Research - (2020) Advances in Dental Surgery
Role of Salivary PH on the Prevalence of Periodontal Disease: A Cross Sectional Pilot Study
Ranjith Raj VPRB and Murugan Thamaraiselvan*
*Correspondence: Murugan Thamaraiselvan, Department of Periodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University Tamilnadu, India, Email:
Abstract
Periodontium comprises alveolar bone, cementum, periodontal ligament, and the gingiva which function as one single unit in anchoring the teeth. Dental caries and periodontal disease have been reported as the common causes for tooth loss. Periodontitis refers to the inflammation of the periodontium which is a disease multifactorial in nature. Apart from plaque many other factors could also contribute as risk factor for periodontitis. The aim of this study is to assess the association between salivary pH and periodontal disease. This study was designed a cross sectional pilot study conducted in the subjects who visited the university dental hospital. The subjects were categorized into 3 groups: Healthy gingiva, Gingivitis and Periodontitis based on the gingival and periodontal parameters like gingival index (GI), periodontal probing depth (PPD), clinical attachment loss (CAL). The mean salivary pH was found to be 6.24 ± 0.11 in periodontitis group, 6.58 ± 0.58 in gingivitis group and 7 ± 0.18 in healthy gingiva group. From the above results it shows that the salivary pH of periodontitis group is acidic when compared to gingivitis and healthy group however did not show statistical significant difference (P>0.05).Within the limits of this pilot study it can be concluded that change in salivary pH does not influence the periodontal health status. However further studies are required to confirm our results.
Keywords
Saliva, pH, Periodontitis, Chairside, Biomarker
Introduction
Periodontium comprises alveolar bone, cementum, periodontal ligament, and the gingiva which function as one single unit in anchoring the teeth [1]. Dental caries and periodontal disease have been reported as the most common causes for tooth loss [2-5]. Periodontitis refers to the inflammation of the periodontium which is multifactorial in nature [6], where plaque and calculus are considered the main etiological agents, along with many other contributing factors such as altered immunity, genetic susceptibility etc. [7,8]. Enormous number of studies have been reported in the past 3 decades and are still underway regarding the role of these contributing factors in the pathogenesis of periodontal diseases [9,10]. Many other factors could play a role as a contributing factor that has not been proved or studied yet, which if proved can be used as a biomarker that can identify the subjects at risk of disease at an early stage. Some of the biomarkers that have been widely researched for its association with periodontal diseases are Interleukin-1beta, prostaglandins E2, oxidative stress, Vitamin D, neutrophil functions etc. [11-14]. With a lot of accumulating evidence regarding the role of many other contributing factors other than plaque and calculus have resulted in a paradigm shift in the understanding of pathogenesis of periodontal disease from plaque hypothesis to ecological plaque hypothesis [15]. Marsh hypothesis (ecological plaque hypothesis) states that the ecological stress could result in an imbalance of the periodontal microflora which ultimately results in the enrichment of the disease-causing pathogen (Ecological plaque hypothesis) [16]. This is supported by a study done by [17] which reported that the increase in the levels of progesterone hormone in women during pregnancy may make the gingival tissue more susceptible to the pathogens causing periodontal diseases [17]. In this context, salivary pH being one of the main contributing factors of dental caries, its role in periodontal disease is not yet explored completely [18-20].
Previously we have worked on plenty of topics in the field of periodontology [21-32]. Based on the previous research experience, we designed this study with the aim to assess the association between salivary pH and periodontal disease.
Materials and Methods
Study design and study setting
This study was designed as a cross sectional pilot study conducted in the subjects who visited as outpatients in a university dental hospital. This cross-sectional Study was carried out after obtaining approval from the institutional ethical review board, Ethical approval number: IHEC/ SDC- UG-1535/19/169, the study was conducted in the month of January 2020. Based on the inclusion and exclusion criteria.
Inclusion criteria
The subjects were divided into 3 groups: Healthy gingiva, generalized chronic gingivitis and generalized chronic periodontitis.
Criteria for gingivitis: based on the gingival index, inflammation of the gingiva without loss of attachment.
Criteria for periodontitis: based on the loss of attachment with pocket depth greater than 5 mm in at least 30% of the sites in the oral cavity.
Exclusion criteria
Subjects with xerostomia.
Subjects with systemic conditions which affect the salivary functions.
Subjects with cancer.
Subjects with completely edentulous arches.
Subjects under medications which affects the salivary function.
