Research - (2022) Volume 10, Issue 1
Study of Medical and a Microbiological Study
Gopalsamy Santhanam Prabudoss*
*Correspondence: Gopalsamy Santhanam Prabudoss, Department of General Surgery, Sree Balaji Medical College & Hospital Chromepet, Chennai, India, Email:
Abstract
Necrotizing fasciitis is a progressive, rapidly spreading, inflammatory infection located in deep fascia. It may cause necrosis of skin and subcutaneous tissue and can even result in involvement of adjacent soft tissues such as muscles (necrotizing myositis). In addition to direct spreading of the necrosis to adjacent tissues, distribution of the disease via blood vessels and lymphatic can lead to shock, organ failure and death. Prevalence of this disease in adults is higher than children (0.4 and 0.08 cases for each 100,000 population in adults and children respectively) .The incidence of this disease has increased about five folds during the last decade, which can be partly due to increase in the number of Immuno deficient patients and even may be due to frequent reports during the recent years.
Keywords
Blood vessels, Immune defiency, Myositis, DM
Introduction
There are several predisposing factors that may lead to an increase in the susceptility for persons to this disease. Immune deficiency is the main factor that can be due to diabetes mellitus, complement C4 deficiency, AIDS, malignancies and drugs. In a diabetic patient, with longstanding disease have the combined effects of large vessels atherosclerosis, micro vascular disease of diabetes and diabetic neuropathy. Vasculopathy and neuropathy are synergistic and predispose this patient of foot ulceration, followed by local contamination and invasive infection into the deep compartments, necrosis and suppuration of skin, subcutaneous tissue, introsseous space yield a complex infectious process .The neuropathy of diabetic results in the loss of sensation, degeneration of motor fibers and loss of autonomic Neuro control in the foot. Loss of sensation results in pressure ulceration. Loss of vasomotor control also leads to inadequate cutaneous blood supply. The net connect of these neuropathology changes is that the diabetes are prone to ulceration with secondary invasive infection. After infection, the lesion enters into the deep spaces of the leg; true climb-threatening circumstance exists.
Each factor that influences the health and integrity of the skin or mucus membranes can result in penetration of infection. Primary infection can penetrate due to skin trauma, infected needle in intravenous drug abusers or previous dermatological diseases such as psoriasis and Bed sore. Mucosal membranes in gastrointestinal or genitourinary systems are the other routes of infection. This study was done in an attempt to identify the frequency of Necrotizing Fasciitis in our institution and to analyze the clinical presentation, predisposing factors, comorbid conditions, to determine the bacteriological profile, surgical and resuscitative management and the outcome of this surgical problem [1-10].
Materials and Methods
Study design
The study was a descriptive study of Necrotizing fasciitis. This study involved a single group of patients with Necrotizing fasciitis admitted in Sree Balaji Medical College & Hospital, Chennai-44. Between the period of November 2014 and October 2016. The approval from the ethical committee was obtained to conduct the study.
Inclusion criteria
All cases of Necrotizing fasciitis admitted in Sree Balaji Medical College & Hospital, Chennai-44 between the period of November 2014 and October 2016.
Exclusion criteria
All patients with necrotizing fasciitis leaving before the treatment are complete.
Methodology
Patients with Necrotizing fasciitis admitted and treated in the surgical ward of Sree Balaji Medical College & Hospital, Chennai-44. Between the period of November 2014 and October 2016 are included in the study. Diagnosis was made by combination of clinical and gross anatomical findings during surgery. Demographic patient data was collected.
Patients were interviewed by the researcher regarding history of pre-existing diabetes mellitus, any prior antibiotics used before admission and the duration of symptoms prior to admission, Systolic and diastolic blood pressure and temperature on the day of admission was recorded.
Thorough physical examination was performed to look for any bullae formation. On admission, patients’ blood testing included Haemoglobin, Platelets, RBS, Urea, Creatinine, Sodium and Potassium levels.
Radiograph of the involved area was done to look for subcutaneous gas formation. Treatment was started that includes hemodynamic stabilization, blood-spectrum antibiotics and aggressive wound debridement.
