Review Article - (2024) Volume 12, Issue 4
Progressive Supranuclear Palsy: What We Need to Know and What are the Treatment Options for this Neurological Disorder
*Correspondence: Reema A Sharaf, Department of Restorative Dentistry, Prince Sultan Medical Military City, Riyadh, Saudi Arabia, Email:
Abstract
Progressive Supranuclear Palsy (PSP) is a rare brain disorder. Treatment of patients with PSP is both effective and beneficial. This case review aims to share our experience with active management of PSP, considering the patient, family, and medical context in which the disease occurs. There are many opportunities to help your patients, improve their symptoms, reduce their risk, and harm, and guide them through the complex medical, social, and legal minefields that characterize life with chronic neurological conditions. We summarize the challenges of early diagnosis, consider PSP mimics, and the role of investigations in excluding these, and discuss the available pharmacological and non-pharmacological treatment strategies to tackle the common and challenging symptoms of PSP. The best treatment for PSP should be patient-centered and involve a multidisciplinary team.
Keywords
Progressive Supranuclear Palsy (PSP), Neurodegenerative disease, Parkinson disease, Multiple system atrophy
Introduction
Progressive Supranuclear Palsy (PSP) is a rare neurodegenerative disease with a prevalence of five to six people per 100,000 population [1]. The clinical examination findings are diverse and PSP cases are often under-diagnosed or misdiagnosed. Parkinsonism’s symptoms and signs (i.e., tremor, bradykinesia, rigidity, and postural instability) can be prominent in neurodegenerative disorders other than idiopathic Parkinson disease, particularly in atypical parkinsonian disorders, which include Corticobasal Degeneration (CBD), Multiple System Atrophy (MSA), and PSP. The PSP, also known as Steele-Richardson-Olszewski syndrome, is an uncommon but not rare Parkinsonian syndrome. Characteristic features of PSP and its variants include vertical supranuclear gaze palsy, postural instability with unexplained falls, akinesia, and cognitive dysfunction. The clinical hallmarks of PSP are: (1) Vertical gaze palsy; (2) Pseudobulbar palsy; (3) Axial rigidity; and (4) Cognitive impairment. Falls are included in the first year of illness, and more specifically in supranuclear gaze palsy [2].
Clinical presentations of PSP
PSP often affects movements, gait, balance, speech, swallowing, eye movements and vision, as well as mood behavior and thinking. The pattern of signs and symptoms can be different from person to person. The most frequent and first symptom of PSP is a loss of balance while walking. Individuals may have abrupt and unexplained falls without loss of consciousness, a stiff and awkward gait, or slow movement [3]. As the disease progresses, most people will begin to develop a blurring of vision and problems controlling eye movement. These symptoms may include as follow: (a) Slow eye movements, (b) Trouble voluntarily shifting gaze vertically (i.e., downward and/or upward), (c) Trouble controlling eyelids, tendency to move the head to look in different directions, (d) Involuntary closing of the eyes, (e) Prolonged or infrequent blinking, (f) Difficulty in opening the eyes, and (g) Inability to maintain eye contact during a conversation. In addition to the above symptoms, people with PSP often show alterations of mood and behavior [4]. These symptoms may include: (a) Depression, (b) Apathy, (c) Changes in judgment, insight, and problem solving, (d) Difficulty finding words, (e) Loss of interest in ordinary pleasurable activities, (f) Increased irritability and forgetfulness, (g) Sudden laughing or crying or displaying angry outbursts for no apparent reason, and (h) Personality changes. Moreover, these people may have other signs and symptoms, which include: (a) Slowness of thought, (b) Memory problems, (c) Slowed, slurred, or monotone speech, (d) Difficulty swallowing solid foods or liquids, and (e) Mask-like facial expressions.
Differential diagnosis
PSP is often misdiagnosed as Parkinson’s disease, especially early in the disorder, as they share many symptoms, including stiffness, movement difficulties, clumsiness, bradykinesia (slow movement), and rigidity of muscles [5]. The onset of both diseases is in late middle age. However, PSP progresses more rapidly than Parkinson’s disease [6]. Diagnostic criteria of PSP are given in below [7].
