Research - (2022) Volume 10, Issue 4
Role of Steroid Injection in Prevention of Keloid Recurrence
*Correspondence: Shwetha Shashikumar, Department of ENT, Sree Balaji Medical College and Hospital, Shankar Nagar, Chromepet, Chennai, Tamil Nadu, India, Email:
Abstract
Keloid scars are a common cutaneous lesion encountered by surgeons. They differ from ordinary and hypertrophic scars in that they can expand beyond the boundaries of the initial scar. Because corticosteroids limit fibroblast proliferation and increase collagen degradation, they are thought to be effective in keloid treatment. Keloids are tough to deal with and have a high recurrence rate. It has been proven that surgical excision combined with intralesional steroid injection, specifically Triamcinolone acetonide, is efficacious. The goal of this study was to see how Triamcenaloneaceonide may be utilized to treat keloid scars, either alone or in combination.Keywords
Keloid scars, Triamcinolone acetonide, Intralesional steroid
Introduction
Keloids are nodular lesions that span over the injury site and are a type of pathological scar. They don't go regress on their own, and they keep evolving through time. The lack of control mechanisms that self-regulate cell proliferation and tissue repair causes the pathological wound-healing process that leads to keloid development [1,2]. Keloids can cause both visual and functional deformity, decreasing one's quality of life. Despite the fact that various treatment options have been reported in the literature, there has yet to be a universally viable cure. The most successful way is to inject corticosteroids into the lesion alone or in combination with other treatment strategies. Triamcinolone acetonide is the most often used intralesional corticosteroid (TAC). Figure 1 shows keloid present over the pinna.
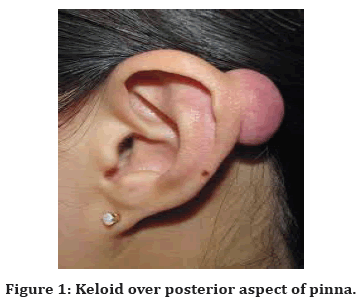
Figure 1. Keloid over posterior aspect of pinna.
The dark phototypes are highly prevalent. The most commonly affected body parts are the chest, elbows, earlobes, and upper back. Itching and discomfort are typical findings of the condition. Unlike hypertrophic wounds, keloids do not heal over time and frequently reoccur following excision. Large lesions can be disfiguring and functionally debilitating [3].
The aberrant wound-healing process that leads to keloid formation is caused by the breakdown of regulatory mechanisms that regulate cell proliferation and tissue repair. Keloids are identified by irregularly formed hyalinized collagen bundles and an advancing tip in the papillary dermis on histological examination [4]. A disruption in the normal equilibrium between ECM deposition and degradation found during wound healing, particularly during the remodeling phase, can influence keloid formation. The development and propagation of keloid scars has been associated to increased levels of cytokines such as tumour necrosis factor (TNF), interleukin (IL)-6, and IL-13, as well as growth factors such as vascular endothelial growth factor (VEGF) and transforming growth factor beta (TGF-B).Several ways of keloid treatment have been explored, but no uniform solution has yet been found. Inflammatory response alert, collagen metabolism alteration, and surgical and physical keloid scar manipulation are the three current clinical techniques [5].
Case History
We treated 10 cases of keloid. Patients presented to ENT OPD with history of swelling over the pinna of varying sizes, which progressively increased in size, not associated with any pain or discharge. Patients also gave history of a recent ear piercing that was done in the near past.
Size and extent of the keliod was assessed, in cases where the lesion was small, intra lesion Triamcenalone injection or combination of excision and intralesional injection was planned.
Necessary preoperative investigations were done and excision was done under local anaesthesia.
This was followed by 6 doses of intralesional Injection of Triamcenaloneacetonide was given. Preop and postop pictures are shown in Figure 2 and Figure 3.
