Review Article - (2022) Volume 10, Issue 8
Review on Impact of Diabetes Mellitus on COVID-19 Mortality and Severity
Shiv Joshi* and Shubhangi Shreysee
*Correspondence: Shiv Joshi, Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi (Meghe), Maharashtra, India, Email:
Abstract
COVID-19 Infection also called as coronavirus disease is a newly discovered surging viral illness which is caused due to severe acute respiratory syndrome coronavirus 2. Wuhan, China found its 1st case in December 2019. Since then, the disease has expanded across the world, which resulted into a pandemic that lead to the strain being kept on putting on global systems for health care across. Diabetes mellitus patients are a group that has been significantly affected by the epidemic. We performed a search on the online database PubMed to identify the relevant articles based on our eligibility criteria. There were a total of 18 papers, all of which identified the relation of diabetes mellitus with COVID-19 severity or mortality or both. Hence all of these studies were included. The aim of the research is to use this narrative review to summarise the data and evidence about Diabetes Mellitus and related COVID-19 mortality and severity.Keywords
COVID-19, Coronavirus, Diabetes mellitus, ACE-2, SARSIntroduction
Coronavirus disease 2019 (COVID-19) is a viral infection which is caused due to the severe acute respiratory syndrome corona virus 2 (SARS-CoV-2) [1]. COVID-19 was declared a public health emergency on January 30, 2020, by the World Health Organization (WHO) [2]. Despite the fact that a large number of individuals infected with COVID-19 have mild to no symptoms, some will progress to develop Acute Respiratory Distress Syndrome (ARDS), severe pneumonia, failure of multiple organs, and demise. SARS-CoV-2 infection can activate both innate and acquired immunological reactions, resulting in significant inflammatory reactions later in the illness. The uncontrolled and exacerbated inflammatory reactions can lead to both local and systemic tissue damage [3]. Decreased count of Eosinophils and decrease in number of lymphocytes with a substantial drop in the counts of B cells, CD8+, CD4+ T cells and natural killer cells are found in individuals with severe COVID-19 [4,5]. The occurrence of a cytokine storm, which is defined by increased serum levels of pro inflammatory cytokines, determines the severity of COVID-19 [6]. Furthermore, along with the viral RNA, IgA specific antibodies, IgG, and IgM antibodies against SARS-CoV-2 can be found in most individuals, laying the groundwork for tests that will help in patient diagnosis [7].
Diabetes Mellitus (DM) is an illness and a global wellbeing danger, the seriousness of which has expanded over the most recent two decades. Diabetes Mellitus affected 3 crore people in 1985, and by 2010, the amount had risen to 28.5 crores. According to the International Diabetes Federation's most recent global estimate, there are 46.3 crores of diabetes patients worldwide in 2019. Diabetes Mellitus is expected to affect around 70 crores people by 2045, according to projections. Diabetes Mellitus is the primary wellspring of kidney failure also called as end-stage renal disease, visual impairment, hearing impairment, neuropathy and non-horrendous lower limit removals. Diabetic complexities cause greater incapacity, and at the limit, dangerous issues [8]. The dysregulation of the Renin-Angiotensin-Aldosterone System [RAAS], the worsening inflammatory response, the hypercoagulability, and the physiological and underlying lung abnormalities induced by high blood glucose can all explain why diabetic people need to nurture extreme instances of COVID-19. In diabetic individuals, uncontrolled hyperglycaemia may induce glycosylation of Angiotensin-Converting Enzyme 2 [ACE 2], allowing SARS CoV-2 to enter the host [9]. COVID-19 is found to affect different individuals in different ways. Some patients with COVID-19 develop mild to moderate or sometimes remain asymptomatic and recover without hospitalization. The main prevalent signs and symptoms in patients suffering from COVID found were Pyrexia (79.5 percent), expectoration (25.0 percent), cough (61.8 percent), and Fatigue (31.4 percent). Initial symptoms in some individuals were dizziness, diarrhoea, and weariness. According to earlier studies, most common indicators of individuals suffering from COVID-19 were pyrexia (99%), non-productive cough (69%), myalgia (49%), and dyspnoea (42%). However, there was no discernible difference in clinical symptoms in diabetic versus non-diabetic subjects [10]. COVID-19 has shown unpredictable courses in various patients, hence, making it necessary for healthcare workers to be prepared for the various complications, differences in symptomatology, treatment modifications, outcomes and prognosis of their patients with special conditions. Diabetes mellitus, one of the most common chronic illnesses, is one such condition. Individuals with Diabetes Mellitus were found to be more prone to suffer from more severe and life-threatening COVID-19 after being infected with SARS-CoV-2 and the treatment outcome was much worse than in other patients.
