Research Article - (2022) Volume 10, Issue 10
Study of Etiology of Ophthalmoplegia in a Tertiary Care Hospital of Southern Odisha
Rajendra Kumar Behera and Deepak Choudhury*
*Correspondence: Deepak Choudhury, Department of Ophthalmology, MKCG Medical College, Berhampur, Odisha, India, Email:
Abstract
Aim: To study the etiology of ophthalmoplegia in a tertiary care hospital of southern Odisha.
Materials and methods: Prospective observational type of study. 50 patients having different grades of ophthalmoplegia attending out patients and inpatient department of Ophthalmology during the period from September 2019 to August 2021 of a tertiary eye care hospital of southern Odisha were included in this study. Each patient was examined thoroughly after taking detailed history. Detailed ophthalmological evaluation and detailed blood investigations was done. Radiological investigations were done whenever required.
Results: Highest incidence was found in the age group of 61-70 years i.e. 28%. Male to female ratio was 1.17:1. 98% of ophthalmoplegia showed unilateral involvement. 76% cases had single nerve affection. The most common nerve involved in present series was abducens nerve i.e. 40% followed by oculomotor nerve. Mydriasis was absent in 54% cases.
Conclusion: Most common cause of Ophthalmoplegia was vascular lesion, followed by craniofacial trauma. Abducent nerve involvement was more followed by oculomotor nerve.
Keywords
Ophthalmoplegia, Abducens nerve, Oculomotor nerve
Introduction
Ophthalmoplegia is paralysis or weakness of one or more of the ocular muscles [1]. It can be caused by neurological or myopathic disorders [2]. It may be internal or external, total or partial, pupil involving or sparing, painful or painless. Various causes are common ocular palsies (Occulomotor, Trochlear, Abducent nerve palsy), painful ophthalmoplegia (nasopharyngeal growth, tumour or aneurysm in cavernous sinus), Ophthalmoplegia caused by toxins or deficiency (Lead poisoning, Thiamine deficiency), Others (Progressive supranuclear palsy, thyroid disease, diabetes mellitus, brainstem tumours, migraine, basilar artery stroke, myasthenia gravis, muscular dystrophy, Fisher variant of Gullaine- Barresyndrome, MS) [3]. This study was conducted to find out the various etiologies of ophthalmolplegia in patients attending a tertiary care hospital of southern Odisha.
Materials and Methods
50 patients having different grades of ophthalmoplegia attending out patients and inpatient department of Ophthalmology during the period from September 2019 to August 2021 of a tertiary eye care hospital of southern Odisha were included in this study. Each patient was examined thoroughly. Detailed history was taken in each case giving importance to the present illness, mode of onset, duration, history of trauma preceding the symptoms, history of vomiting, fever, convulsion, giddiness, tinitus, chronic cough, history of symptoms suggestive of other cranial nerve involvement. In case of children, importance was given to birth history i.e. history of birth trauma, asphyxia. In case of females obstetrical and gynaecological history was taken. In past history, patients were asked about similar complaints in past. In personal history, patient was questioned regarding his habits, appetite, digestion, frequency of micturition. More importance was given to his addiction.
In general examination detailed examination was made, to look for any septic focus, lymphadenopathies, any abdominal masses, nutritional status of patient, conditions of heart and lungs. However, more importance was given for examination of central nervous system, examination of other cranial nerves, motor systems, sensory system, deep and superficial reflexes, gait and higher intellectual function was done to know whether there was any other neurological deficit. Blood pressure was recorded in every case.
Detailed ophthalmic examination was done in every case giving more importance to orthoptic examination and pupillary reactions in case of Oculomotor nerve palsies. The examination included:
• Vision recording was done for both near and distance, each eye separately with and without glasses and also with pin hole.
• Facial symmetry was evaluated. Any ptosis, proptosis, increased wrinkling on forehead in one side was noted.
• Anterior segment examination was done by slit lamp, with more importance to pupillary reaction. Both direct and consensual reaction was studied in both eyes. Pupillary reactions on near reflex were also examined. Corneal sensation was tested in both eyes.
• Cover test was done to know the type of squint and also to know primary and secondary deviations.
• Ocular movements were tested in cardinal positions of gaze. Restriction whether mild, moderate or gross in any particular direction was noted. Both uniocular and binocular eye movements were tested.
• Worth four-dot test: This test was done to know whether the patient has suppression of affected eye or has diplopia. If he has diplopia whether crossed or uncrossed.
• Diplopia charting: Diplopia is the most prominent symptom in case of acquired paralytic squint and useful guide in diagnosis.