Culture and sensitivities was taken from the infected wound during debridement or fasciotomy, particularly to test for aerobic and anaerobic organisms.
The tissue was homogenized under sterile conditions and cultured in blood and Mc Conkey agar. The culture plates were incubated overnight at 37 áµ?C for aerobic growth.
Bacterial growth was identified by the biochemical test and the resistance pattern by disk diffusion method according to CLSI (Clinical and Laboratory Standards Institute) guidelines.
The tissue sample or the wound swab was inoculated immediately after collection in RCM (Robertson's Cooked Meat) media for further anaerobic culture and identification.
Statistical Analysis
Statistical methods
Descriptive statistical analysis has been carried out on the present study. Results in continuous measurements are presented on Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%). 95% Confidence Interval has been computed to find the significant features. Confidence Interval with lower limit more than 50% is associated with statistical significance.
Statistical software
The statistical software namely, Statistical Package for the Social Sciences software, SPSS 15.0(SPSS Inc., Chicago, IL), and R environment ver.2.11.1 were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables etc.
Results
The study period was from Sree Balaji Medical College & Hospital, Chennai-44. between the period of November 2014 and October 2016. 60 patients of Necrotizing Fasciitis were treated during the study period. The age ranged from 2 -81 years, the mean age being 50.42 ± 17.31 years.
Maximum cases were above the age of 50 years. There were 49 males and 11 females, the male: female ratio being 4:45:1 (Table.1). Out if the 60 patients studied, 17(28.3%) were farmers by occupation (Table 2).
| Male | Female | Total | ||||
|---|---|---|---|---|---|---|
| Age in years | No | % | No | % | No | % |
| <20 | 2 | 4.1 | 2 | 18.2 | 4 | 6.7 |
| 21-30 | 1 | 2.1 | 1 | 9.1 | 2 | 3.3 |
| 31-40 | 10 | 20.4 | 2 | 18.2 | 12 | 20 |
| 41-50 | 7 | 14.3 | 1 | 9.1 | 8 | 13.3 |
| 51-60 | 14 | 28.6 | 3 | 27.3 | 17 | 28.3 |
| >60 | 15 | 30.6 | 2 | 18.2 | 17 | 28.3 |
| Total | 49 | 0 | 11 | 100 | 60 | 100 |
| Mean ± SD | 52.27±17.1 | 42.18±16.71 | 50.42±17.31 | |||
Table 1: Age and gender distribution of necrotizing fasciitis.
| Occupation | Number of patients | % |
|---|---|---|
| Farmer | 17 | 28.3 |
| Housewife | 10 | 16.7 |
| Unskilled | 12 | 20 |
| Service | 9 | 15 |
| Skilled | 10 | 16.7 |
| Not applicable | 2 | 3.3 |
| Total | 60 | 100 |
Table 2: Occupation of patients.
Lower limb was the most common site involved in 32 (53.3%) patients followed by the perineum in 18 (30%) patients and trunk in 5 (8.3%) patients. (Table 3)
| Site | Number of Patients | % | 95%CI |
|---|---|---|---|
| Lower limb | 32 | 53.3 | 40.89-65.37 |
| Perineum | 18 | 30 | 19.90-42.61 |
| Trunk | 5 | 8.3 | 3.61-18.07 |
| Upper limb | 4 | 6.7 | 2.62-15.93 |
| Anterior Abdominal wall | 1 | 1.7 | 0.3-8.96 |
| Total | 60 | 100 | - |
Table 3: Site.
Regarding symptoms, pain was present in most of the cases 57(95%). Fever and discharge was present in 37(61.7%) & 35(58.3%) respectively. Swelling in 27(45%) and blisters/skin vesicles in 11(18.3%) were also noted. (Table 4)
| Symptoms | Number of patients (n=60) | % | 955CI |
|---|---|---|---|
| Pain | 57 | 95 | 86.30-98.29 |
| Fever | 37 | 61.7 | 49.62-72.91 |
| Discharge | 35 | 58.3 | 45.73-69.94 |
| Swelling | 27 | 45 | 33.09-57.51 |
| Blisters/Skin Vesicles | 11 | 18.3 | 10.56-29.52 |
| Hyper pigmentation/Hard Texture of skin | 8 | 13.3 | 6.91-24.17 |
Table 4: Symptoms at presentation.