Given that diabetes mellitus is one of the most prevalent co-morbidities in SARS patients, it is critical to define all elements of the relationship between these two disorders in order to equip the scientific and clinical communities with the tools they need to combat this epidemic as effectively as possible.
Literature Review
Methodology
Two authors (SS and SJ) individually researched and selected the studies using the following keywords and MeSH terms to search the PubMed database for papers written in English: “Covid”, “Diabetes”, “mortality″, “severity”, “(((covid[ti]) AND (diabetes[ti])) AND (mortality[ti])) and (severity[ti])”. The review was written following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
COVID-19 pathogenesis
COVID-19 virus belongs to corona virus family, characterised by a single stranded RNA which is encapsulated. The COVID-19 virus has been known to be having 4 genera consisting of alpha, beta, gamma, and delta. The former two genera are known to be infecting mammals, while the latter ones mainly infect birds. The virus outbreak of 2002 has been attributed to the SARS-Cov-1 virus, whose symptomatology resembles the current infection caused by SARS CoV-2. These symptoms are Acute Respiratory Distress, depletion of oxygen saturation and shortness of breath. The cause of similarity between the 2 viral strains can be attributed to their structural analogy, since both consist of envelope-anchored Spike S proteins, which is used by these viruses to anchor and enter their respective host cells. Studies have reported that SARS-CoV-1 and SARS-CoV-2 share 76% to 78% sequence resemblance, strongly suggesting both have the same access route into host cells that is ACE-2 (Angiotensin Converting enzyme 2).
The Ministry of Health and Family Welfare, Government of India has issued new guidelines dated 28 November 2021 for international travellers in context of reporting of a new variant of SARS-CoV-2 (B.1.1.529) named Omicron which has now classified as Variant of concern by the World Health Organization. This variant was first reported on November 24, 2021, in South Africa to World Health Organization. In South Africa, the epidemiological condition has been characterised by three different peaks in reported cases, the most recent of which was dominated by the Delta form. Infections have risen sharply in recent weeks, corresponding with the discovery of the B.1.1.529 strain. The first confirmed B.1.1.529 infection was discovered in a specimen taken on November 9, 2021. Furthermore, COVID-19 infection results in the elevation production of cytokines and chemokines that are responsible for inflammation such as interleukins IL-4, IL-10, and IL-1, Interferon (IFN), Monocyte Chemoattractant Protein 1 (MCP-1)and interferon gamma-instigated protein 10 (IGIP-10) (IP-10). Patients with severe illness admitted in the ICU had remarkably increased levels of plasma Interleukins like IL-6, IL-2, IL-7, IL-10, macrophage inflammatory protein-1A (MIP-1A), Granulocytes Colony Stimulating Factor (GCSF) and tumour necrosis factor alpha(TNF-α), suggesting a possible cytokine-storm that is then associated with increased severity and mortality of illness in COVID-19. Release of cytokines and chemokines that are responsible for inflammation attributes to high epithelial and endothelial cell death, as well as vascular leakage caused by rapid replication of virus. IL-1 and IL-6, among the supplied pro-inflammatory cytokines, are particularly compelling and appear to be highly associated with the development of COVID-19 infection in adult patients. Increased release of cytokines in the body appears to be a crucial factor in occurrence of fibrosis in Lungs and which is also linked to higher viral burden, respiratory failure, lung damage, and higher incidence of death rate [11].
Course of diabetes mellitus
India is capital of diabetes. The number of newly detected patients of type 2 Diabetes Mellitus is 40% that presents without complications. Out of total near about 25% of the patients presents with complications of diabetes due to discontinuation of anti-diabetic medication and faulty lifestyle. The remaining 35% of patients are undetected diabetes mellitus as they do not present in the healthcare system due to their decreased awareness regarding diabetes and its symptomatology. The major group which are at higher risk of getting diabetic complications secondary to diabetes comprises of 60% of the individuals who are at increased possibility of preponderant complications of diabetes including infections, sepsis, worsening of previous infective aetiology as compared to normal patients and hypercoagulable states.
