Case Report - (2021) Volume 9, Issue 12
REPLACEMENT OF MISSING HALLUX WITH GLOVE TYPE SILICONE PROSTHESIS- A CASE REPORT
Abstract
Loss of hallux produces significant esthetic and functional deficiencies. The concealment of an amputated part with the help of prosthesis can shield an amputee from social stigma. Prosthesis for such patient must be comfortable to wear lightweight, durable, cosmetically pleasing easy to put on and remove. The prosthetic rehabilitation of an amputated finger/toe is considered when microvascular reconstruction is not possible, unavailable, unsuccessful, or unaffordable. Replacement by prosthesis offers psychological support and social acceptance in such cases. This clinical report describes a method to fabricate glove retained silicone toe prosthesis in a patient with greater toe loss.
Keywords
Missing hallux, Silicone prosthesis, Mechanical retentionIntroduction
Prosthetics is an art and science which offers a natural appearance to the lost structures of the patient. Loss of hallux produces significant esthetic and functional deficiencies [1]. Most common methods to replace the loss of finger or hallux are endoprosthesis, e.g., implants and exoprosthesis, e.g., silicon prosthesis, acrylic prosthesis, prosthesis using attachments, and magnets. Passing through various materials, the acceptance rate has been much higher when an individually sculpted custom restoration using silicone elastomer. Silicone is the material of choice in fabricating prosthesis due to acceptable strength and durability [2]. To aid in retention of the prosthesis, adhesives, or mechanical methods can be incorporated. This report presents a case of rehabilitation of a hallux defect with a silicone prosthesis and describes a method of retention for the same.
Case report
A male patient, aged 38 years, reported to the department, with a history of loss of right hallux (greater toe), about 3 years back, due to occupation-related trauma. Clinical examination of the affected foot revealed amputated hallux from metatarsal phalangeal joint (Figure 1). The surrounding area appeared to be normal with no signs of any infection. Glove type toe prosthesis was planned for the replacement of the missing hallux. After having informed consent from the patient, to ensure his willingness and cooperation the treatment was executed.
Figure 1: Preoperative photograph showing missing hallux of right foot.
Technique of fabrication
Impression making
The patient’s foot with missing hallux was lubricated with a thin layer of petroleum jelly and the area around the foot was boxed. A thin layer of irreversible hydrocolloid impression material was placed over the plantar side first and then the dorsum aspect of foot. The patient was instructed to keep the foot in the normal resting position without stretching while impression making (Figure 2a & b). Also impression of the left foot was made following the same procedure.
Figure 2(a & b): Impression making of the affected foot.
Model preparation
When the material was set the impression was retrieved and fabrication of model was carried out. Both the impressions were poured in stone plaster, type-III (Figure 3a & b). At the same appointment another impression was made of patient’s left foot hallux in a combination of light body and putty (Figure 4). The impression of the patient’s left foot hallux was poured with wax. The pattern was retrieved from the elastomeric impression.
Figure 3(a & b): Stone model obtained of right (a) & left foot (b)
Figure 4: Putty and light body impression made of hallux of left foot.
Wax pattern fabrication and try in
The wax pattern was then adjusted by sculpting and adapted on the working cast. Approximate length and angulations were determined on working cast and later confirmed during trial of wax pattern (Figure 5). The wax pattern was tried on the patients affected foot (Figure 6).
Figure 5: Wax-pattern for prosthesis.
Figure 6: Try-in of wax pattern.
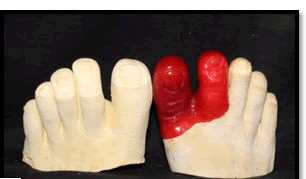
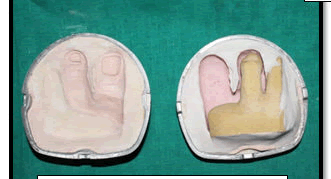
Investment technique
The master cast was duplicated and the duplicate cast was used for investing. The pattern was sealed to the master cast at the junction, where the margins of the pattern overlapped the cast. The pattern and the cast were then invested in a large size flask. The mold was first poured only up to half of the pattern (Figure 7). Separating medium was applied and then the other half was poured, wax was eliminated in the conventional way (Figure 8).
Figure 7: Flasking of the wax pattern.
