Research Article - (2023) Volume 11, Issue 1
Superior Mesenteric Vein, Splenic Vein And Portal Vein Thrombosis With Bowel Gangrene In Covid-19 And HIV Positive Patients: A case report
Juee Meghe1*, Meenakshi Yeola2, Abhyuday Meghe3 and Yeshwant Lamture4
*Correspondence: Juee Meghe, Department of Medicine, Krishna Institute of Medical Sciences, Karad, Maharashtra, India, Email:
Abstract
COVID-19 pandemic which broke out in Wuhan province of China in December of 2019 has rapidly spread globally with millions of deaths in the past one and half year. Along with severe lower respiratory tract infection it also causes coagulopathy due to an imbalance in the coagulation homeostasis. Here we report a case of superior mesenteric artery thrombosis with bowel gangrene in a COVID-19 and HIV positive female patient with its management. A female patient presented with complaint of pain in abdomen since 15 days. On per abdominal examination the abdomen was tender with guarding, rigidity and distention. X-ray abdomen ERECT was done which was significant of free gas under right dome of diaphragm. CECT abdomen pelvis was significant of thrombus in the superior mesenteric vein, portal vein, splenic vein with the evidence of perforation. Urgent laparotomy was done, after surgery patient developed multiple opacities in bilateral lung and repeat RT-PCR was done which turned out to be positive for COVID-19. Unfortunately patient died on 4 postoperative days due to ARDS related to COVID-19 pneumonia. Elderly male patients with comorbidities such as hypertension and diabetes mellitus are more likely to develop severe COVID-19 complications and are more susceptible to thromboembolism. Drugs such as low molecular weight heparin should be administered as soon as a patient is hospitalized for COVID-19 infection to prevent vascular thrombosis and end organ failure. Immunosuppressed patients with conditions like cancer, HIV, TB, etc. should be monitored under intensive care following the government protocols. Once the patients are recovered from COVID-19, they have to take care of their high blood pressure and blood sugar level should be monitored and kept under control. It is advisable that the patients should get their cardiac investigations done within 21 days of their positive results. This can prevent post COVID complications like MI, stroke DVT, PE, etc.
Keywords
COVID-19, HIV, Superior mesenteric vessels, Bowel ischemia, Thrombosis
Introduction
COVID-19 pandemic which broke out in Wuhan province of China in December of 2019 has rapidly spread globally with millions of deaths in the past one and half year. Along with severe lower respiratory tract infection it also causes coagulopathy due to an imbalance in the coagulation homeostasis [1]. Pathogenicity of SARS-CoV-2 is very crucial for understanding the progression of the disease and prevention of its complications. SARS-CoV-2 belongs to the genera beta Coronavirus containing single stranded RNA associated with a nucleoprotein within a capsid comprised of matrix protein. Important mechanism being that of angiotensin converting enzyme 2 receptors which is widely expressed including respiratory system, cardiovascular system, central nervous system GIT, renal system and adipose tissue [2]. In certain studies it was found that cardiac pericytes express ACE-2 which is related to underlying cardiac lesion in COVID-19 positive patients [3]. Angiotensin 2 is known as one of the potent vasoconstrictors and increases hypercoagulability by increasing expression of tissue factor and plasminogen activator inhibitor 1. Hypercoagulability is a crucial hallmark of inflammation and severe organ damage in COVID-19 patients. Coagulopathy and elevated D dimer levels in a COVID-19 patient have been associated with a poor clinical prognosis and higher in patient mortality rate [4]. As the patient is HIV positive and severely immune compromised this can make patient more prone to non-contagious diseases which can affect the cardiovascular system, in past studies it is proven that high numbers of HIV related deaths had been succumbed to influenza which makes these patients highly prone for contracting COVID-19 [5]. In contrast the suppressed immunity and low CD4 count may protect HIV positive individuals from developing the cytokine storm observed in patients with COVID-19 [6].
