Research - (2021) Volume 9, Issue 6
Sensitivity Dictates Treatment Plan among Periodontists: Fact or Fiction Based on Patient Related Clinical Survey Following Periodontal Procedures
Siddharth Narayan* and ND Jayakumar
*Correspondence: Siddharth Narayan, Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, Tamil Nadu, India, Email:
Abstract
Background: Dentinal hypersensitivity is a unique complaint among the population which acts as a deterrent towards further treatment as well motivation towards the same. However most commonly it acts as a sign of some change in homeostasis of teeth and surrounding periodontium which requires attention. The fear of clinician induced postoperative sensitivity is also sometimes seen as a reason to alter the choice of treatment from an ideal to an alternative treatment plan. The present study aims to compare the postoperative dentinal hypersensitivity after scaling, root planning, kirkland flap and modified widman flap immediately after treatment and 10 days postoperatively. Methodology: The following study was conducted as a prospective single centre clinical trial in a Dental college and hospital-based setup. A total of Eighty patients were included from the department of Periodontology who were then divided into four groups of Twenty each based on treatment done including scaling (Group A), root planning (Group B), Kirkland flap surgery (Group C) and Modified Widman flap surgery (Group D). The 4 groups were matched based on age and gender and Oral hygiene status using OHI-S. A single operator sensitivity using a 10-point Visual analogue scale, Oral hygiene index simplified at baseline, immediately after treatment and 10 days after treatment. Sensitivity was assessed by using a triple way syringe using air flow along with water spray for 5 seconds after the drying the tooth using a dry cotton. Result: Net increase in sensitivity from baseline till 10 days postoperatively was seen in the root planning group>modified Widman group>scaling group>kirkland flap group, with increase in VAS score of 0.85, 0.45, 0.30 and 0.15 (p<0.05). Conclusion: Within the limits of this study, it was found that net increase in sensitivity was found to be maximal after root planning group, modified Widman flap surgery, scaling followed by kirkland flap surgery which was found to be clinically and statistically significant.
Keywords
Attachment loss, Sensitivity, Visual analogue scale, Periodontal therapy, Periodontal, postoperative.
Introduction
Dentinal hypersensitivity is a common complaint among individuals in university-based settings as well as private practice. It is also a strong motivator towards further dental treatment as the patient is unable to continue with his daily routine eliciting sharp shooting pain like sensation on intake of even water. As per the Canadian dental board it is defined as “pain derived from exposed dentin in response to chemical, thermal tactile or osmotic stimuli which cannot be explained as arising from any other dental defect or disease.” [1]. It is induced by multiple etiologies including non-surgical and postsurgical treatment of periodontal disease, gingival recession and tooth related wear facets (attrition, abrasion, erosion and abfraction) [2].
Dentinal hypersensitivity is caused by periodontal disease both as a direct result of destruction of periodontium along with the indirect effect seen as post therapeutic shrinkage of inflamed tissue. However few studies have tried to assess alterations in immediate and postoperative dentinal hypersensitivity compared to baseline values after non-surgical or surgical periodontal therapy.
The aim of the present study was to compare the postoperative dentinal hypersensitivity after scaling, root planning, kirkland flap and modified widman flap immediately after treatment and 10 days postoperatively.
Objective
The objective of the present study was to assess Visual analogue scale for dentinal hypersensitivity among patients maxillary and mandibular premolars immediately after and 10 days postoperatively after scaling, root planning, kirkland flap and modified widman flap surgery.
Methodology
The following study was conducted as a prospective single centre clinical trial in a Dental college and hospital-based setup. The study was initiated after approval from the institutional ethical review board and committee with ethical clearance number IHEC/SDCPERIO/ 1707/19/041. Patients included in the study were based on convenience sampling from the department of Periodontology in a Dental college and Hospital from 1st December 2019 till 1st January 2020. Written consent was obtained from all individuals taking part in this study after informing them about their entire treatment plan.