Thirty three patients (55%), presented within a week, 19(31.7%) in 2 weeks and 8(13.3%) beyond 2 weeks. Mean duration of symptoms was 10.08 ± 10.09 days (Table 5). Clinical signs of oedema and ulcer was present in 51(85%) & 46(76.7%) respectively (Table 6).
| Duration of Symptoms | Number of patients(n=60) | % |
|---|---|---|
| 1-7 days | 33 | 55 |
| 8-14 days | 19 | 31.7 |
| >14 days | 8 | 13.3 |
| Mean ± SD: 10.08±10.09 | ||
Table 5: Duration of symptoms.
| Signs | Number of patients (n=60) | % | 95%CI |
|---|---|---|---|
| Pallor | 6 | 10 | 3.61-18.07 |
| Oedema | 51 | 85 | 73.89-91.90 |
| Ulcer | 46 | 76.7 | 64.56-85.56 |
| Lymph Adenopathy | 11 | 18.3 | 10.56-29.92 |
Table 6: Signs.
Trauma was the most common etiological factors comprising of 18(30%) patients. No predisposing factor was present in 4(6.7%) patients. The diversification of etiological factors is mentioned in Table 7.
| Etiology | Number of patients(n=60) | % | 95%CI |
|---|---|---|---|
| Trauma | 18 | 30 | 19.90-42.61 |
| Alcoholism | 8 | 13.3 | 6.91-24.17 |
| Native drug allergy | 9 | 15 | 8.10-26.11 |
| RTA | 6 | 10 | 4.86-20.15 |
| Insect bite | 6 | 10 | 4.86-20.15 |
| Thorn prick | 4 | 6.7 | 2.62-15.93 |
| Post-surgery | 3 | 5 | 1.71-13.70 |
| Injection | 2 | 3.3 | 0.9-11.36 |
| Abrasion | 1 | 1.7 | 0.3-8.86 |
| Eczema | 1 | 1.7 | 0.30-8.86 |
| Episiotomy sepsis | 1 | 1.7 | 0.30-8.86 |
| Septic abortion | 1 | 1.7 | 0.30-8.86 |
| IR Rays | 1 | 1.7 | 0.30-8.86 |
| Idiopathic | 4 | 6.7 | 2.62-15.93 |
Table 7: Etiology.
Diabetes mellitus was the most common associate comorbid condition comprising of 23(38.3%) patients, followed by hypertension in 18 patients (30%). Two of the patients in this study were HIV positive (Table 8).
| Associated Co morbid conditions | Number of patients(n=60) | % |
|---|---|---|
| 1.DM | 21 | 38.3 |
| 2.Hypertension | 18 | 30 |
| 3.Smoking | 11 | 18.3 |
| 4.CKD | 9 | 15 |
| 5.COPD | 8 | 13.3 |
| 6.CAD | 6 | 10 |
| 7.Cirrhosis | 3 | 5 |
| 8.HIV | 2 | 3.3 |
| 9.Tuberculosis | 2 | 3.3 |
| 10.Anemia | 1 | 1.7 |
| 11.Eczema | 1 | 1.7 |
| 12.Osteo arthritis | 1 | 1.7 |
| 13.Sepsis | 1 | 1.7 |
| 14.Idiopathic | 10 | 16.7 |
Table 8: Associated co morbid conditions.
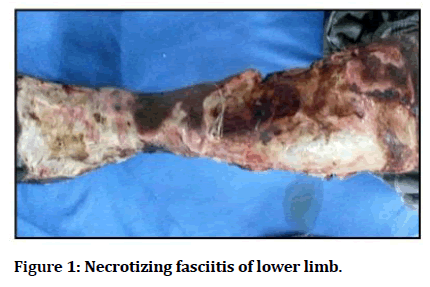
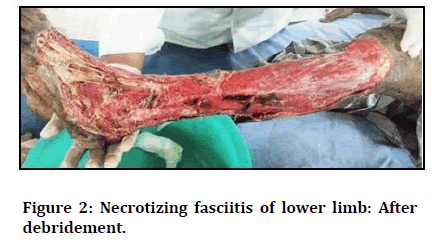
The laboratory parameters were evaluated. It was observed that 11(18.3%) patients had haemoglobin <10gm%, 18(30%) has RBS >180md/dl, 14(23.3%) had serum Creatinine >1.6mg/dl and 9(15%) with sodium levels <128mEq/l, which are all risk indicators as describes by a recently developed Laboratory Risk Indicator score for necrotizing fasciitis (LRINEC) (Table 9) (Figures 1 and 2).