In type 2 Diabetes Mellitus having uncontrolled sugar showed increased frequency of infections due to readily availability of glucose in extra cellular and intracellular compartments. Diabetes is said to further reduce the potency of immune system due to changes occurring in microvascular and macrovascular levels. Hence, leading the patients more susceptible and vulnerable to infections. Diabetes is further said to be most important cause of hyper coagulable state of blood of patient. Hypercoagulable state of the patient further exposes the patient to the diseases involving myocardial infarction, cerebrovascular episodes including strokes. This condition makes the patient moribund. And hence increasing the chances of secondary infections.
Hyperglycaemia in COVID-19
It has been observed that the Individuals who were suffering from Diabetes mellitus showed an increased severity of COVID sickness, for which SARS-COV-2 was accountable. Corona Virus disease also leads to hyperglycaemia in persons who have been exposed to it. The remarkable Hyperglycaemia which is found in COVID-19 individuals during their state of acute inflammation has been documented and it has been observed to be more evident in individuals who are pre-diabetic or have Obesity and/or Diabetes Mellitus. A two-way relation has already been discovered between chronic inflammation and hyperglycaemia as the complications of chronic Diabetes Mellitus. Multiple changes in the immune system are present in obesity and Diabetes Mellitus type 2, for example, including increase in the number of chemokines and cytokines, changes in the quantity and activation status of different leukocyte cells, and high rate of apoptosis and fibrosis, indicating that inflammation plays a major part in the aetiology of hyperglycaemia, progression of complications in chronic Diabetes Mellitus. This baseline inflammatory state, we believe, may prepare the way for greater levels of inflammatory cytokines, such as those described in COVID-19 and other acute infectious illnesses, as well as increased insulin resistance and consequences of inflammatory reactions of acute infections or stress [12].
Hyperglycaemia, when combined with other risk factors, might alter insusceptible and provocative reactions, putting patients at risk for catastrophic COVID-19 and potentially fatal outcomes. Angiotensin converting enzyme II (ACE II) is a main portion receptor for SARS COV 2, which is required for the Renin-Angiotensin-Aldosterone System (RAAS), while Dipeptidyl Peptidase IV (DPP IV) can also possibly be a limiting mark. When the CoV-2 protein associated with SARS attaches to the Angiotensin-Converting Enzyme II (ACE II) receptor, it invades the human cell [13]. The ACE II receptor is found in the renal epithelium, enterocytes, pancreas, lungs, heart, and endothelial cells, which also acts as an anti-inflammatory marker. After immunostaining, the high expression of the ACE II receptor in pancreatic endocrine and exocrine tissue suggests that this organ is also a potential target for Corona Virus 2. Pancreatic damage caused due to the virus's cytopathic action, can result in impaired metabolism of glucose, leading to hyperglycaemia and a bad prognosis in COVID-19 patients [14-16]. In COVID-19-infected patients, uncontrolled hyperglycaemia deteriorates the patients' condition and frequently results in a poor prognosis and death.
Discussion
In a study if was reported that the deadly infection also induces hyperglycaemia by disrupting fat cells and hence decreasing the production of adiponectin. Adiponectin is a fat-cell secreted protein hormone that plays a critical role in the prevention of insulin resistance, diabetes, and atherosclerosis. Adiponectin deficiency is believed to be a critical factor in the development of type 2 diabetes, obesity, and cardiovascular disease in humans. Further studies indicated that the COVID-19 ARDS patients had significant drops in adiponectin levels in their blood.
In any case, preliminary data suggest that glucose lowering DPP IV inhibitors have no discernible effect on SARS-CoV-2 predisposition. Because of their unique pharmacology, sodium glucose cotransporter II (SGLT II) inhibitors are not recommended in individuals with COVID-19 infection. Insulin should be the first line of defence in the fight against diabetes presently [17]. However, Doctors eventually discovered that COVID-19 is associated with hyperglycaemia in individuals who had no history of diabetes. Therefore, all medical practitioners must strive for adequate glycaemic control (Blood glucose 180 mg/dl) in all patients infected with COVID, whether or not they have diabetes.
The risk of diabetes mellitus in covid-19
COVID-19 positive diabetic individuals are more prone to have an abnormally hypercoagulable condition and uncontrolled inflammatory responses, which can lead to a poorer result [18,19]. It is evident that advanced age, the presence of diabetes mellitus, hypertension, and obesity (Body Mass Index greater than 40 kg/m2) are all associated with increased mortality in COVID-19 patients. As there is an increased incidence of Cardio Vascular Diseases (CVD), hypertension and Obesity among diabetic individuals, it is unclear if Diabetes Mellitus contributes to this increased risk on its own. In any event, Diabetes Mellitus are blood glucose levels are independent predictors of severity and death in SARS infected individuals.