• Visual fields: Perimetry was done using humphrey field analyser. In cases of oculomotor nerve palsy with ptosis fields were recorded in the affected eye after mechanically elevating the lids.
• Fundus examination: Fundus of both eyes was examined with direct ophthalmoscopy after dilating the pupils with 10% phenylephrine drops. Any pathological changes especially papilloedema, optic disc pallor were noted. At last retinoscopy was done in every case.
Routine investigations like Hb% estimation, total RBC. count, total WBC. count, differential count, ESR. were done with special stress on fasting blood sugar and urine sugar estimation to find out if the patient was diabetic. Montoux test and V.D.R.L. test were done to rule out tuberculosis and syphilis respectively. X-ray of Chestpostero- anterior view was taken to look for any pathology in lungs where ever it was felt necessary. CT was done to rule out brain tumor, stroke, aneurysm or multiple sclerosis. CSF study was done to diagnose multiple sclerosis, Kearns-Sayre syndrome. EMG (Electromyogram) was done where ever it was necessary.
Results
The present study was carried out in 50 patients of different types of ophthalmoplegia, screened out of 28,124 patients attending the department of Ophthalmology of a tertiary care hospital of south Odisha, from September 2019 to August 2021 for various eye problems. The incidence of ophthalmoplegia was observed to be 0.177% (Table 1).
| Age Group (years) | Numbers of patients | Percentage (%) | Sex | |
|---|---|---|---|---|
| Male | Female | |||
| 0-10 | 1 | 2 | 1 | 0 |
| Nov-20 | 2 | 4 | 1 | 1 |
| 21-30 | 7 | 14 | 3 | 4 |
| 31-40 | 10 | 20 | 8 | 2 |
| 41-50 | 5 | 10 | 3 | 2 |
| 51-60 | 4 | 8 | 3 | 1 |
| 61-70 | 14 | 28 | 5 | 9 |
| 71-80 | 5 | 10 | 2 | 3 |
| 81-90 | 2 | 4 | 1 | 1 |
| Total | 50 | 100 | 27 | 23 |
Table 1: Incidence of ophthalmplegia in relation to age and sex.
Highest incidence was found in the age group of 61-70 years i.e. 28% (14 cases). 54% cases were male. Male to female ratio was 1.17:1.
Our study showed that maximum number of 20 cases (40%) observed in upper class people, 30% cases in lower class. Rest of the cases i.e. 15 cases (30%) were distributed between upper middle, upper lower and lower middle class.
Out of 50 cases studied, 35 cases (70%) were from urban areas and 15 cases (30 %) were from the rural areas. It was observed that 49 cases (98%) of ophthalmoplegia showed unilateral involvement, whereas only one case had bilateral oculomotor nerve affection. Our study showed that maximum number of cases i.e. 38 cases (76%) had single nerve affection and only 12 cases (24%) had multiple nerve affection. The most common nerve involved in present series was abducent nerve i.e. 20 cases (40%). The Oculomotor nerve was the second most commonly involved nerve i.e. 18 cases (36%). No case of isolated Trochlear nerve palsy was reported in present series (Table 2).
| Causes of Ocular nerve palsy | Present Study | Percentage (%) |
|---|---|---|
| Idiopathic | 18 | 36 |
| Craniofacial trauma | 18 | 36 |
| Metabolic (DM) | 16 | 32 |
| Vascular (Hypertensive, Ischaemic) | 20 | 40 |
| Neoplasm | 8 | 16 |
| ORL disease | 8 | 16 |
| Meningitis | 4 | 8 |
| Congenital | 4 | 8 |
Table 2: Causes of ocular nerve palsies.
In the present study mydriasis was absent in 27 cases (54%). Moderate mydriasis is detected in 3 cases i.e. (6%) and complete mydriasis was present in 20 cases (40%). In the present series the distribution of mild, moderate and severe ptosis were 46%, 10% and 44%. Sixth cranial nerve (abducent) palsies were highest in number i.e. 20 cases (40%). Cranio-facial trauma was the most frequent cause of sixth nerve palsy.
Discussion
In our study highest incidence was found in the age group of 61-70 years i.e. 28% (14 cases). In this age group highest incidence might be occurred because of vascular origin. The second most common age group involved was 4th decade (20%). It might be due to more proneness of this age group to cranio-facial trauma. Higher incidence of ophthalmoplegia in people of upper socio-economic status (40%) might be due to higher risk of metabolic diseases like diabetes mellitus and hypertension that give rise to cerebrovascular accidents. This can also be attributed to the fact that economically higher groups are more conscious about their health problems leading to more hospital visits. 70% cases were from urban areas. Because of health consciousness more persons from the urban area attended the department in comparison to rural habitants. Moreover the higher incidence of diabetes, hypertension, and stress and strain seen in urban population may be the factors for increased incidence of ophthalmoplegia in the urban population. 98% cases were unilateral whereas only one case (2%) had bilateral oculomotor nerve involvement. Such higher incidence of unilaterality was also cited by Manon, et al. who reported 182 cases of unilateral involvement and only 15 cases of bilateral affection [4].