Inclusion criteria
All individuals included in the study were between the age groups of 25 to 60 years of age diagnosed as generalised chronic periodontitis (as per Armitage classification of periodontal disease 1999) with a clinical attachment loss equal to or more than 3mm in 33% teeth with dental arch comprising at least 24 teeth.. The teeth included in the study were standardized to Maxillary and mandibular premolars to obtain homogenous results.
Clinical attachment loss was defined as the deepest point of base of periodontal pocket till Cementoenamel junction at the mesio-buccal or disto-buccal line angle of the tooth. Probing pocket depth was defined as the deepest point of base of periodontal pocket till the free gingival margin at the mesio-buccal or disto-buccal line angle of the tooth. The simplified Oral hygiene index given by John C Greene and Jack R Vermillion in 1964 was also assessed.
Exclusion criteria
All individuals excluded from the study were based on (i) Pregnancy and lactating mothers (ii) Smokers (iii) Patients with uncontrolled systemic diseases (iv) Drug induced gingival enlargement (v) Patients under long term Non-steroidal anti-inflammatory drugs for the past 6 months for other ailments (vi) Teeth with dental caries, attrition, abfraction of tooth fracture (vii) Desquamative gingivitis or allergic dermatitis of unknown etiology.
Procedure
A total of Eighty patients were selected from the department of Periodontology which were then divided into four groups of Twenty each based on treatment done including scaling (Group A), root planning (Group B), Kirkland flap surgery (Group C) and Modified Widman flap surgery (Group D) randomly using a computergenerated table of numbers. Treatment done for all patients included phase 1 periodontal therapy including full mouth scaling (using universal tips and Woodpecker scaler units) with oral hygiene maintenance instructions followed by root planing separated using Gracey's Curettes (manufactured by Hu friedy instruments Pvt.) by a gap of 1 week under local anaesthesia (Lignocaine with 1:1,00,000 units adrenaline). Patients who required further periodontal therapy in the form of flap surgery received full thickness kirkland flap or modified Widman flap under adequate local anaesthesia based on clinical requirement. (Kirkland flap was performed for moderate pocket depth or aesthetic zone while modified Widman was performed in deep pockets where need for respective treatment modalities for altered bone morphology was felt or gingival enlargement despite Phase 1 therapy). All procedures were performed by the same operator (SN) under the guidance and supervision of the second author to standardize the level of care and clinical skill involved.
Only cases which required open flap debridement without the need for regenerative materials were included in the present study, black braided silk sutures were used to approximate the wound without any regenerative material like bone grafts or membranes or emdogain. A single operator assessed all clinical parameters of the study including preoperative sensitivity using a 10-point Visual analogue scale for all teeth of interest along with their Oral hygiene index simplified scores, respectively at baseline, immediately after treatment and 10 days after treatment. Sensitivity was assessed by using a triple way syringe using air flow along with water spray for 5 seconds after the drying the tooth using a dry cotton, sensitivity was scored and recorded using VAS 10-point scale.
Statistical analysis
All values obtained in the present study were analysed using SPSS version 23. (The Statistical Package for the Social Sciences (SPSS) after being developed by Norman H. Nie, Dale H. Bent, and C. Hadlai Hull) P value less than 0.05 was considered statistically significant. The highest VAS values were recorded per individual. No statistical significance was found in the association of age/gender/ OHI-S and treatment done using Chi Square test (p>0.05). Intergroup and intragroup statistical significance was assessed using Anova. There was no statistical significance between baseline sensitivity VAS values (p>0.05) however, post treatment VAS values and 10 days postoperative VAS values were found to be statistically significant (p<0.05).
Results
A total of eighty patients were included in the present study with 40 males and 40 females’ patients involving 320 teeth. Each group of 20 individuals had 10 males and 10 females with a mean age ranging from 32 to 55 years respectively. OHI-S status was also recorded at the first appointment before initiation of any treatment which was between the range of 1.50 to 2.85, respectively. Teeth with maximal dentinal hypersensitivity was found to be mandibular premolars followed by maxillary premolar.
Visual analogue scale recorded showed maximal increase in sensitivity immediately after the procedure was found to be among the scaling group and modified Widman flap group with a mean reduction of 1.20 and 1.10. On the other hand, it was also found that 10 days postoperatively there was a reduction in sensitivity while comparing the scaling group with a difference of VAS of about 0.90 and 0.50 in the modified Widman group.