Saliva sampling
The subjects were categorized into 3 groups: Healthy gingiva, Gingivitis and Periodontitis based on the gingival and periodontal parameters like gingival index (GI), periodontal probing depth (PPD), clinical attachment loss (CAL). The subjects were informed of the study protocol and guidelines for saliva collection. Subjects were asked to rinse their mouth with 50ml of drinking water for 30 seconds, after which they were instructed to spit in the rinsed water into a sample collection container given to them, the subjects were instructed to refrain from talking and were asked to tilt their head downwards to let the saliva flow freely into the container (Figure 1). The process lasted about 10-15 minutes until the required quantity of saliva was obtained. The pH of the saliva was immediately measured to prevent discrepancies.
Figure 1: Shows the 25 ml saliva sample collected in the container, prior to the pH measurement the subjects were asked to rinse their mouth with 50 ml drinking water and were then asked to spit it out to remove the superficial food debris in the oral cavity before the pH measurement. 25ml of saliva sample was required for the electrode tip to touch the salivary sample.
Salivary pH analysis
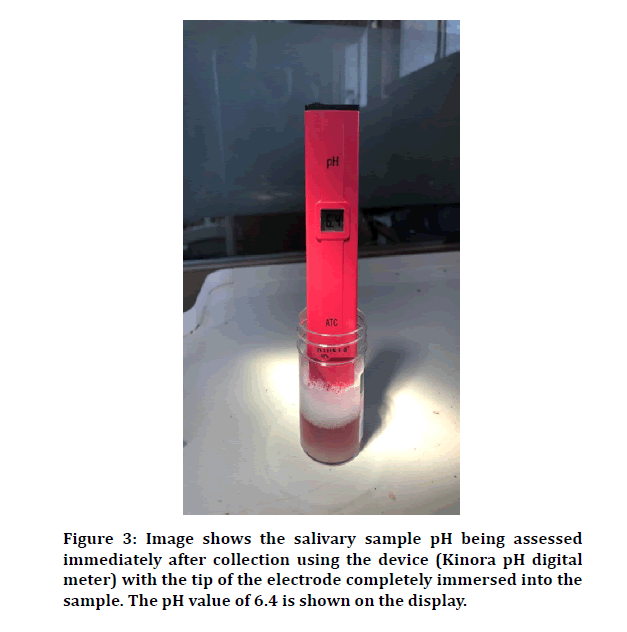
pH of the collected salivary samples was measured using Kinora Digital pH Meter as shown in Figure 2. The calibration of the digital pH meter was done everyday. The salivary pH meter was dipped inside the salivary sample to the level till which the electrode contacted with the saliva for about 10 seconds to get the actual reading (Figure 3). The reading was noted after which the electrode tip was disinfected and dried prior to the next measurement.
Figure 2: Shows the Pocket Digital pH meter (manufactured by KINORA). It has a range of 0.0 to 14.0 with an accuracy of + 0.1 pH and accuracy of ± 0.1pH. The device is calibrated before each use and was covered using protective cap after every use to prevent miscalibration.
Figure 3: Image shows the salivary sample pH being assessed immediately after collection using the device (Kinora pH digital meter) with the tip of the electrode completely immersed into the sample. The pH value of 6.4 is shown on the display.
Statistical analysis
Data obtained was exported to (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.) for further statistical analysis, With the obtained data frequency tests, descriptive tests and One-way ANOVA were done.
Results and Discussions
The present cross-sectional study assessed the salivary pH levels in 3 different groups of subjects based on the periodontal health status. Group 1: Healthy gingiva, Group 2: Gingivitis, Group 3: Periodontitis. Each group consisted of n=5. The mean salivary pH was found to be 6.24 ± 0.11 in periodontitis group, 6.58 ± 0.58 in gingivitis group and 7 ± 0.18 in healthy gingiva group (Table 1). From the above results it is shown that the salivary pH of periodontitis group is acidic when compared to gingivitis and healthy group. It could be because microbes survive better in an acidic environment making the oral cavity prone to plaque formation, caries formation and halitos which has been reported in few studies [33,34]. The more alkaline the salivary pH, the better the health status of the periodontium. However, the difference in salivary pH between groups did not reach statistical significance (p value>0.05). This could be due to the smaller sample size of n=5 of the study (Table 2).
| Study group | Salivary pH (Mean ± SD) | Range |
|---|---|---|
| Healthy Gingiva (n=5) | 7 ± 0.18 | 6.8 to 7.2 |
| Gingivitis (n=5) | 6.58 ± 0.58 | 6.5 to 6.7 |
| Periodontitis (n=5) | 6.24 ± 0.11 | 6.1 to 6.4 |
Table 1: Shows the mean salivary pH in healthy gingiva, gingivitis and periodontitis groups.
| Comparison between groups | P value |
|---|---|
| Group 1 vs Group 2 | 0.357 |
| Group 1 vs Group 3 | 0.192 |
| Group 2 vs Group 3 | 0.929 |
Table 2: Shows the comparison of mean salivary pH between the 3 groups (ANOVA test with Tukey’s correction).