In our study 76% cases showed single nerve involvement, whereas 24% cases had multiple nerve affection. This high incidence of single nerve affection of 76% corresponds with the findings of Rucker 81.1% and 87.3%, Krishna, et al. 74.9%, Rama, et al. 65.5%, Rush, et al. 80%, Menon, et al. 82.7% and Jean-Claude, et al. 74.18% [4-10]. Table 3 shows involvement of various ocular nerves in our study and comparison with other studies.
| Ocularnerve | Rucker, 1958 | Rucker, 1966 | Krishna, 1973 | Rama, 1980 | Rosh, 1981 | Menon, 1983 | Jean –Claude, 2006 | Present study |
|---|---|---|---|---|---|---|---|---|
| Oculomotor | 33.50% | 27.40% | 33.30% | 31.10% | 29% | 32% | 35.48% | 36% |
| Trochlear | 6.70% | 8.40% | 0.50% | 1.10% | 17.20% | 6.10% | 0% | 0% |
| Abducent | 40.90% | 51.50% | 41.10% | 32.30% | 41.90% | 44.60% | 38.70% | 40% |
| Multiple | 18.90% | 12.70% | 25.10% | 35.50% | 11.90% | 17.30% | 25.82% | 24% |
Table 3: Comparion of cases with various ocular nerve involvements.
No case of isolated trochlear nerve palsy was reported in present series. However Rucker, Krishna, et al., Rama, et al., Rush, et al., Menon, et al. reported 6.7% and 8.4%, 0.5%, 1.1%, 17.2% and 6.1 % cases of isolated trochlear nerve palsy respectively [4-9]. Figure 1 shows a case of occulomotor nerve palsy. Figure 2 shows oculomotor nerve palsy following craniofacial trauma in a 9 year old child. Table 4 shows the comparison between various studies and present study with respect to causes of ocular nerve palsies.
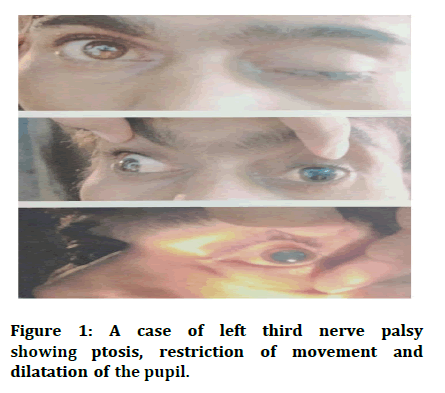
Figure 1: A case of left third nerve palsy showing ptosis, restriction of movement and dilatation of the pupil.
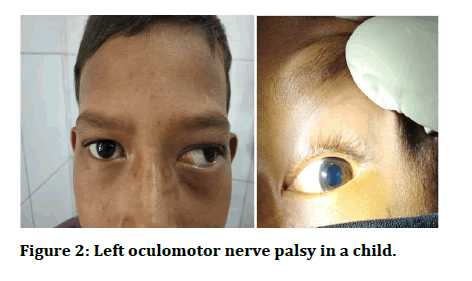
Figure 2: Left oculomotor nerve palsy in a child.
| Causes of Ocular nerve palsy | Rucker, 1958 | Rucker, 1966 | Krishna, 1973 | Rama, 1980 | Rosh, 1981 | Menon, 1983 | Jean-Claude, 2006 | Present Study |
|---|---|---|---|---|---|---|---|---|
| Idiopathic | 8.22% | 21.10% | 18.30% | 7.00% | 26.30% | 30.50% | 6.60% | 18% |
| Craniofacial trauma | 16.80% | 13.90% | - | - | 19.70% | 18.70% | 12.90% | 18% |
| Metabolic (DM) | - | - | - | - | - | - | 9.60% | 16% |
| Vascular (Hypertensive, Ischaemic) | 15.30% | 10.60% | 8.90% | 14.00% | 19.80% | 7.10% | 25.80% | 20% |
| Infective | - | - | 7.80% | 21.00% | - | 21.00% | - | - |
| Neoplasm | 16.50% | 26.30% | 9.50% | 18.00% | 14.30% | 12.00% | 9.60% | 8% |
| Pseudotumor orbit | - | - | - | - | - | 7.60% | - | - |
| ORL disease | - | - | - | - | - | - | 19.70% | 8% |
| Meningitis | - | - | - | - | - | - | 6.40% | 4% |
| HIV related | - | - | - | - | - | - | 9.60% | - |
| Congenital | - | - | - | - | - | - | - | 4% |
Table 4: Causes of ocular nerve palsies (comparison of previous report and present series).
