Case Report - (2022) Volume 10, Issue 11
Rare Presentation of Tetralogy of Fallot with Pulmonary Atresia in New Born-A Case Report
Prithvi Raj, Ravanagomagan* and Jagadeeswari
*Correspondence: Dr. Ravanagomagan, Department of Paediatrics, Sree Balaji Medical College, Chromepet, Chennai, Tamilnadu, India, Email:
Abstract
Tetralogy of Fallot with Pulmonary valve Atresia and Major Aortopulmonary Collateral Arteries (TOF/PA/MAPCAs) is the most extreme variant of TOF. Presentation is relatively rare, with a reported incidence of 0.7 per 10,000 live births. Without flow through PDA, major Aortopulmonary collateral arteries play a major role in maintaining pulmonary blood flow. The management is based on the anatomy of MAPCAs and the nature of PDA. The goal of surgical management is to construct completely separate in series pulmonary and systemic circulations. The Procedure is done by unifocalization, which involves detachment of collateral vessels from their aortic origins and anastomosis to the central pulmonary arteries, followed by reconstruction of RVOT using an allograft valved conduit from the RV that results in ante grade pulmonary blood flow, followed by closure of VSD. Here, we report a case of a Term, boy baby, born to nonconsanguineous parents by caesarean section with birth weight of 2.508 kg. The baby cried immediately after birth with APGAR scores 8 at 1’ and 9 at 5 minutes and did not require resuscitation with subsequent details as follows.
Keywords
MAPCAs, Unifocalization, Tetralogy of fallot
Introduction
Tetralogy of fallot with Pulmonary valve Atresia and Major Aortopulmonary Collateral Arteries (TOF/PA/MAPCAs) is the most extreme variant of TOF, in which complete atresia of the pulmonary valve replaces pulmonary stenosis along with ventricular septal defect, overriding of aorta and right ventricular hypertrophy.
Presentation is relatively rare, with a reported incidence of 0.7 per 10,000 live births. Without flow through PDA, MAPCAs play a major role in maintaining pulmonary blood flow. The clinical presentation and management decisions are based on the character of the MAPCAs and presence of PDA.
Case Presentation
We report a case of Term, boy baby born to nonconsanguineous parents by caesarean section with birth weight of 2.508 kg. The baby cried immediately after birth with APGAR scores 8 at 1’ and 9 at 5 minutes and did not require resuscitation. At 10 minutes of birth, on pulse oximetry the baby’s saturation was less than 90% in all four limbs even after supported with 100% oxygen and maintained the same thereafter. Baby’s other vitals were stable and there were no signs of cyanosis, respiratory distress and heart failure.
The mother’s antenatal history was insignificant and she was not on any medications. There was no family history of congenital heart disease.
The baby had no obvious external congenital anomalies. His cardiac examination revealed the presence of single second heart sound with systolic murmur heard throughout the precordium. The baby was shifted to NICU for further observation.
Management
Under observation in NICU, the baby underwent cardiac evaluation, chest x-ray showed a boot shaped heart, ECHO showed presence of TOF. CTVS opinion was obtained and was advised for CT pulmonary angiography. It showed features of TOF a sub aortic VSD of size 1.1 cm, right sided aortic arch with overriding of aorta with MPA stenosis, right and left pulmonary artery were draining through PDA with formation of multiple MAPCAs.
As the child was alert, active and tolerating paladai feeds well and was haemodynamically stable with saturation maintaining >85% in all four limbs in room air, the child was discharged from NICU with the follow up advice to check saturation levels at home daily as advised by cardiothoracic surgeon. Parents were advised to report to hospital in case of any cyanotic episodes and in case of fall in saturation levels <70%. The child was advised for surgery in future, by unifocalization procedure with entire reconstruction of the Right Ventricular Outflow Tract (RVOT) with closure of VSD (Figures 1-3).
Figure 1: Boy baby born to non-consanguineous parents by caesarean section.
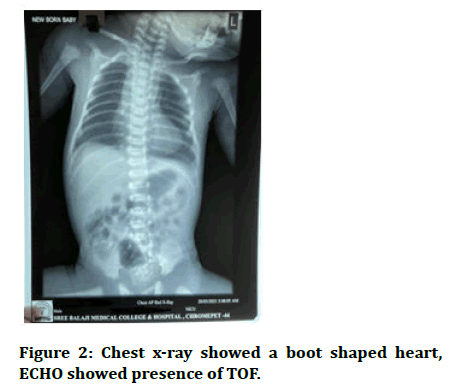
Figure 2: Chest x-ray showed a boot shaped heart, ECHO showed presence of TOF.