Diagnostic criteria for PSP
Mandatory inclusion criteria
• Postural instability with falls in the first year of symptoms.
• Slowing of vertical saccadic eye movements (clinically possible); vertical supranuclear gaze palsy (clinically probable).
Supportive criteria
• Frontal/sub-cortical cognitive dysfunction.
• Axial rigidity.
• Pseudobulbar dysphagia and dysarthria.
• Blepharospasm/apraxia of eyelid opening.
How is PSP different from Parkinson’s disease
Table 1 details the differentiating features between people with PSP usually stand exceptionally straight or occasionally tilt their heads backward (and tend to fall backward) [6]. This is termed “axial rigidity.” Those with Parkinson's disease usually bend forward. Problems with speech and swallowing are much more common and severe in PSP than in Parkinson's disease and tend to show up earlier in the disease. Eye movements are abnormal in PSP but close to normal in Parkinson's disease. Tremor is rare in PSP but very common in individuals with Parkinson’s disease. Although individuals with Parkinson's disease markedly benefit from the drug levodopa, people with PSP respond minimally and only briefly to this drug. People with PSP show accumulation of the protein Tau in affected brain cells, whereas people with Parkinson’s disease show accumulation of a different protein called alpha-synuclein.
| Clinical features | PSP | PD |
|---|---|---|
| Balance | Early postural instability | Initially well preserved gait and balance |
| Speech | Growling dysarthria | Hypophonic dysarthria |
| Facial appearance | Taut | Loose |
| Extrapyramidal features | Axial rigidity; relatively well preserved fine finger movements; tremor in <10% | Distal rigidity and bradykinesia; decrement in amplitude and speed of fine finger movements; tremor in 95% through disease course |
| Symmetry | Symmetry of symptoms and signs | Asymmetry of onset and persistent asymmetrical signs |
| L-DOPA | Little response to L-DOPA | Excellent response to L-DOPA |
Table 1: Clinical presentation of Parkinson’s disease (PD) and PSP.
What are the causes of the PSP?
The exact cause of PSP is unknown. Research, however, said that it is a slow degeneration of brain cells in a few distinct regions of the brain, primarily the brain stem [8]. The substantia nigra, is where brain cell loss occurs, which contributes to the motor symptoms shared by Parkinson's disease and PSP. The hallmark of PSP is the accumulation of abnormal deposits of the protein Tau in nerve cells in the brain. These deposits cause the cells to malfunction and die, which stops the flow of information to other nerve cells. The accumulation of Tau puts PSP in the group of disorders called tauopathies, which includes Alzheimer’s disease, corticobasal degeneration, and some forms of frontotemporal degeneration.
PSP is usually sporadic, meaning that it occurs infrequently and without a known cause. In very few cases, the disease results from mutations in the Microtubule-Associated Protein Tau (MAPT) gene [9]. This mutation provides faulty instructions for making Tau to the nerve cell. Genetic factors have not been implicated in most individuals.
Several theories suggest that PSP might be caused by:
• Protein: The abnormal build-up of the protein Tau in a cell causes the building up a connected cell, which then spreads through the nervous system [10];
• Infection: An unconventional infectious agent that takes years or decades to start producing visible effects (as is seen in disorders like Creutzfeldt-Jakob Disease) [11];
• Genetics: Random genetic mutations—the kind that occur in individuals all the time-happen to occur in particular cells or certain genes, in a specific combination that injures these cells [12];
• Chemicals: Exposure to some unknown chemical in food, air, or water, which slowly damages certain vulnerable areas of the brain, mimicking a neurological disorder found on the Pacific island of Guam and on a few neighboring islands; and
• Cellular damage: caused by free radicals, which are reactive molecules produced continuously by all cells during normal metabolism. Although the body has built-in mechanisms for clearing free radicals from the system, scientists suspect that-under certain circumstances-free radicals can react with and damage other molecules.
How is PSP diagnosed?