However, the difference in salivary pH is considered clinically significant. In healthy conditions saliva aids in the maintenance of the oral environment. However, the pH of the saliva can be affected by various factors such as smoking habits, systemic conditions such as diabetes and the type of food consumed such as soft drinks and fruits [35-37]. This altered salivary pH may further have an impact on the periodontal health as reported in our study.
Use of serum and blood samples for investigation causes discomfort to the patient while saliva can be easily obtained with the patient's cooperation [38]. This proves that saliva can be used as an easy and valuable tool for chairside evaluation [39].
Our study had few limitations such as crosssectional study design, smaller sample sizes, less standardization. Hence further longitudinal studies, with larger sample size and standardized study design can confirm our study results and clear the doubt regarding whether the change salivary pH is the cause or result of periodontal disease.
Conclusion
Within the limits of this pilot study it can be concluded that change in salivary pH does not influence the periodontal health status. However further studies are required to confirm our results.
Acknowledgement
The authors would like to acknowledge the participants of the study.
Conflict of Interest
The authors declare no conflict of interest.
References
- Madukwe IU. Anatomy of the periodontium: A biological basis for radiographic evaluation of periradicular pathology. J Dent Oral Hygiene 2014; 6:70–76.
- Ong G, Yeo JF, Bhole S. A survey of reasons for extraction of permanent teeth in Singapore. Community Dent Oral Epidemiol 1996; 24:124–127.
- Gilbert GH, Miller MK, Duncan RP, et al. Tooth-specific and person-level predictors of 24-month tooth loss among older adults. Community Dent Oral Epidemiol 1999; 27:372–385.
- Bäumer A, El Sayed N, Kim TS, et al. Patient-related risk factors for tooth loss in aggressive periodontitis after active periodontal therapy. J Clin Periodontol 2011; 38:347–354.
- Nibali L, Farias BC, Vajgel A, et al. Tooth loss in aggressive periodontitis. J Dent Res 2013; 92:868–875.
- Ono T. Why and how do teeth come off? -New insights into the tooth loss during periodontitis-. Dent Oral Craniofac 2018; 4.
- Agrawal AA, Kapley A, Yeltiwar RK, et al. Assessment of single nucleotide polymorphism at IL-1A+ 4845 and IL-1B+ 3954 as genetic susceptibility test for chronic periodontitis in Maharashtrian ethnicity. J Periodontol 2006; 77:1515–1521.
- Knight ET, Liu J, Seymour GJ, et al. Risk factors that may modify the innate and adaptive immune responses in periodontal diseases. Periodontol 2016; 71:22–51.
- Kaarthikeyan G, Jayakumar ND, Padmalatha O, et al. Analysis of the association between interleukin-1β (+3954) gene polymorphism and chronic periodontitis in a sample of the south Indian population. Indian J Dent Res 2009; 20:37.
- Varghese S. Role of interleukin-1 in peri-implantitis. Drug Invention Today 2018; 10.
- Taba M, Kinney J, Kim AS, et al. Diagnostic biomarkers for oral and periodontal diseases. Dent Clin North Am 2005; 49:551–571.
- Amina M, Gayathri R, Priya VV. A detailed study on the function of neutrophils and macrophages in periodontitis. Drug Invention Today 2018; 10.
- Murthykumar K, Arjunkumar R, Jayaseelan VP. Association of vitamin D receptor gene polymorphism (rs10735810) and chronic periodontitis. J Investigative Clin Dent 2019; 10:12440.
- Ram AJ, Vishnupriya V, Ponnulakshmi R, et al. Estimation of salivary superoxide dismutase levels in chronic periodontitis patients with or without coronary heart disease. Drug Invention Today 2019; 12.
- Rosier BT, De Jager M, Zaura E, et al. Historical and contemporary hypotheses on the development of oral diseases: Are we there yet? Frontiers Cellular Infection Microbiol 2014; 4:92.
- Marsh PD. Microbial ecology of dental plaque and its significance in health and disease. Adv Dent Res 1994; 8:263–271.
- Lapp CA, Lapp DF. Analysis of interleukin–activated human gingival fibroblasts: modulation of chemokine responses by female hormones. J Periodontol 2005; 76:803-812.
- Galgut PN. The relevance of pH to gingivitis and periodontitis. J Int Academy Periodontol 2001; 3:61–67.
- Hans R, Thomas S, Garla B, et al. Effect of various sugary beverages on salivary pH, flow rate, and oral clearance rate amongst adults. Scientifica 2016; 2016.