| Blood Parameters | Number of patients (n=60) | % | 95 %CI |
|---|---|---|---|
| Hemoglobin gm% | |||
| <10 | 11 | 18.3 | 10.66-29.92 |
| >=10 | 49 | 81.7 | 70.08-89.44 |
| RBS mg/dl | |||
| <180 | 42 | 70 | 57.49-80.10 |
| >=180 | 18 | 30 | 19.90-42.51 |
| Serum Creatinine mg/dl | |||
| <1.6 | 46 | 76.7 | 64.56-85.66 |
| >=1.6 | 14 | 23.3 | 14.44-35.44 |
| Sodium mEq/L | |||
| <128 | 9 | 15 | 8.10-26.11 |
| >=128 | 51 | 85 | 73.89-91.90 |
Table 9: Laboratory investigations on admission.
Figure 1: Necrotizing fasciitis of lower limb.
Figure 2: Necrotizing fasciitis of lower limb: After debridement.
The culture was monomicrobial in 37 (61.7%) patients, polymicrobial in 22 (36.7%) patients and steri le in 1 (1.7%) patients.
Among this 52(86.7%) isolates were aerobic and 8(13.3%) were anaerobic (Table 10).
| Bacteriological Study | Number of patients(n=60) | % | 95%CI |
|---|---|---|---|
| Monomicrobial | 37 | 61.7 | 49.02-72.91 |
| Polymicrobial | 22 | 36.7 | 25.62-49.32 |
| Sterile | 1 | 1.7 | 0.3-8.86 |
| Aerobic | 52 | 86.7 | 75.83-93.09 |
| Anaerobic | 8 | 13.3 | 6.91-24.17 |
Table 10: Bacteriological study.
The commonest bacteria isolated were E.coli in 21(35%) patients followed by P. Aeruginosa in 14(23.3%) patients and L. Pneumoniae in 11(18.3%) patients.
Patients were initially given broad spectrum antibiotic combination with second or third generation cephalosporine+aminoglycosides+metronidazole followed by culture based antimicrobials.
Surgical treatment included debridement’s in 57(95%), Fasciotomy 3(5%), followed by Split skin grafting in 21(35%) and secondary suturing in 17(28.3%).
Statistical methods
Descriptive statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%). 95% Confidence Interval has been computed to find the significant features. Confidence Interval with lower limit more than 50% is associated with statistical significance.
Statistical software
The statistical software namely, SPSS 15.0, and R environment ver.2.11.1 were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables etc.
Discussion
Necrotizing fasciitis has been recognized for centuries dating back to Hippocrates in the 5th century BC. Necrotizing fasciitis was first described in 1871 by Confederate Army Surgeon Joseph Jones during the American civil was as 'hospital gangrene' and then by Meleney as 'haemolytic streptococcal gangrene'. In 1883, Fournier described a fulminating genital gangrene affecting healthy men, and named the process 'idiopathic gangrene of the scrotum'. In 1952, Wilson used the term Necrotizing fasciitis to describe the same disease in other parts of the body.
Necrotizing fasciitis is defined as a rapidly progressive tissue infection characterized by extensive necrosis of the subcutaneous fat and fascia. Secondary necrosis of the overlying skin is common, but the underlying muscles are mostly spared. The most frequent sites are the perineum and lower extremity, but any part of the body can be involved. Patients with necrotizing fasciitis present with local signs of infection and severe pain disproportionate to local findings. These may be associated with systemic toxic manifestations. Systemic manifestations such as hypotension, fever, tachycardia, Tachypnoea and laboratory findings of leukocytosis and metabolic acidosis are indices of development of sepsis.