- Reduced viral clearance from the body,
- Effective infection passage,
- Cytokine storm,
- Decreased count of T cell cells,
- Increased blood sugar levels,
- Increased vulnerability to hyper inflammation, and
- Presence of Cardiovascular Disorders is all the possible factors that could increase COVID-19 predisposition in individuals with Diabetes Mellitus [20-22].
A huge assemblage of proof has featured an expanded vulnerability of patients with Diabetes Mellitus to irresistible illnesses, which is potentially ascribed to an inadequate resistant framework in diabetes [23]. Pneumonia has lately emerged as a significant cause of fatality, owing to Diabetes Mellitus patients’ diminished resistance. Diabetes Mellitus and blood glucose levels were shown to be independently linked to increased severity and mortality in COVID-19 patients [24].
Various complications associated with diabetes mellitus and COVID-19
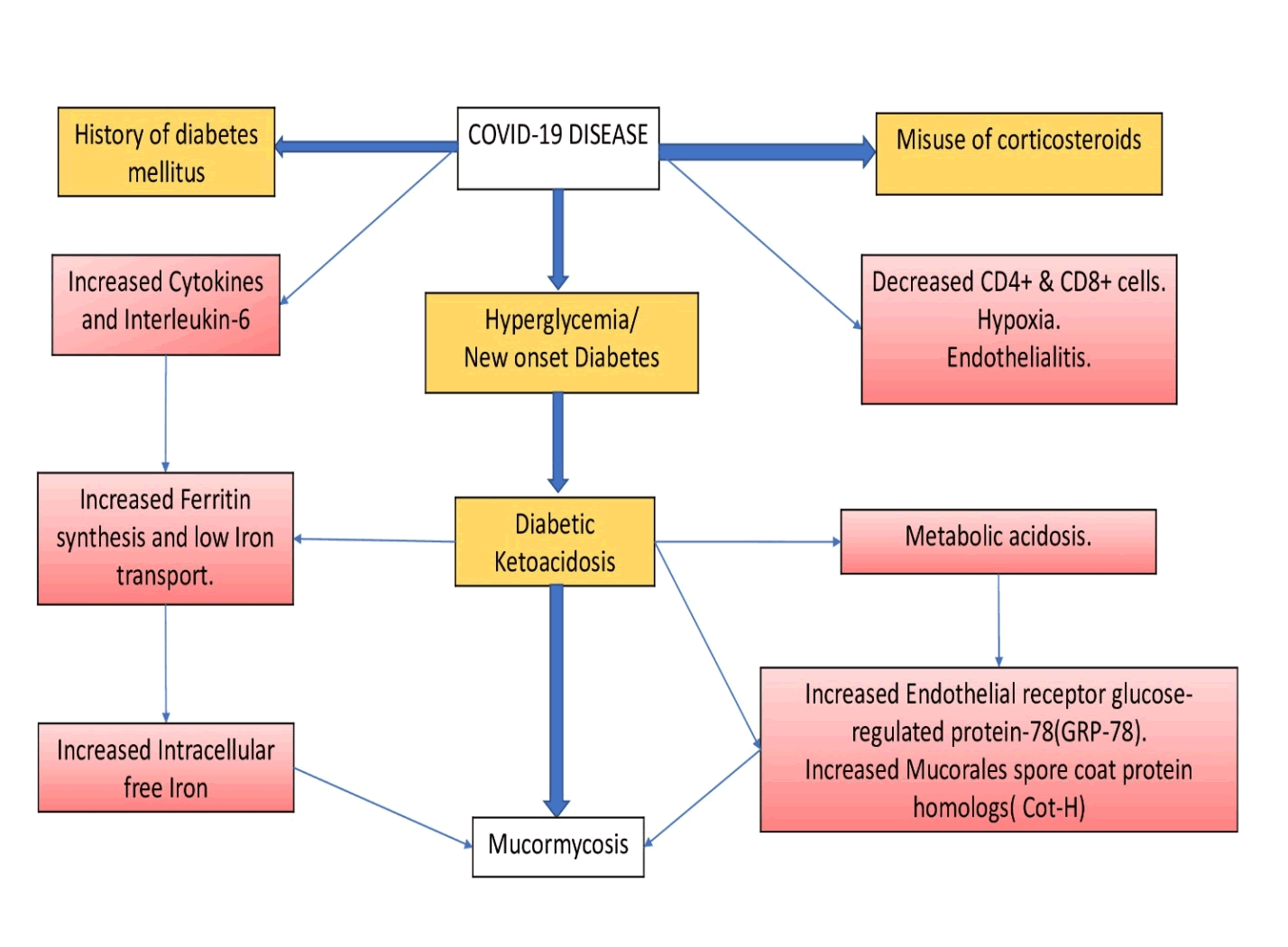
It has been noted that there has been an increase in the number of cases of rhino-orbital mucormycosis in persons with coronavirus disease 2019 (COVID-19), particularly in India. Diabetes is a separate risk factor for both severe COVID-19 and mucormycosis [25]. Diabetes (73.5 percent), malignancy (9.0 percent), excessive use of corticosteroids and organ transplantation are all risk factors for mucormycosis in Indians (7.7 percent) [26]. Uncontrolled hyperglycaemia consequently plays an important role in the susceptibility to Mucor mycosis. There are several triggers that lead to development of Mucormycosis as a complication in COVID-19 affected individuals like weakened cell mediated immunity by lowering CD4+ and CD8+ cell numbers, leads to increased susceptibility to this complication [27,28]. Moreover, Diabetes Mellitus, in conjunction with or in the absence of DKA, increases the risk of contracting mucormycosis. Apart from that overuse, misuse and rampant use of corticosteroids for the treatment of the same leads to immunosuppression. Patients however benefit greatly from free iron. Hyperglycaemia causes ferritin and transferrin to be glycosylated; reducing iron binding and allowing for freer iron [29]. Mucor development is aided by acidic PH, high sugar levels, more free iron and ketones due to which there is diminished WBC phagocytic activity (Figure 1) [30].
Figure 1: Mechanism of higher susceptibility to mucormycosis in individuals infected with COVID-19.