- Sim CP, Soong YL, Pang EP, et al. Xerostomia, salivary characteristics and gland volumes following intensity-modulated radiotherapy for nasopharyngeal carcinoma: A two-year follow up. Australian Dent J 2018; 63:217–223.
- Ramesh A, Ravi S, Kaarthikeyan G. Comprehensive rehabilitation using dental implants in generalized aggressive periodontitis. J Indian Society Periodontol 2017; 21:160–163.
- Ravi S, Malaiappan S, Varghese S, et al. Additive effect of plasma rich in growth factors with guided tissue regeneration in treatment of intrabony defects in patients with chronic periodontitis: a split-mouth randomized controlled clinical trial. J Periodontol 2017; 88:839–845.
- Arjunkumar R. Nanomaterials for the management of periodontal diseases in Chaughule RS. Edn Dental Applications of Nanotechnology. Springer International Publishing 2018; 203–215.
- Gajendran PL, Parthasarathy H, Tadepalli A. Comparative evaluation of cathepsin K levels in gingival crevicular fluid among smoking and nonsmoking patients with chronic periodontitis. Indian J Dent Res 2018; 29:588–593.
- Jain M, Nazar N. Comparative Evaluation of the efficacy of intraligamentary and supraperiosteal injections in the extraction of maxillary teeth: A randomized controlled clinical trial. J Contemporary Dent Practice 2018; 19:1117–1121.
- Kavarthapu A, Thamaraiselvan M. Assessing the variation in course and position of inferior alveolar nerve among south Indian population: A cone beam computed tomographic study. Indian J Dent Res 2018; 29:405–409.
- Ramesh, A. et al. (2018) Comparative estimation of sulfiredoxin levels between chronic periodontitis and healthy patients-A case-control study. J Periodontol 2018; 89:1241–1248.
- Ramesh A, Vellayappan R, Ravi S, et al. Esthetic lip repositioning: A cosmetic approach for correction of gummy smile-A case series. J Indian Society Periodontol 2019; 23:290–294.
- Ezhilarasan D, Apoorva VS, Ashok Vardhan N. Syzygium cumini extract induced reactive oxygen species-mediated apoptosis in human oral squamous carcinoma cells. J Oral Pathol Med 2019; 48:115–121.
- Kaarthikeyan G, Jayakumar ND, Sivakumar D. Comparative Evaluation of bone formation between prf and blood clot alone as the sole sinus-filling material in maxillary sinus augmentation with the implant as a tent pole: A randomized split-mouth study. J Long-term Effects Med Implants 2019; 29:105–111.
- Kavarthapu A, Malaiappan S. Comparative evaluation of demineralized bone matrix and type II collagen membrane versus eggshell powder as a graft material and membrane in rat model. Indian J Dent Res 2019; 30:877–880.
- Vijayashree Priyadharsini J. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol 2019; 90:1441–1448.
- https://www.researchgate.net/profile/Madhvi_Gupta/publication/339017442_SALIVARY_pH_A_DIAGNOSTIC_BIOMARKER_OF_GINGIVITIS_AND_PERIODONTITIS_STATUS/links/5e39282792851c7f7f1a57ed/SALIVARY-pH-A-DIAGNOSTIC-BIOMARKER-OF-GINGIVITIS-AND-PERIODONTITIS-STATUS.
- Peterson S, Woodhead J, Crall J. Caries resistance in children with chronic renal failure: Plaque pH, salivary pH, and salivary composition. Pediatr Res 1985; 19:796–799.
- Kleinberg I, Hall G. pH and depth of gingival crevices in different areas of the mouths of fasting humans. J Periodont Res 1969; 4:109–117.
- Sánchez GA, De Preliasco MVF. Salivary pH changes during soft drinks consumption in children. International Journal of Paediatric Dentistry, pp. 2003; 13:251–257.
- Alghamdi SB, Togoo RA, Bahamdan GK, et al. Changes in salivary pH following consumption of different varieties of date fruits. J Taibah University Med Sci 2019; 14:246–251.
- Carolina DN, Rusyanti Y, Susanto A. Comparison of salivary alpha-amylase levels in gingivitis and periodontitis. Dent J 2017; 50:216-219.
- Nabi T, Singh S. Periodontal disease and salivary pH: Case control study. Int Archives Integrated Med 2019; 6:1–6.
Author Info
Ranjith Raj VPRB and Murugan Thamaraiselvan*
Department of Periodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University Tamilnadu, Chennai, IndiaCitation: Ranjith Raj VPRB, Murugan Thamaraiselvan, Role of Salivary PH on the Prevalence of Periodontal Disease: A Cross Sectional Pilot Study, J Res Med Dent Sci, 2020, 8 (7): 423-427.
Received: 21-Sep-2020 Accepted: 11-Nov-2020 Published: 18-Nov-2020