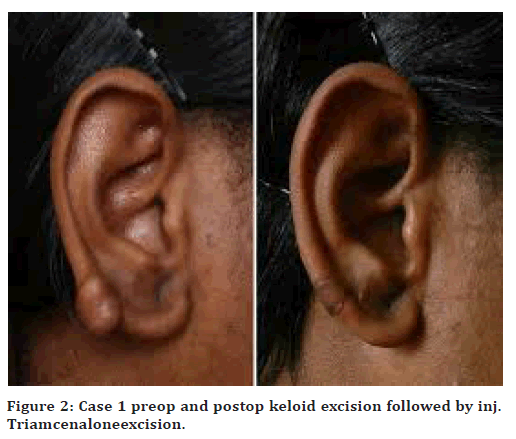
Figure 2. Case 1 preop and postop keloid excision followed by inj. Triamcenaloneexcision.
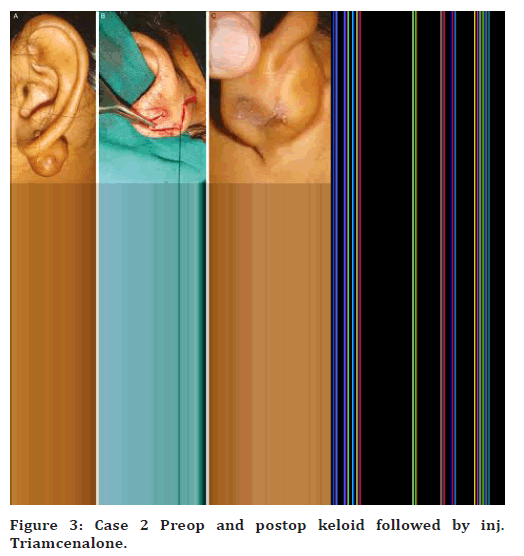
Figure 3. Case 2 Preop and postop keloid followed by inj. Triamcenalone.
Discussion
Keloids are aberrant wounds that appear as nodular hard lesions that extend beyond the point of injury. They don't regress on their own, and in fact, they can evolve through time. The lack of regulatory systems that regulate cell proliferation and tissue repair causes the pathological wound-healing process that leads to keloid development. Keloids have an advancing edge in the papillary dermis and hyalinized collagen bundles that are randomly organized [6]. The International Advisory Panel on Scar Management recommended intralesional steroid injections to prevent keloids and hypertrophic lesions. Through a variety of mechanisms, corticosteroids have been found to cause keloid regression [7]. They are strong vasoconstrictors, decreasing oxygen and nutrient availability to the wound bed, and hence reduce inflammation by inhibiting leukocyte and monocyte migration and phagocytosis Figure 4 and Figure 5.
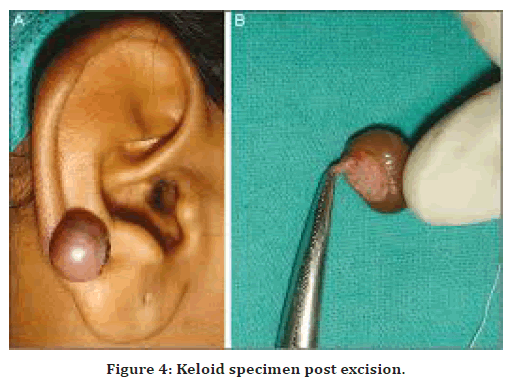
Figure 4. Keloid specimen post excision.
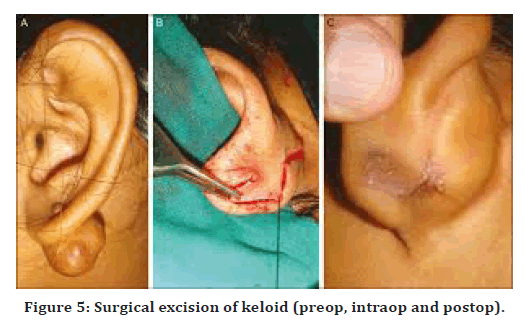
Figure 5. Surgical excision of keloid (preop, intraop and postop).
Amniotic effect inhibits keratinocytes and fibroblasts, delaying epithelialization and new collagen production.
Plasma protease inhibitors can be reduced, allowing collagenase to break down collagen.
TAC also lowers levels of alpha-1-antitrypsin and alpha-2-macroglobulin, which are typical collagenase regulators in human skin and appear to be higher in keloidal tissue.