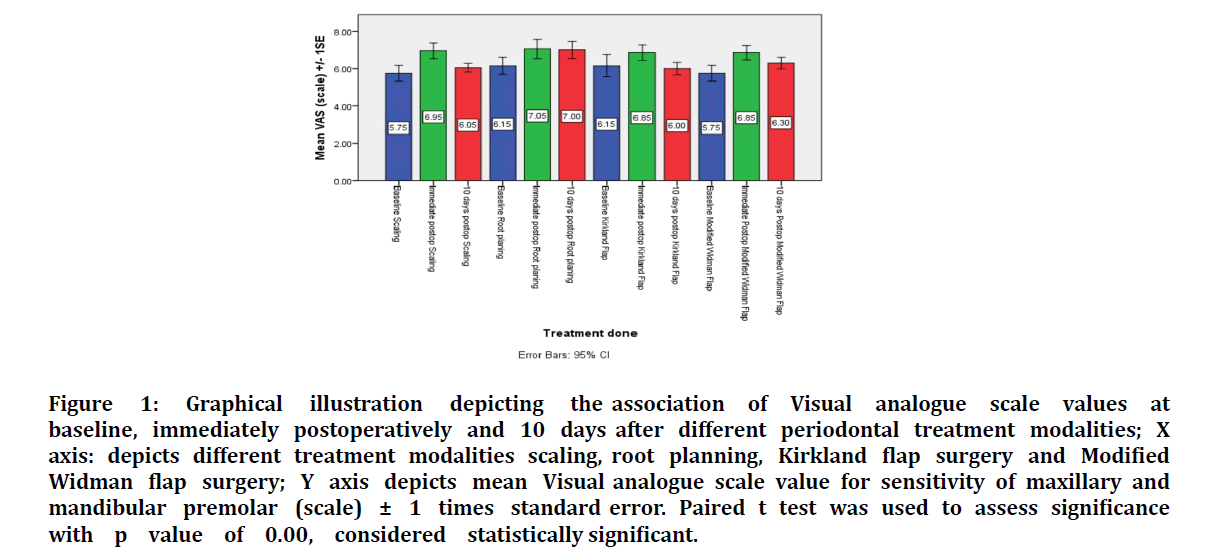
However net increase in sensitivity from baseline till 10 days postoperatively was seen in the root planning groupmodified Widman group>scaling group>kirkland flap group (Table 1 and Table 2), (Figure 1).
Figure 1: Graphical illustration depicting the association of Visual analogue scale values at baseline, immediately postoperatively and 10 days after different periodontal treatment modalities; X axis: depicts different treatment modalities scaling, root planning, Kirkland flap surgery and Modified Widman flap surgery; Y axis depicts mean Visual analogue scale value for sensitivity of maxillary and mandibular premolar (scale) ± 1 times standard error. Paired t test was used to assess significance with p value of 0.00, considered statistically significant.
| Features | Group A | Group B | Group C | Group D |
|---|---|---|---|---|
| (Mean ± Std. dev) | (Mean ± Std. dev) | (Mean ± Std. dev) | (Mean ± Std. dev) | |
| Number (n) | 20 | 20 | 20 | 20 |
| Age (years) | 41.5 ± 14.05 | 40.23 ± 14.28 | 39.38 ± 13.55 | 40.7 ± 14.3 |
| Gender (Male, Female) | 10 M 10 F | 10 M 10 F | 10 M 10 F | 10 M 10 F |
| OHI Scale | 2.21 ± 0.58 | 2.16 ± 0.58 | 2.30 ± 0.57 | 2.21 ± 0.56 |
| Baseline VAS | 5.75 | 6.15 | 6.15 | 5.75 |
| Immediate postoperative VAS | 6.95 | 7.05 | 6.85 | 6.85 |
| 10 days after VAS | 6.05 | 7 | 6 | 6.3 |
Table 1: Illustrates demographic data of age, gender, OHI-S matched Group A,B,C and D with their VAS scores at baseline, immediately postoperative and 10 days postoperatively; Treatment done Group A scaling, Group B root planning, Group C Kirkland flap, Group D Modified Widman flap.