Due to the increased mortality, a higher index of suspicion is essential in high risk groups to guarantee quick diagnosis and proper treatment for improving the natural history of the devastating disease [31,32].
Conclusion
Diabetes mellitus has severe implications on COVID-19 mortality and severity. Individuals with Diabetes Mellitus Type 2 and raised levels of HBA1c when exposed to SARS-CoV-2 develop more complications. Hence, a robust management is required for the individual having COVID-19 with Diabetes Mellitus. If further examined, these discoveries could assist with developing appropriate interventions for individuals with Diabetes Mellitus who also tested positive for COVID-19. Therefore, there is a need to undertake further scientific studies to enhance our understanding of COVID-19, not only with respect to Diabetes but also other non-communicable diseases.
References
- Anka AU, Tahir MI, Abubakar SD, et al. Coronavirus disease 2019 (COVIDâ?19): an overview of the immunopathology, serological diagnosis and management. Scand J Immunol 2021; 93:12998.
- Chow N, Fleming-Dutra K, Gierke R, et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019–United States, February 12â??March 28, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:382-386.
- Felsenstein S, Herbert JA, McNamara PS, et al. COVID-19: Immunology and treatment options. Clin immunol 2020; 215:108448.
- Qin C, Ziwei MP, Tao SY, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China; Clinical Infectious Diseases; Oxford Academic. Clin Infect Dis 2020.
- Tan M, Liu Y, Zhou R, et al. Immunopathological characteristics of coronavirus disease 2019 cases in Guangzhou, China. Immunol 2020; 160:261-268.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. lancet 2020; 395:497-506.
- Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol 2020;20:269-270.
- Abdi A, Jalilian M, Sarbarzeh PA, et al. Diabetes and COVID-19: A systematic review on the current evidences. Diabetes Res Clin Pract 2020; 166:108347.
[Crossref] [Google Scholar] [Pubmed]
- Leon-Abarca JA, Portmann-Baracco A, Bryce-Alberti M, et al. Diabetes increases the risk of COVID-19 in an altitude dependent manner: An analysis of 1,280,806 Mexican patients. Plos one 2021; 16:0255144.
[Google Scholar] [Pubmed]
- Booth CM, Matukas LM, Tomlinson GA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. Jama 2003; 289:2801-2809.