Corticosteroids impair fibroblast proliferation and development, resulting in fibroblast degeneration. TGF B, insulin-like growth factor-1 (IGF-1), and hydroxyproline levels were also decreased in scar tissues treated with methylprednisolone. By interacting with glucocorticoid receptors, dexamethasone inhibited endogenous VEGF expression and fibroblast proliferation, producing keloid regression.
The most commonly used is Triamcenaloneacetonide amongst the many corticosteroids used for the treatment of keloiSmaller keloids were treated with 6 doses of intralesional Inj. Triamcenaloneacetonide, whereas bigger keloids were excised and treated with 6 doses of Inj. Triamcenaloneacetonide at the keloid site after 1 week of excision. All patients benefited, and only one out of ten patients had a keloid recurrence after steroid injection [8].
Complications
✓ Bleeding.
✓ Recurrence.
✓ Pain.
✓ Dehiscence.
✓ Infections.
✓ Chronic wounds.
✓ Severe pigmentation.
Conclusion
TAC intralesional injection, either alone or in combination with 5-FU, verapamil, and bleomycin, is the most common treatment for keloid scars, either before or after surgery. It's the gold standard for nonsurgical treatment of hypertrophic and keloid scars. It has been demonstrated to help reduce the size of keloid scars, as well as itching, pain, and discomfort, as well as prevent recurrence. Positive outcomes and patient satisfaction are frequently associated with combination therapy. Following surgical removal, triamcinolone helps to reduce keloid recurrence. It may also assist in the prevention of post-inflammatory hyper pigmentation.
References
- McCoy BJ, Diegelmann RF, Cohen IK. In vitro inhibition of cell growth, collagen synthesis, and prolyl hydroxylase activity by triamcinolone acetonide. Proc Soc Exp Biol Med 1980; 163:216–222.
- Ogawa R. The most current algorithms for the treatment and prevention of hypertrophic scars and keloids. Plast Reconstr Surg 2010; 125:557– 568.
- Brisset AE, Sherris DA. Scar contractures, hypertrophic scars, and keloids. Facial PlastSurg 2001; 17:263– 272.
- Sadeghinia A, Sadeghinia S. Comparison of the efficacy of intralesional triamcinolone acetonide and 5fluorouracil tattooing for the treatment of keloids. Dermatol Surg 2012; 38:104–109.
- Khan MA, Bashir MM, Khan FA. Intralesional triamcinolone alone and in combination with 5-fluorouracil for the treatment of keloid and hypertrophic scars. J Pak Med Assoc 2014; 64:1003–1007.
- Gupta S, Sharma VK. Standard guidelines of care: Keloids and hypertrophic scars. Indian J Dermatol Venereol Leprol 2011; 77:94–100.
- Dierickx C, Goldmann MP, Fitzpatrick RE. Laser treatment of erythematous/hypertrophic and pigmented scars in 26 patients. Plast Reconstr Surg 1995; 95:84–92.
- Norris JE. The effect of carbon dioxide laser surgery on the recurrence of keloids. Plast Reconstr Surg 1991; 87:44-53.
Indexed at, Google Scholar, Cross ref
Indexed at, Google Scholar, Cross ref
Indexed at, Google Scholar, Cross ref
Indexed at, Google Scholar, Cross ref
Indexed at, Google Scholar, Cross ref
Indexed at, Google Scholar, Cross ref
Author Info
1Department of ENT, Sree Balaji Medical College and Hospital, Shankar Nagar, Chromepet, Chennai, Tamil Nadu, India
Citation: MK Rajasekar, Shwetha Shashikumar, Role of Steroid Injection in Prevention of Keloid Recurrence, J Res Med Dent Sci, 2022, 10 (4):63-66.
Received: 30-Mar-2022, Manuscript No. JRMDS-22-58989; , Pre QC No. JRMDS-22-58989 (PQ); Editor assigned: 01-Apr-2022, Pre QC No. JRMDS-22-58989 (PQ); Reviewed: 18-Apr-2022, QC No. JRMDS-22-58989; Revised: 21-Apr-2022, Manuscript No. JRMDS-22-58989(R); Published: 28-Apr-2022