| Dependent Variables | Mean Difference (I-J) | Standard Error | Significance (p value) | 95% confidence interval | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| VAS baseline score | 1.00* | ||||
| VAS Immediately after procedure Scaling (i) | |||||
| Root planing (j) | -1.3 | 0.294 | 0 | -2.09 | -0.5 |
| Kirkland flap (j) | -1.1 | 0.294 | 0.002 | -1.89 | -0.3 |
| Modified Widman flap(j) | -1.1 | 0.294 | 0.002 | -1.89 | -0.3 |
| VAS 10 days postoperatively Root planing (i) | |||||
| Scaling(j) | 0.95 | 0.232 | 0.001 | 0.31 | 1.58 |
| Kirkland flap(j) | 1 | 0.232 | 0 | 0.36 | 1.63 |
| Modified Widman flap(i) Root planing(J) | -0.7 | 0.232 | 0.021 | -1.33 | 0.69 |
Table 2: Illustrates statistical significance Inter and Intragroup assessed using Anova using Bonferroni correction with a p value of 0.05 considered statistically significant. 1.00* was considered statistically insignificant.
Discussion
Dental hypersensitivity is one of the most frequently faced chief complaints in all dental clinics around the world with prevalence studies suggesting about 25–30 % of the adult population complaining of dentin hypersensitivity while 52.6% of the population in a dental hospital. This corresponds to one among every four patients complaining of sensitivity of various etiologies [3]. Furthermore, it seems to have a negative effect on an individual’s life, especially affecting dietary selection along with the maintenance of optimal oral hygiene.
The present study using standardised teeth of maxillary and mandibular premolars showed a net increase in sensitivity from baseline till 10 days postoperatively was seen in the root planning group > modified Widman group > scaling group > kirkland flap group, with increase in VAS of about 0.85, 0.45, 0.30 and 0.15. A possible explanation for these findings could be the means of mechanical removal of calculus and plaque where scaling is ultrasonic driven while root planing and flap surgery follow hand instrumentation. Studies comparing the effect of air polishing, ultrasonic driven scaling and hand instruments in preserving cementum found air driven polishing preserved the most cementum followed by ultrasonic driven scalers and whereas Hand curettes were the most effective instruments in removing root cementum to expose dentin [4]. Another possible explanation could be the root substance removal per stroke after various strokes, low forces root substance loss per stroke was found to be between 6.8 μ to 2.3 μ while high forces root substance loss per stroke during strokes was found to be 20.6 μ to 5.6 μ using an electron transducer [5]. Periodontal flaps provide visibility and accessibility to remove residual calculus more efficiently in deeper pockets, both in anterior and posterior teeth [6]. Scaling and root planning with flap was found to show better removal of calculus as compared to that seen after scaling and root planning alone [7,8].
The present study observes greater postoperative sensitivity among patients treated by root planing as compared to modified widman flap. Suggesting the use of Modified Widman flap as a routine periodontal procedure for pocket reduction and not just for surgical crown lengthening disproving the long-term fear of postoperative sensitivity as a complication of the same.
Among all teeth assessed for dental hypersensitivity incisors (25.7%) and premolars (31.3%) were found to be the highest in studies conducted across various parts of the world [9–11]. Studies in India found similar findings with 25% prevalence of dentine hypersensitivity because of periodontal attachment loss and recession seen more among the older group of 50-59 years accounting for 98% of patients [12,13]. These studies were kept in mind while selecting Maxillary and mandibular incisors and premolar as teeth of interest. Periodontal literature has suggested buccal plaque scores were lower than lingual plaque scores among a normal population acting as a sign of tooth brushing habits of patients with findings like right sided patients had improved brushing habits on the left side [14,15].