Currently there are no tests and/or brain imaging techniques to definitively diagnose PSP. An initial diagnosis is based on the person’s medical history and a physical and neurological exam. Identifying early gait problems, problems moving the eyes, speech and swallowing abnormalities, as well as ruling out other similar disorders is important. Diagnostic imaging may show shrinkage at the top of the brain stem and look at brain activity in known areas of degeneration.
Is there any treatment for PSP?
There is currently no effective treatment for PSP and symptoms usually do not respond to medications [13]. Parkinson’s disease medications, such as ropinirole, rarely provide additional benefit. In some individuals, other antiparkinsonian medications, such as levodopa, can treat the slowness, stiffness, and balance problems associated with PSP, but the effect is usually minimal and short-lasting. Botulinum toxin, which can be injected into muscles around the eyes, can treat excessive eye closing. Some antidepressant drugs may offer some benefits beyond treating depression, such as pain relief and decreasing drooling. Non-drug treatment for PSP can take many forms. Weighted walking aids can help individuals avoid falling backward. Bifocals or special glasses called prisms are sometimes prescribed for people with PSP to remedy the difficulty of looking down. Exercise supervised by a healthcare professional can keep joints limber but formal physical therapy has no proven benefit in PSP. A gastrostomy (a surgical procedure that involves the placement of a tube through the skin of the abdomen into the stomach for feeding purposes) may be necessary when there are swallowing disturbances or the definite risk of severe choking. Deep Brain Stimulation (DBS)-which uses surgically implanted electrodes and a pacemaker-like medical device to deliver electrical stimulation to specific areas in the brain to block signals that cause the motor symptoms of several neurological disorders and other surgical procedures commonly used in individuals with Parkinson's disease have not been proven effective in PSP [14].
What is the prognosis for PSP?
The disease gets progressively worse, with people becoming severely disabled within three to five years of onset. Affected individuals are predisposed to serious complications such as pneumonia, choking, head injury, and fractures. The most common cause of death is pneumonia. With good attention to medical and nutritional needs, it is possible for individuals with PSP to live a decade or more after the first symptoms of the disease appear.
Literature Review
Clinical history
In 2019, a 64-year-old female who reported recurrent falls and gait and balance problems for three years. Falls were mild, moderate, and sometimes it was very severe. There was no dizziness or loss of consciousness. She was having depression and non-specific memory problems. Medically, she reported hypothyroidism, and she was taking thyroxin 75 mg once a day. She had a history of total knee replacement for both knees done in 2006 with no complications. She reported a history of cigarette smoking for more than 20 years. She has been seen by a neurologist who started her on Plavix. Her family history was unremarkable. She went to a lot of medical clinics to help find out her problem, but none were helpful. In the same year 2019 and due to recurrent falls one of her prosthetic knees loosened. She had gone to revision surgery for the affected knee prosthesis. Following the surgery her family reported episodes of hallucination and was imagining pictures and some people. She reported depression and nonspecific memory problems. In December 2019, she had been seen by a neurologist who diagnosed her with Progressive Supranuclear Palsy with Parkinsonism (PSP-P). She started to show signs of dementia and loss of memory. Speech problems and heavy tongue were also noticed.
MRI findings
Mild diffuse volume loss of the brain with no predilection. Small patches of signal abnormality in deep white matter of both cerebral hemispheres, more in the parietal lobes representing moderate chronic ischemic changes. Tiny dots of susceptibility in the right occipital lobe represent old microhemorrhages. No acute infarction, mass effect or hydrocephalus. Orbits and nasopharynx are clear. Mild mucosal thickening of ethmoid sinuses. Previous facial fillers with no complication.
Conclusion: Mild diffuse volume loss. Moderate chronic ischemic changes. No acute brain abnormalities (Figure 1).
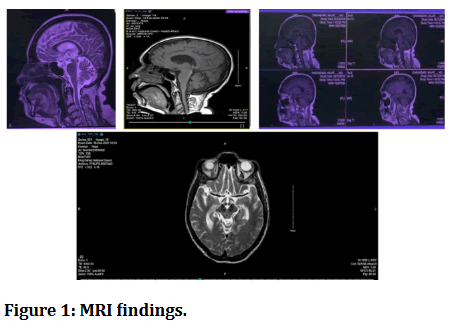
Figure 1: MRI findings.
