Research - (2022) Volume 10, Issue 1
Segmental Neurofibromatosis with Angioedema on the Same Side of Face: Report of an Interesting Case
Shikhar Ganjoo1*, MPS Sawhney1, Uma Sharma2 and Tulika Gupta3
*Correspondence: Shikhar Ganjoo, Department of Dermatology & STD, Shree Guru Gobind Singh Tricentenary Medical College and Hospital, Gurugram, India, Email:
Abstract
Neurofibromatosis (NF) is a genetic disorder arising from neural crest derived cells. Riccardi suggested a classification for NF dividing it into eight subtypes with segmental neurofibromatosis (SNF) being type 5. SNF is characterized by neurofibromas, café-au-lait macules (CALM) or only neurofibromas distributed in a particular segment of the body. We describe one patient who showed segmental expression of the disease along with angioedema on the same side of face. Cutaneous neurofibromas arise from small peripheral nerves and are composed of Schwann cells, fibroblasts, degranulation mast cells, and vascular cells. Increased number of mast cells in neurofibromatosis may be responsible for pruritus. Such patients may also have localized angioedema due to degranulation of this increased number of mast cells.
Keywords
Neurofibromatosis, Angioedema
Introduction
Neurofibromatosis (NF) is a genodermatosis arising from neural crest derived cells. They tend to develop from peripheral nerves and their supporting structures, including neurolemmal cells. Segmental neurofibromatosis is characterized by neurofibromas, cafe-au-lait macules (CALM) or only neurofibromas distributed in a particular segment of the body. The term “mosaic localized NF1” has been proposed to define this condition [1].
Crowe et al. [2] first reported about segmental neurofibromatosis but termed it as “sectorial neurofibromatosis” which was later renamed as segmental neurofibromatosis (SNF) by Miller et al. [3]. Later Riccardi proposed a classification for neurofibromatosis in which the disease was classified into eight variants with SNF being type 5 [4].
We describe one patient who showed segmental expression of the disease along with angioedema on the same side of face.
Case Report
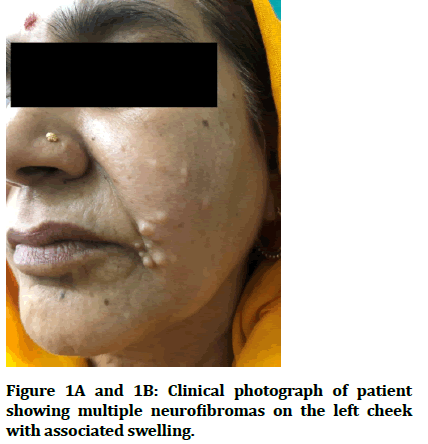
A 48-year-old female presented with a history of multiple small skin coloured nodules, on the left side of cheek. Initially a single nodule of about the size of a pea appeared on her left cheek 15 years back and progressively increased in size and number. The patient also had a peculiar history of angioedema on the left side of face, occurring everyday on waking up in the morning and spontaneously regressing in a few hours. She did not seek any investigations or treatment for the same. She had no family history of neurofibromatosis and no history of any neurological or ocular involvement.
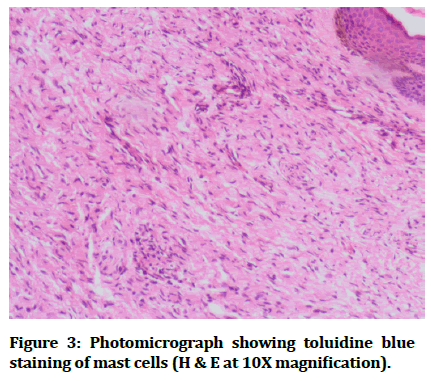
Physical examination revealed 12 soft to firm skin coloured nodules ranging from 0.5 to 1 cm diameter on the left side of cheek 1 cm lateral to angle of mouth (Figure 1a, 1b). On thorough examination we noted there were no axillary freckling, cafe-au-lait spots, or neurofibromas on any other part of the body. Slit lamp examination was done to rule out Lisch nodules. Routine haematological and biochemical investigations were within normal limits. Histopathological examination was suggestive of neurofibromas and revealed a nodule of delicate, wavy fibrils of nerve cells with elongated fibroblasts. The stroma showed myxoid change and epidermis was irregular (Figure 2). Toluidine blue stain was done showing increased number of mast cells (Figure 3).
