and palate – Its implications in surgical management. J Oral Biol Craniofac Res 2018; 8:241–244.
- Shrey S, Singam A, A comparative study of atracurium and cisatracurium in paediatric cleft lip and cleft palate surgeries. Res J Pharm Technol 2020; 13:867-870.
- Hazare A, Kamble R, Shrivastav S, et al. Association between Genetic Polymorphism in Interferon Regulatory Factor 6 (IRF6) and Non-Syndromic Cleft Lip and Palate Cases in Central Indian Population. J Evol Med Dent Sci 2020; 9:641-644.
- Gosavi S, Shrivastav S, Kamble R, et al. Multidisciplinary Approach for the Management of a Case of Bilateral Cleft Lip and Palate (Baru’s Score 5) Using Modified Dentoalveolar Distractor. J Evol Med Dent Sci 2020; 9:3276–3279.
Author Info
Vinus Shivlani*, Priyanka Niranjane, Ranjit Kamble and Pratiksha Lakhe
Department of Orthodontics and Dentofacial Orthopedics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of medical sciences (Deemed to be University) Sawangi (Meghe), Wardha, Maharashtra, IndiaCitation: Vinus Shivlani, Priyanka Niranjane, Ranjit Kamble, Pratiksha Lakhe, Syndromes Associated to Cleft Lip and Palate: A Review, J Res Med Dent Sci, 2022, 10 (10): 224-229.
Received: 02-Aug-2022, Manuscript No. JRMDS-22-47361; , Pre QC No. JRMDS-22-47361(PQ); Editor assigned: 04-Aug-2022, Pre QC No. JRMDS-22-47361(PQ); Reviewed: 18-Aug-2022, QC No. JRMDS-22-47361; Revised: 03-Oct-2022, Manuscript No. JRMDS-22-47361(R); Published: 13-Oct-2022