[Crossref] [Google Scholar] [Pubmed]
- Azar WS, Njeim R, Fares AH, et al. COVID-19 and diabetes mellitus: how one pandemic worsens the other. Rev Endocr Metab Disord 2020; 21:451-463.
[Crossref] [Google Scholar] [Pubmed]
- Gianchandani R, Esfandiari NH, Ang L, et al. Managing hyperglycemia in the COVID-19 inflammatory storm. Diabetes 2020; 69:2048-2053.
[Crossref] [Google Scholar] [Pubmed]
- Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: Knowledge in progress. Diabetes Res Clin Pract 2020; 162:108142.
[Crossref] [Google Scholar] [Pubmed]
- Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci 2020; 12:1-5.
[Crossref] [Google Scholar] [Pubmed]
- Soleimani A, Kazemian S, Karbalai Saleh S, et al. Effects of Angiotensin Receptor Blockers (ARBs) on in-hospital outcomes of patients with hypertension and confirmed or clinically suspected COVID-19. Am J Hypertens 2020; 33:1102-1111.
[Crossref] [Google Scholar] [Pubmed]
- Yang JK, Lin SS, Ji XJ, et al. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta diabetol 2010; 47:193-199.
[Crossref] [Google Scholar] [Pubmed]
- Lim S, Bae JH, Kwon HS, et al. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol 2021; 17:11-30.
- Corrao S, Pinelli K, Vacca M, et al. Type 2 diabetes mellitus and COVID-19: a narrative review. Front Endocrinol 2021; 12.
[Google Scholar] [Pubmed]
- Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol-Endocrinol Metab 2020.
- Moghaddam Tabrizi F, Rasmi Y, Hosseinzadeh E, et al. Diabetes is associated with higher mortality and severity in hospitalized patients with COVID-19. EXCLI j 2021;20:444-53.
[Google Scholar] [Pubmed]
- Deng YP, Xie W, Liu T, et al. Association of diabetes with severity and mortality in hospitalized patients with COVID-19 in Wuhan, China: a single-centered, retrospective study. Arch Endocrinol Metab 2021; 65:596-608.
- Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis 2020; 71:762-768.
- Yang JK, Lin SS, Ji XJ, et al. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol 2010; 47:193-199.
- Apicella M, Campopiano MC, Mantuano M, et al. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol 2020; 8:782-792.
- Singh AK, Singh R, Joshi SR, et al. Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabetes Metab Syndr: Clinical Research and Reviews 2021; 15:102146.
[Crossref] [Google Scholar] [Pubmed]
- Patel A, Kaur H, Xess I, et al. A multicentre observational study on the epidemiology, risk factors, management and outcomes of mucormycosis in India. Clin Microbiol Infect 2020; 26:944-949.
[Crossref] [Google Scholar] [Pubmed]
- Song G, Liang G, Liu W. Fungal co-infections associated with global COVID-19 pandemic: a clinical and diagnostic perspective from China. Mycopathologia 2020; 185:599-606.
[Crossref] [Google Scholar] [Pubmed]
- Selarka L, Sharma S, Saini D, et al. Mucormycosis and COVIDâ?19: An epidemic within a pandemic in India. Mycoses 2021; 64:1253-1260.
- Chavda VP, Apostolopoulos V An opportunistic infection in the aged immunocompromised individual: A reason for concern in COVID-19. Maturitas 2021; 154:58-61.
- Baldin AS, Ibrahim. Molecular mechanisms of mucormycosis-The bitter and the sweet. PLoS Pathog 2017; 13:1006408
[Pubmed]
- Petrikkos G, Skiada A, Lortholary O, et al. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis 2012; 54:23-34.
[Crossref] [Google Scholar] [Pubmed]
- Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169:467-473.
Author Info
Shiv Joshi* and Shubhangi Shreysee
Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi (Meghe), Maharashtra, IndiaCitation: Shiv Joshi, Shubhangi Shreysee, Review on impact of diabetes mellitus on COVID-19 mortality and severity, J Res Med Dent Sci, 2022, 10 (7): 000-000.
Received: 31-May-2022, Manuscript No. JRMDS-22-50013; , Pre QC No. JRMDS-22-50013; Editor assigned: 02-Jun-2022, Pre QC No. JRMDS-22-50013; Reviewed: 20-Jun-2022, QC No. JRMDS-22-50013; Revised: 01-Aug-2022, Manuscript No. JRMDS-22-50013; Published: 08-Aug-2022