It is generally agreed that toothbrushing behaviour primarily influences buccal plaque, since most individuals spend little or none of the time of the brushing cycle on palatal or lingual aspects of teeth [16]. Studies done priorly with dentinal hypersensitivity among an Indian population showed maximal periodontal related (attachment loss, recession) complaint of sensitivity was among the age group of 50 to 59 years which were contrary to the findings of the present study with a mean age of all four groups as 39.38 to 41.5 years [12].
Demerits of the present study include the fact that dentinal sensitivity is patient based clinical finding and all scales used to assess the same are subjective based on included patients. The threshold of pain could not be standardised by conducting a crossover study design as patients also get used to the experience of sensitivity around subsequent appointments affecting the overall purpose of the study.
Conclusion
Within the limits of this study, it was found that net increase in sensitivity was found to be maximal after root planning group, modified Widman flap surgery, scaling followed by kirkland flap surgery which was found to be clinically and statistically significant. Periodontists should not neglect modified Widman flap as root planning was found to produce more sensitivity.
References
- Canadian Advisory Board on Dentin Hypersensitivity. Consensus-based recommendations for the diagnosis and management of dentin hypersensitivity. J Can Dent Assoc 2003; 69:221–226.
- Gillam D, Talioti E. The management of dentine hypersensitivity. Dentine Hypersensitivity 2015; 45–76.
- Splieth CH, Tachou A. Epidemiology of dentin hypersensitivity. Clin Oral Investig 2013; 17:S3–S8.
- Bozbay E, Dominici F, Gokbuget AY, et al. Preservation of root cementum: A comparative evaluation of power-driven versus hand instruments. Int J Dent Hyg 2018; 16:202–209.
- Zappa U, Smith B, Simona C, et al. Root substance removal by scaling and root planing. J Periodontol 1991; 62:750–754.
- Kepic TJ, O’Leary TJ, Kafrawy AH. Total calculus removal: An attainable objective? J Periodontol 1990; 61:16–20.
- Buchanan SA, Robertson PB. Calculus removal by scaling/root planing with and without surgical access. J Periodontol 1987; 58:159–63.
- Caffesse RG, Sweeney PL, Smith BA. Scaling and root planing with and without periodontal flap surgery. J Clin Periodontol 1986; 13:205–210.
- Cunha-Cruz J, Wataha JC, Heaton LJ, et al. The prevalence of dentin hypersensitivity in general dental practices in the northwest United States. J Am Dent Assoc 2013; 144:288–296.
- Clark D, Levin L. Tooth hypersensitivity treatment trends among dental professionals. Quintessence Int 2018; 49:147–151.
- Que K, Guo B, Jia Z, et al. A cross-sectional study: non-carious cervical lesions, cervical dentine hypersensitivity and related risk factors. J Oral Rehabil 2013; 40:24–32.
- Dhaliwal JS, Palwankar P, Khinda PK, et al. Prevalence of dentine hypersensitivity: A cross-sectional study in rural Punjabi Indians. J Indian Soc Periodontol 2012; 16:426–429.
- Rao KA, Thomas S, Kumar JK, et al. Prevalence of dentinal hypersensitivity and dental erosion among competitive swimmers, Kerala, India. Indian J Community Med 2019; 44:390–393.
- Addy M, Mostafa P, Newcombe RG. Dentine hypersensitivity: the distribution of recession, sensitivity and plaque. J Dent 1987; 15:242–248.
- Arno A, Waerhaug J, Lovdal A, et al. Incidence of gingivitis as related to sex, occupation, tobacco consumption, toothbrushing, and age. Oral Surg Oral Med Oral Pathol 1958; 11:587–595.
- Macgregor IDM, Rugg-Gunn AJ. Toothbrushing duration in 60 uninstructed young adults. Community Dent Oral Epidemiol 1985; 14:121–122.
Author Info
Siddharth Narayan* and ND Jayakumar
Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, Tamil Nadu, IndiaCitation: Siddharth Narayan, ND Jayakumar,Sensitivity Dictates Treatment Plan among Periodontists: Fact or Fiction Based on Patient Related Clinical Survey Following Periodontal Procedures, J Res Med Dent Sci, 2021, 9(6): 1-6
Received: 03-May-2021 Accepted: 09-Jun-2021 Published: 17-Jun-2021