Case Presentation
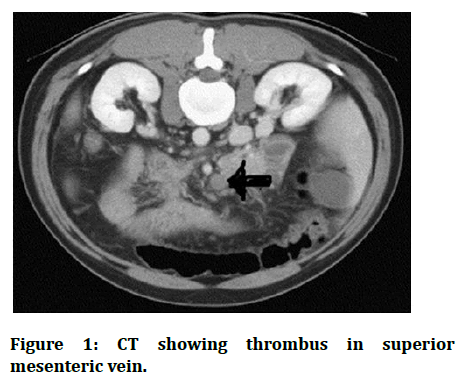
32 years old female patient presented to the casualty with complaint of pain in abdomen since 15 days. Patient was apparently alright 15 days back when she started complaining of pain in abdomen which was insidious in onset and gradually progressed in severity. The pain was dull aching in nature, non-radiating with no aggravating and relieving factors. History of loss of appetite was present with no history of fever, nausea, vomiting, trauma, weight loss, altered bowel and bladder habits. Patient attended menarche at the age of 14 and had regular menstrual cycles with 3-4 days of bleeding and it was a cycle of 30 days with dysmenorrhea. Patient has one live birth which was full term normal delivery. Patient had mixed diet with no addiction and was not a known case of HTN, DM, TB and BA. Patient was a known case of HIV positive status for which the patient was on anti-retroviral therapy with no significant family history. On examination patient conscious and well oriented to time, place and person. Lying comfortably on the bed with pulse rate of 90 beats per minute and blood pressure being 120/80 mmhg with saturation of 98% on room air. Patient was anaemic with no icterus, no cyanosis, no clubbing, no cervical lymphadenopathy and no pedal oedema. On systemic examination patient had bilateral equal air entry into the lungs with S1 and S2 present on all the auscultator areas of heart. On per abdominal examination the abdomen was tender with guarding, rigidity and distention. Bowel sounds were absent on all the quadrants of the abdomen. X-ray abdomen ERECT was done which was significant of free gas under right dome of the diaphragm. CECT abdomen pelvis was done which was significant of thrombus in the superior mesenteric vein, portal vein, splenic vein with the evidence of perforation peritonitis of the abdomen with bowel necrosis. Urgent exploratory laparotomy was done under general anesthesia. Intra operatively the abdomen was full of fecal matter with the formation of membranes in the abdomen. The perforation was traced 25 cm from the duodenojejunal flexure and resection anastomosis was done (Figure 1).
Figure 1: CT showing thrombus in superior mesenteric vein.
Postoperatively the patient was shifted to SICU for further supportive treatment. After the surgery patient developed multiple ground glass opacities in bilateral lung filed and decision of repeat RT-PCR was taken, which came out positive for COVID-19 infection. Patient was admitted for 6 days on oxygen with ventilator support and died on 4th post-operative day due to ARDS related to COVID-19 pneumonia. The case described is unique in its self as it is rare to see gastrointestinal involvement in a COVID-19 and HIV positive patient. The most common systems which are affected in COVID-19 are cardiovascular and central nervous system and to some extend renal system.
Discussion
COVID-19 pandemic continues to spread worldwide with significant morbidity and mortality in patients with comorbidities, there have been several reports indicating increased coagulation activity in these patients [7]. Thrombotic events include autopsy proven micro vascular thrombosis in a variety of vascular beds likely contributing to end organ function deterioration as well as large vessel thrombosis such as extensive DVTs or arterial thrombosis leading to stroke, myocardial infarction or lower extremity ischemia in otherwise low risk patients [7]. Management of COVID-19 hyper coagulopathy can be cumbersome, due to the acuteness of the illness, a general approach has been recommended for all in hospital patients presenting with coagulopathy. These interventions should include pharmacological thromboprophylaxis, with IV unfractionated heparin or low molecular weight heparin unless contraindicated. Human Immunodeficiency Virus (HIV) infection is often associated with an increased risk of venous and arterial thrombosis, before the widespread use of combination antiretroviral therapy, deficiencies in protein C and protein S and molecules involved in the inactivation of the pro coagulant factor Va and VIIIa, were recognized contributors to venous thrombotic risk in patients with advanced HIV infection [8]. Even under suppressive therapy ART, many HIV infected patients tend to maintain increased levels of immune activation and inflammation, recent studies have shown that HIV replication causes increase in many pro coagulant factors and decrease in multiple anticoagulant factors [9,10]. Several risk factors have been well associated with severe forms of COVID-19, such as older age, male sex, metabolic disorders, cardiovascular and other chronic disease, as we know that many patients living with HIV are often the carrier of theses co-morbidities it is important for a doctor to prevent further complications by providing prophylactic therapy to such patients [11].
Adjunct disease modifying treatment should be made mandatory for patients with HIV positive status along with ART to target excess inflammation and coagulation activation, cardio protective medications such as aspirin, statins and angiotensin receptor blockers are commonly used drugs. Aspirin along with anti-platelet action has broad anti-inflammatory properties and demonstrated potential to reduce T-cell activation, monocyte activation and platelet activation, use of new generation oral anticoagulant drugs such as direct inhibitors to thrombin and factor Xa would represent a novel approach to hyper coagulation during chronic HIV disease but bleeding risks are predictable and become a major treat when considering a treatment strategy.