Figure 1A and 1B: Clinical photograph of patient showing multiple neurofibromas on the left cheek with associated swelling.
Figure 2: Photomicrograph showing wavy, buckled nuclei of Schwann cells. (H&E at 10X magnification).
Figure 3: Photomicrograph showing toluidine blue staining of mast cells (H & E at 10X magnification).
Discussion
The above described case showed localized manifestations of neurofibromatosis (NF) limited to a circumscribed region of the body and not crossing midline. She also had history of angioedema on the same side of her face occurring on waking up in the morning which would spontaneously regress within a few hours. Hence, we believe that it is a case of segmental neurofibromatosis along with increased mast cells expression.
Riccardi suggested a classification for NF dividing it into eight subtypes [4]. NF1 also known as von Recklinghausen disease is the most common subtype. NF-1 is inherited as an autosomal dominant disorder. The gene for NF-1 (neurofibromas) is located on chromosome 17 [5]. The diagnosis of NF-1 is mainly clinical, based upon agreed clinical criteria which require two or more of the following conditions to be fulfilled :Cafe-au-lait spots (six or more with the greatest dimension of 5-15mm), neurofibromas (two or more of any type or one plexiform neurofibromas), freckling (axillary or inguinal), optic gliomas, Lisch nodules, two or more bony lesions (sphenoid dysplasia and others), family history (a first-degree relative with the disease) [6].
NF2 is characterized by acoustic neuromas which are usually bilateral, as well as meningiomas, optic gliomas and other tumours of the nervous system. NF-V is segmental NF (SNF), defined by presence of cafe-au-lait spots and neurofibromas limited to a given region of the body which is usually unilateral. It is a rare disorder with a prevalence estimated between 0.0014 and 0.002% [7]. This condition arises as a result of postzygotic mutation of NF1 gene representing somatic mosaicism hence it is not inherited explaining a negative family history in such cases [8]. It usually does not have any systemic involvement.
Furthermore, Roth et al [9] proposed another sub classification for SNF dividing it into true segmental, localized with deep involvement, hereditary, and bilateral subtypes with our patient being a case of true segmental NF. Patients can be clinically categorized into four groups: (i) Those which have only pigmentary changes, (ii) Which have only neurofibromas, (iii) Which have both pigmentary changes and neurofibromas, and (iv) Which have isolated plexiform neurofibromas [10]. Most commonly, patients present with only neurofibromas as in our case.
Cutaneous neurofibromas arise from small peripheral nerves and are observed in greater than 95% of patients with NF1 these tumors are composed of Schwann cells, fibroblasts, degranulating mast cells, and vascular cells [11,12]. Riccardi postulated a pivotal role for mast cells and melanocytes in NF1 causing pruritus, pigmentation defects, and, potentially, neurofibroma formation [13]. Mature mast cells are normally found in the endoneurial, perineurial, and epineurial spaces of peripheral nerves [14]. et al postulated that neurofibromas contained relatively high concentrations of mast cells significantly greater than the concentrations in other neoplastic or reactive nerve sheath tumors [15].
On the basis of above the fact emphasizing presence of mast cells in neurofibromas we can explain the presence of angioedema in our patient on the same (left) side of face occurring on waking up in the morning. Exosomes are vesicles secreted by mast cells responsible for transfer of substances responsible for cancer growth [16]. Ras is significantly linked to exosome biogenesis [17]. Exosomes can promote tumour growth and can also be used to treat oncogenic driven cancers. Mast cells show a significant correlation to neurofibromatosis apart from contributing just to angioedema, it secretes chondroitin sulphate and nerve growth factor in which chondroitin sulphate binds with nerve growth factor and increases its half-life, responsible for tumour survival and proliferation. This was possibly due to degranulation of mast cells as a result of pressure against pillow as she sleeps on her left side.
There are very few case reports (less than 150) of SNF and to the best of our knowledge none with angioedema presenting along with SNF. Therefore, with our article we would like to emphasize the role and presence of mast cells in neurofibromas.
Conclusion
Presence of increased number of mast cells in neurofibromatosis responsible for pruritus in such cases, can also present with localized angioedema due to mast cell degranulation. In such cases mast cells are present in deeper dermis and can degranulate on pressure.