Age and sex
Necrotizing fasciitis is commonly seen in middle age males. In our study 56% of the patients were >51 years and the male dominance was 81.7%. Male predominance is perhaps due to the increased incidence of trauma in males and increased outdoor activity. This is coinciding with the literature findings.
Etiology
Necrotizing fasciitis is known to follow minor trauma, insect bite, pustule or minor operations, anorectal abscess, instrumentation, septic abortion, genitourinary infection. In our study majority of the patients had a predisposing factor and majority (30%) was due to trauma. No etiological factor was present in 4(6.7%) patients. Primary or idiopathic. Necrotizing fasciitis occurs in the absence of a known or identifiable etiologic factor. The underlying pathogenesis of idiopathic Necrotizing fasciitis is still unknown. The etiology may be due to minor trauma and the trauma would have been so insignificant that the patient may have forgotten.
Site
In our study, lower limb (53.3%) and perineum (30%) was the commonest site involved. Other studies did not show similar results, perineum being the most common site. There may be a difference in the orunary site of infection due to a difference in the hygiene level. But other studies have shown the infection to be more common in the lower limbs, similar to our study.
Symptoms
Regarding symptoms, pain was present in most of the cases 57(95%). Fever and discharge was present in 37(61.7%) & 35(58.3%) respectively. Swelling in 27(45%) and blisters/skin vesicles in 11(18.3%) were also noted. Clinical signs of oedema and ulcer was present in 51(85%) & 46(76.7%) respectively. In their 14 year retrospective study of necrotizing fasciitis reported similar findings.
Co-morbid diseases
Diabetes mellitus was the most common co-morbid condition in our study (23%) which is co-relating with that in other literatures. Majority of the series reported diabetes mellitus as the most common co-morbid condition. Higher blood sugar in these patients produces a good medium foe bacterial growth and predisposes to an environment of low oxygen tension and rich substrate for bacterial growth. Diabetes also causes defective phagocytosis, decreased cellular immunity and micro vascular disease with resultant ischemia. Other comorbid factors associated with necrotizing fasciitis include chronic alcoholism, drug abuse, corticosteroid use, immune-suppression, AIDS, malignancy, chronic obstructive lung disease, chronic venous or lymph insufficiency, obesity, malnutrition, peripheral vascular diseases, tuberculosis and leprosy. In our series, other comorbid factors noted were: hypertension in 18 patients (30%), CKD in 9(15%), COPD in 8(13.3%), CAD in 6(10%), Cirrhosis in 3(5%), Tuberculosis in 2(3.3%). Two patients were HIV positive [11-19].
Conclusion
Necrotizing Fasciitis (NF) is a life threatening soft tissue infection, characterized by foudroyant spreading necrosis of the involved fascia’s. Every fascia in the body can be destroyed by this disease. Early diagnosis is critical to the survival of the patient and must rely on the clinical picture. The study was descriptive prospective study of Necrotizing Fasciitis. This study involved a single group of 60 patients with Necrotizing fasciitis admitted in Sree Balaji Medical College & Hospital, Chennai-44. Between the period of November 2014 and October 2016. The approval from the ethical committee was obtained to conduct the study.
The age ranged from 2 -81 years, the mean age being 50.42 ± 17.31 years. Maximum cases were above the age of 50 years. There were 49 males and 11 females, the male: female ratio being 4:45:1 Out if the 60 patients studied, 17(28.3%) were farmers by occupation.
Lower limb was the most common site involved in 32 (53.3%) patients followed by the perineum in 18 (30%) patients and trunk in 5 (8.3%) patients. Regarding symptoms, pain was present in most of the cases 57(95%). Fever and discharge was present in 37(61.7%) & 35(58.3%) respectively. Swelling in 27(45%) and blisters/skin vesicles in 11(18.3%) were also not ed.
Thirty three patients (55%), presented within a week, 19(31.7%) in 2 weeks and 8(13.3%) beyond 2 weeks. Mean duration of symptoms was 10.08 ± 10.09 days. Clinical signs of oedema and ulcer was present in 51(85%) & 46(76.7%) respectively. Trauma was the most common etiological factors comprising of 18(30%) patients. No predisposing factor was present in 4(6.7%) patients.