The above Table 4 shows that vascular lesion was the most common cause of ophthalmoplegia (20%), which is nearly same as found by Rush, et al. i.e. 19.8% and relatively higher than other study groups like Rucker 15.3%, Rucker 10.6%, Krishna, et al. 8.9%, Rama, et al. 14% and Menon, et al. 7.1% [4-8]. But it is little lower than study of Jean-Claude, et al. i.e. 25.8 % [10]. The second highest group are idiopathic. ldiopathic cause is approximately same with study of Krishna, et al. i.e. 18.3 % [7].
Neoplasm caused 8% of all cases of paralysis including ocular motor nerves. However, the incidence was lower compared to study of Rucker 16.5%, Rucker 26.3%, Krishna, et al. 9.5%, Rama, et al. 18%, Rush, et al. 14.3%, Menon, et al. 12% and Jean-Claude, et al. 9.6% [4-10].
The exact nature of neoplasm could not be studied because maximum cases were referred to higher centres for investigation and further management. However, the provisional diagnosis was made on the basis of radiological evaluation.
In the present study mydriasis was not present in 34% cases, whereas in Jean Claude et al study it was higher 63.2% [10]. In the present series the distribution of ptosis with mild (46%), moderate (10%) and severe (44%) were nearly equal with the study of Jean-Claude, et al. i.e. 47.4%, 10.5% and 42.1% respectively. Sixth cranial nerve (abducent) palsies were highest in number i.e. 20 cases (40%) and the cranio-facial trauma was the most frequent cause of abducent nerve palsy. It might be due to thin, slender and longest intracranial course.
Conclusion
Most common cause of Ophthalmoplegia was vascular lesion, followed by craniofacial trauma. Abducent nerve involvement was more followed by oculomotor nerve. In spite of thorough clinical examinations and investigations, cause could not be determined in some of cases. However a detailed etiological work-up is necessary for management of these patients.
References
- Yu Wai Man CY, Smith T, Chinnery P, et al. Assessment of visual function in chronic progressive external ophthalmoplegia. Eye (Lond) 2006; 20:564-568.
- Elder D, Stewart W. Neuro-ophthalmology, in System of ophthalmology. Ed. Henry and Kimptom, London, 1972; 7:780.
- Chiba A, Kusunoki S, Obata H. Serum anti-GQ1b IgG antibody is associated with ophthalmoplegia in Miller Fisher syndrome and Guillain-Barre syndrome: clinical and immuno-histochemical studies. Neurol 1993; 43:1911–1917.
- Menon V, Singh J, Prakash P. Aetiological patterns of ocular motor nerve palsies. Indian J Ophthalmol 1984; 32:447-453.
- Rucker C. Paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol 1958; 46:787-794.
- Rucker C. The causes of paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol 1966; 61:1293-1298.
- Krishna A, Mehkri M. India Neurol 1973; 20:584.
- Rama V, Vimala J, Chandrasekhar M, et al. Ophthalmoplegia. Indian J Ophthalmol 1980; 28:13-16.
- Rush J, Young B. Paralysis of the cranial nerves 3,4,6: Cause and prognosis in 1000 cases. Arch Ophthalmol 1981; 99:76-79.
- Jean-Claude M, Georgette B, David L. Ocular motor nerve palsy. Indian J Ophthalmol 2006; 54:173-175.
Author Info
Rajendra Kumar Behera and Deepak Choudhury*
Department of Ophthalmology, MKCG Medical College, Berhampur, Odisha, IndiaCitation: Rajendra Kumar Behera, Deepak Choudhury, Study of Etiology of Ophthalmoplegia in a Tertiary Care Hospital of Southern Odisha, J Res Med Dent Sci, 2022, 10 (10): 215-219.
Received: 27-Jul-2022, Manuscript No. JRMDS-22-56987; , Pre QC No. JRMDS-22-56987(PQ); Editor assigned: 29-Jul-2022, Pre QC No. JRMDS-22-56987(PQ); Reviewed: 16-Aug-2022, QC No. JRMDS-22-56987; Revised: 27-Sep-2022, Manuscript No. JRMDS-22-56987(R); Published: 11-Oct-2022