Figure 8: Dewaxing
Color matching
Appropriate shade matching was done during day time. Two shades of silicone were used for dorsal surface of the toe and the second which would represent the plantar surface of the artificial toe. A base color mixture of the silicone material was prepared; the lighter shades were used for plantar surface and darker shades were used for color matching of dorsal surface. After attaining closest possible match, the mold cavity was filled by first coating the silicone material prepared for plantar surface of toe and in other mold silicone material prepared for dorsal surface of toe was placed to fill the mold cavity (Figure 9a, b & c). The two pieces were re-assembled and excess silicone was expressed using light pressure. The mold was then clamped and placed into a dry heat oven at the manufacturer’s prescribed time and temperature. After polymerization, the mold was allowed to cool at room temperature, opened and flash removed with a sharp scalpel and finished with an abrasive stone.
Final prosthesis
The final prosthesis was obtained and was trimmed and finished (Figure 10). Nail was fabricated using cold cure clear acrylic and attached to the prosthesis using cyanoacrylate. The prosthesis was tried in the patient. Extrinsic staining and dematting was done to match the exact color (Figure11a & b). The prosthesis was finally delivered to the patient after giving instructions regarding its maintenance.
Patients follow up
For prostheses evaluation, the patient was asked to return on day 1 and 7 for follow-ups. There after a 6 month follow-up was done and it was noted that the patient had no complaints and was satisfied about esthetics and comfort of the toe prostheses.
Discussion
Body deformity may cause physical, emotional, and psychological as well as social damage to the patient. In this technique conventional impression method is used which has a certain advantage over the older technique. It is a less cumbersome quick, easy and economical technique using minimal material [3]. For making of wax pattern the same person’s unaffected foot can be used to eliminate the error in respect to size and shape. We can also use the analogous finger technique.
Wax was preferred over clay to make the pattern because residual oils from clay contaminate the mold surface, which interferes with the platinum catalyst employed in silicone prosthesis materials. The resultant wax was pliable enough to form into small shapes with fingers when warm, yet stiff enough to carve with an instrument when chilled. Placing it in chilled water for some time prevents distortion of the pattern [4]. If any surface details were lost, then the wet gauze technique was used to recreate surface details. Silicone prostheses do not have color longevity. The ideal color properties required in a maxillofacial prosthetic material must accept and retain intrinsic and extrinsic coloration.
Despite the advances in the microsurgical techniques, the reconstruction of the amputated digits for a number of patients may not be successful and they can be more benefitted with passive prostheses. The primary purpose of prosthesis is to allow the patient to pass unnoticed, and concealment of prosthesis usage has been found to be an effective coping strategy. Owing to the wider rate of acceptance, comfort, durability, stain resistance of customized silicone prostheses and patients unwillingness to go for any surgical procedure involving implants, the above‑explained method of fabrication of prosthesis was opted [5]. The additional functional benefits of silicone prostheses include desensitization and protection of the painful hypersensitive tissue at the amputation site by constant gentle pressure exerted over the affected area. It has also been speculated that silicone gel improves the hydration of the stratum, making the scar tissue more pliable, and comfortable. Various methods of retention are available (i.e., using rings over the margins of the finger prosthesis, using medical grade adhesive, or by implant‑retained prosthesis.
Conclusion
It is the primary responsibility of the prosthodontist to restore the function, comfort, and esthetics with a well‑fabricated prosthesis. Hence, an attempt was made to fabricate a glove type toe prosthesis by simple method and found successful. The prosthesis is comfortable to wear, lightweight, durable, cosmetically pleasing easy to put on and remove. Thus fabrication of such prosthesis not only provides psycological comfort but also helps to regain the patient’s lost self-confidence.
References
- Kini AY, Byakod PP, Angadi GS, Pai U, Bhandari AJ. Comprehensive prosthetic rehabilitation of a patient with partial finger amputations using silicone biomaterial: a technical note. Prosthet Orthot Int 2010;34(4):488-94.
- Huber H, Studer SP. Materials and techniques in maxillofacial prosthodontic rehabilitation. Oral Maxillofac Surg Clin North Am 2002;14(1):73-93
- Lundborg G, Brnemark PI, Rosen B. Osseointegrated thumb prostheses: a concept for fixation of digit prosthetic devices. The J HAND SURG-AM 1996;21(2):216-21.
- Matussek J, Neff G. The artificial hand. An overview of hand prostheses. Der Orthopade 2003;32(5):406-12.
- Gary JJ, Smith CT. Pigments and their application in maxillofacial elastomers: a literature review. J Prosthet Dent 1998;80(2):204-8.