References
- Sarani B, Strong M, Pascual J, et al. Necrotizing fasciitis: Current concepts and review of the literature. J Am Coll Surg 2009; 208:279.
- Goldstein EJ, Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: Diagnosis and management. Clin Infect Dis 2007; 44:705-710.
- Anaya DA, McMahon K, Nathens AB, et al. Predictors of mortality and limb loss in necrotizing soft tissue infections. Arch Surg 2005; 140:151-157.
- Kobayashi L, Konstantinidis A, Shackelford S, et al. Necrotizing soft tissue infections: delayed surgical treatment is associated with increased number of surgical debridements and morbidity. J Trauma 2011; 71:1400-1405.
- McHenry CR, Piotrowski JJ, Petrinic D, et al. Determinants of mortality for necrotizing soft- tissue infections. Ann Surg 1995; 221:558 -63.
- Wong CH, Chang HC, Pasupathy S, et al. Necrotizing fasciitis: Clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am 2003; 85:1454-1460.
- Hsiao CT, Weng HH, Yuan YD, et al. Predictors of mortality in patients with necrotizing fasciitis. Am J Emerg Med 2008; 26:170.
- Secil M, Topacoglu H. Retroperitoneal necrotizing fasciitis secondary to colonic diverticulitis. J Emerg Med 2008; 34:95-97.
- Woodburn KR, Ramsay G, Gillespie G, et al. Retroperitoneal necrotizing fasciitis. Br J Surg 1992; 79:342-344.
- Amitai A, Sinert R. Necrotizing fasciitis as the clinical presentation of a retroperitoneal abscess. J Emerg Med 2008; 34:37-40.
- Frazee BW, Fee C, Lynn J, et al. Community-acquired necrotizing soft tissue infections: A review of 122 cases presenting to a single emergency department over 12 years. J Emerg Med 2008; 34:139 -146.
- Lille ST, Sato TT, Engrav LH, et al. Necrotizing soft tissue infections: obstacles in diagnosis. J Am Coll Surg 1996; 182:7.
- Yen ZS, Wang HP, Ma HM, et al. Ultrasonographic screening of clinically-suspected necrotizing fasciitis. Acad Emerg Med 2002; 9:1448-1451.
- Oelze L, Wu S, Carnell J. Emergency ultrasonography for the early diagnosis of necrotizing fasciitis: a case series from the ED. Am J Emerg Med 2013; 31:632.e5-7.
- Wong CH, Khin LW, Heng KS, et al. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: A tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med 2004; 32:1535-41.
- Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001; 345:1368-1377.
- Rybak MJ, Lomaestro BM, Rotschafer JC, et al. Vancomycin therapeutic guidelines: A summary of consensus recommendations from the infectious diseases Society of America, the American Society of Health-System Pharmacists, and the Society of Infectious Diseases Pharmacists. Clin Infect Dis 2009; 49:325-327.
- Talan DA, Moran GJ, Abrahamian FM. Severe sepsis and septic shock in the emergency department. Infect Dis Clin North Am 2008; 22:1-31.
- Lopez FA, Lartchenko S. Skin and soft tissue infections. Infect Dis Clin North Am 2006; 20:759-72.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Gopalsamy Santhanam Prabudoss*
1Department of General Surgery, Sree Balaji Medical College & Hospital Chromepet, Chennai, IndiaCitation: Gopalsamy Santhanam Prabudoss, Study of Medical and a Microbiological Study, J Res Med Dent Sci, 2022, 10(1):306-312
Received: 27-Dec-2021, Manuscript No. JRMDS-21-50904; , Pre QC No. JRMDS-21-50904 (PQ); Editor assigned: 29-Dec-2021, Pre QC No. JRMDS-21-50904 (PQ); Reviewed: 12-Jan-2022, QC No. JRMDS-21-50904; Revised: 17-Jan-2022, Manuscript No. JRMDS-21-50904 (R); Published: 24-Jan-2022