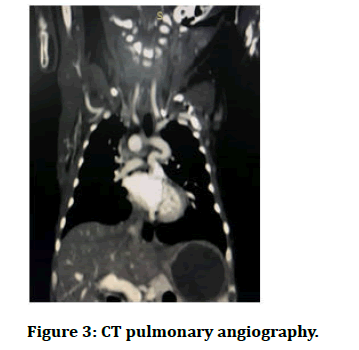
Figure 3: CT pulmonary angiography.
Discussion
An estimated 60-70% of major aortopulmonary collateral arteries from the midpoint of the descending aorta, an estimated 10-20% from the inferior aspect of the arch of aorta, and a negligible portion from the subclavian, coronary arteries and distal part of descending aorta [1].
The course of the major aortopulmonary collateral arteries embedded in the mediastinum is not well understood and is observed to be traversed along the posterior part of the oesophagus and the trachea, observed usually traversing in between the above mentioned structures in to the pulmonary hilum [2].
The management is based on the anatomy of MAPCAs and the nature of PDA. In our case, the baby remained asymptomatic without cyanosis at birth due to the presence of well-developed MAPCAs with presence of PDA. But in few cases, these vessels are restrictive and pulmonary blood flow is low, resulting in significant cyanosis requiring immediate intervention [3]. Certain cases in which the flow is excessive Pulmonary Hypertension (PH) may develop resulting in heart failure.
In patients with in adequate pulmonary blood flow (low oxygen saturation), medical management is focused on increasing the pulmonary flow by administration of Prostaglandin E1 (Alprostadil) to maintain patency of the ductus arteriosus [4], which is not indicated in our case.
The goal of surgical management is to construct completely separate in series pulmonary and systemic circulations. The procedure is done by unifocalization, which involves detachment of collateral vessels from their aortic origins and anastomosis to the central pulmonary arteries, followed by reconstruction of RVOT using an allograft valved conduit from the RV that results in ante grade pulmonary blood flow, followed by closure of VSD [5], which was planned in our case.
Conclusion
• Early identification and surgical intervention is the key in reducing mortality in such rare presentation of TOF.
• Pulse oximetry screening plays a major role in detecting the presence of congenital heart defects even in asymptomatic babies.
• Infants awaiting surgical intervention should be monitored at regular intervals for weight gain and saturation levels for worsening of cyanosis.
References
- Jefferson K, Rees S, Somerville J. Systemic arterial supply to the lungs in pulmonary atresia and its relation to pulmonary artery development. Br Heart J 1972; 34:418-427.
- Liao PK, Edwards WD, Julsrud PR, et al. Pulmonary blood supply in patients with pulmonary atresia and ventricular septal defect. J Am Coll Cardiol 1985; 6:1343-1350.
- Rabinovitch M, Herrera deLeon V, Castaneda AR, et al. Growth and development of the pulmonary vascular bed in patients with tetralogy of fallot with or without pulmonary atresia. Circulation 1981; 64:1234-1249.
- Malhotra SP, Hanley FL. Surgical management of pulmonary atresia with ventricular septal defect and major Aortopulmonary collaterals: A protocol based approach. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2009; 12:145-151.
- Kirklin JW, Blackstone EH, Kirklin JK, et al. Surgical results and protocols in the spectrum of tetralogy of fallot. Ann Surg 1983; 198:251-265.
Author Info
Prithvi Raj, Ravanagomagan* and Jagadeeswari
Department of Paediatrics, Sree Balaji Medical College, Chromepet, Chennai, Tamilnadu, IndiaCitation: Prithvi Raj, Ravanagomagan, Jagadeeswari, Rare Presentation of Tetralogy of Fallot with Pulmonary Atresia in New Born- A Case Report, J Res Med Dent Sci, 2022, 10 (11): 060-062.
Received: 02-Sep-2022, Manuscript No. JRMDS-22-57366; , Pre QC No. JRMDS-22-57366(PQ); Editor assigned: 06-Sep-2022, Pre QC No. JRMDS-22-57366(PQ); Reviewed: 21-Sep-2022, QC No. vJRMDS-22-57366; Revised: 03-Nov-2022, Manuscript No. JRMDS-22-57366(R); Published: 10-Nov-2022