References
- https://accessmedicine.mhmedical.com/book.aspx?bookID=2570
- Crowe FW. A clinical, pathological and genetic study of multiple neurofibromatosis. Neurology 1974; 24:1144-51.
- Miller RM, Sparkes RS. Segmental neurofibromatosis. Arch Dermatol 1977; 113:837–8.
- Riccardi VM. Neurofibromatosis: Clinical heterogeneity. Curr Probl Cancer 1982; 7:1–34.
- Williams VC, Lucas J, Babcock MA, et al. Neurofibromatosis type 1 revisited. Pediatr 2009; 123:124-33.
- Rosser T. Neurocutaneous disorders. Continuum 2018; 24:96-129.
- Victor FC. Segmental neurofibromatosis. Dermatol Online J 2005; 11:20–1.
- Tinschert S, Naumann I, Stegmann E, et al. Segmental neurofibromatosis is caused by somatic mutation of the neurofibromatosis type 1 (NF1) gene. Eur J Hum Genet 2000; 8:455–99.
- Roth RR, Martines R, James WD. Segmental neurofibromatosis. Arch Dermatol 1987; 123:917-20.
- Friedman JM, Gutmann DH, MacCollin M, et al. Neurofibromatosis: phenotype, natural history, and pathogenesis. Johns Hopkins University Press 1999.
- Hirota S, Nomura S, Asada H, Ito A, et al. Possible involvement of c-kit receptor and its ligand in increase of mast cells in neurofibroma tissues. Arch Pathol Lab Med 1993; 117:996–999.
- Riccardi VM. Cutaneous manifestation of neurofibromatosis: cellular interaction, pigmentation, and mast cells. Birth Defects Orig Artic Ser 1981; 17:129–145.
- Bienenstock J, MacQueen G, Sestini P, et al. Mast cell/nerve interactions in vitro and in vivo. Am Rev Respir Dis 1991; 143:S55–S58.
- Johnson MD, Kamso-Pratt J, Federspiel CF, et al. Mast cell and lymphoreticular infiltrates in neurofibromas: comparison with nerve sheath tumors. Arch Pathol Lab Med 1989; 113:1263–1270.
- Skokos D, Botros HG, Demeure C, et al. Mast cell-derived exosomes induce phenotypic and functional maturation of dendritic cells and elicit specific immune responses in vivo. J Immunol 2003; 170:3037-45.
- Sexton RE, Mpilla G, Kim S, et al. Ras and exosome signalling. Semin Cancer Biol 2019; 54:131-7.
- Antonopoulos D, Tsilioni I, Balatsos NAA, et al. The mast cell neurofibromatosis connection. J Biol Regul Homeost Agents 2019; 33:657-9.
Indexed at, Google Scholar, CrossRef
Indexed at, Google Scholar, CrossRef
Indexed at, Google Scholar, CrossRef
Indexed at, Google Scholar, CrossRef
Indexed at, Google Scholar, CrossRef
Indexed at, Google Scholar, CrossRef
Indexed at, Google Scholar, CrossRef
Author Info
Shikhar Ganjoo1*, MPS Sawhney1, Uma Sharma2 and Tulika Gupta3
1Department of Dermatology & STD, Shree Guru Gobind Singh Tricentenary Medical College and Hospital, Gurugram, India2Department of Pathology, Shree Guru Gobind Singh Tricentenary Medical College and Hospital, Gurugram, India
3Department of Ophthalmology, Shree Guru Gobind Singh Tricentenary Medical College and Hospital, Gurugram, India
Citation: Shikhar Ganjoo, MPS Sawhney, Uma Sharma, Tulika Gupta, Segmental Neurofibromatosis with Angioedema on the Same Side of Face: Report of an Interesting Case , J Res Med Dent Sci, 2022, 10(1): 169-171
Received: 12-Dec-2021, Manuscript No. JRMDS-21-47259; , Pre QC No. JRMDS-21-47259 (PQ); Editor assigned: 14-Dec-2021, Pre QC No. JRMDS-21-47259 (PQ); Reviewed: 28-Dec-2021, QC No. JRMDS-21-47259; Revised: 03-Dec-2021, Manuscript No. JRMDS-21-47259 (R); Published: 07-Jan-2022