Conclusion
By now it is certainly clear that, COVID-19 infection is associated with hypercoagulable state and results in worse outcome if associated with any risk factors like diabetes mellitus, hypertension, obesity, thyroid disorders, cancers, or other infections like HIV, TB, hepatitis, etc. It is observed that elderly male with severe COVID-19 infections are more prone to develop thromboembolic complications later in the disease stage or could be developed after a span of 10-15 days. It is suggested that the, patients after getting recovered from COVID-19 infection should have a proper track of their blood pressure and blood sugar and get a thorough cardiac investigation done within 21 days of their positive result, in case of mesenteric ischemia or when abdominal organs are involved contrast enhanced CT scan should be done for diagnosis. This approach can prevent coagulation related complication to a certain degree if done early in the disease when patient is asymptomatic and leads to better prognosis. Patients living with chronic HIV infection who are positive for COVID-19 should be given adjuvant therapy along with ART, as HIV infection is hyper inflammatory state which leads to activation of coagulation cascade.
Sources of Funding
Nil
References
- Karna ST, Panda R, Maurya AP, et al. Superior mesenteric artery thrombosis in COVID-19 pneumonia: An underestimated diagnosis first case report in Asia. Indian J Surg 2020; 82:1235-1237. [Crossref][Googlescholar][Indexed]
- Haimei MA. Pathogenesis and treatment strategies of COVID-19 related hyper coagulant and thrombotic complications. Clin Appl Thromb Hemost 2020; 26:1076029620944497. [Crossref][Googlescholar][Indexed]
- Miesbach W, Makris M. COVID-19: Coagulopathy, risk of thrombosis and the rationale for anticoagulation. Clin Appl Thromb Hemost 2020; 26. [Crossref][Googlescholar][Indexed]
- Cheung S, Quiwa JC, Pillai A, et al. Superior mesenteric artery thrombosis and acute intestinal ischemia as a consequence of COVID-19 infection. Am J Case Rep 2020; 21.[Crossref][Googlescholar][Indexed]
- Mohammed AH, Blebil A, Dujaili J, et al. The risk and impact of COVID-19 pandemic on immunosuppressed patients: Cancer, HIV and solid organ transplant recipients. AIDS Rev 2020; 22:151-157. [Crossref][Googlescholar][Indexed]
- Xu Z, Zhang C, Wang FS. COVID-19 in people with HIV. Lancet HIV 2020; 7:e524-e526. [Crossref][Indexed]
- Bannazadeh M, Tassiopoulos A, Koullias G. Acute superior mesenteric artery thrombosis seven days after discharge for novel Coronavirus pneumonia. J Vasc Surgery Cases Innov Tech 2021; 7:586-588. [Crossref][Googlescholar][Indexed]
- Funderburg NT. Markers of coagulation and inflammation often remain elevated in ART treated HIV infected patients. Curr Opin HIV AIDS 2014; 9:80-86. [Crossref][Googlescholar][Indexed]
- Baker JV. Chronic HIV disease and activation of the coagulation system. Thromb Res 2013; 132:495-499. [Crossref][Googlescholar][Indexed]
- Funderburg NT, Lederman MM. Coagulation and morbidity in treated HIV infection. Thromb Res 2014; 133:S21-S24. [Crossref][Googlescholar][Indexed]
- Etienne N, Karmochkine M, Slama L, et al. HIV infection and COVID-19:Risk factors for sever disease. AIDS 2020; 34:1771-1774. [Crossref][Googlescholar][Indexed]
Author Info
Juee Meghe1*, Meenakshi Yeola2, Abhyuday Meghe3 and Yeshwant Lamture4
1Department of Medicine, Krishna Institute of Medical Sciences, Karad, Maharashtra, India2Department of Surgery, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi, Wardha, Maharashtra, India
3Department of Community Medicine, Acharya Vinoba Bhave Rural Hospital, Sawangi (Meghe), Wardha, Maharashtra, India
4Department of Surgery, Jawaharlal Nehru Medical College and Acharya Vinoba Bhave Rural Hospital, Datta Meghe Institute of Medical Sciences, Sawangi (Meghe), Wardha, Maharashtra, India
Citation: Juee Meghe, Meenakshi Yeola, Zahiruddin Syed Quazi, Abhyuday Meghe, Yeshwant Lamture, Superior Mesenteric Vein, Splenic Vein and Portal Vein Thrombosis with Bowel Gangrene in COVID-19 and HIV Positive Patients: A Case Report, J Res Med Dent Sci, 2023, 11 (01):248-250
Received: 08-Nov-2022, Manuscript No. JRMDS-22-79086; , Pre QC No. JRMDS-22-79086 (PQ); Editor assigned: 14-Nov-2022, Pre QC No. JRMDS-22-79086 (PQ); Reviewed: 28-Nov-2022, QC No. JRMDS-22-79086; Revised: 09-Jan-2023, Manuscript No. JRMDS-22-79086 (R); Published: 16-Jan-2023