Neurological findings
• Masked face and decreased fine motor skills (poor
mobility).
• Hypophonia.
• Gait difficulties that progress at faster rate (sever gait
disturbances) (Figure 2).
• Slow walking evolves into lunching steps.
• Tendency to topple forward or backward.
• Frontal cognitive impairment which is characterized
by: Slowness of thinking and response time impaired
attention, dismissed verbal fluency, and difficulty
shifting cognitive sets.
• Apathy with depression.
• Bulbar dysfunction.
• Eye movement abnormalities-diplopia (Figure 3).
• Dysphasia that is sever enough to require feeding
tube.

Figure 2: Gait abnormalities.
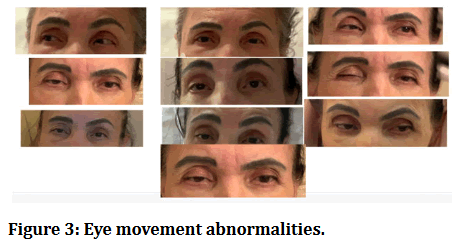
Figure 3: Eye movement abnormalities.
CT pelvis report
There was a non-displaced vertical fracture involving the left side of the sacrum, adjacent to the sacroiliac joint (Figure 4). Also noted well corticated displaced fracture of the left inferior pubic ramus with adjacent bone fragments. A displaced fracture of the left superior pubic ramus was seen with adjacent soft tissue density which likely representing hematoma with fibrosis related to the trauma. Degenerative changes were seen in both sacroiliac joints and the pubis symphysis. Degenerative changes were also seen in the lower lumbar spine. No hip dislocation can be identified.
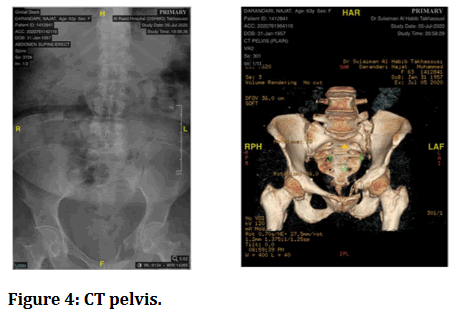
Figure 4: CT pelvis.
Case progression
Three years ago, the patient was in a better condition. She can walk alone but after a while she needed assistance, she can move her hands and feet but in a slow action. She started to have gait unbalance. Dementia and dysphasia were progressively deteriorating. Symptoms continued to worsen during this period until it was difficult for her to talk, look, walk, move, and hold things.
Then, the patient had frequent respiratory obstruction episodes and was transferred to emergency. Neurological examination showed impaired vertical and incomplete lateral gaze. Her speech was slow and monotonous. Contractures were prominent in the neck muscles and elbows. The deep tendon reflexes were increased in the lower extremities. Babinski sign was negative. Snout and forced grasping reflexes were elicited. She showed marked bradykinesia. Brisk reflexes in both upper limbs with positive Hofmann reflex. Magnetic Resonance Imaging (MRI) revealed a midbrain atrophy showing the following: Hummingbird sign also known as Penguin sign. Mickey Mouse appearance, and Morning Glory sign. Single photon emission tomography showed severe hypoperfusion in the frontal cortex. No improvement was provided by the administration of Levodopa-Carbidopa (Sinement). It is primarily used to manage the symptoms of Parkinson’s Disease, but it does not slowdown or stop it from getting worse. Three months ago, the patient developed sudden cellulitis on the right side of her face. Swelling was extending from the lower eyelid of the right eye going down to the right angle of the mandible involving the upper and lower lips. The patient cannot talk or communicate, ambulatory care came to evaluate the case. The facial examination and intra oral examination were difficult due to difficulty in mouth opening because of muscle stiffness. Intra oral radiograph taken with portable x-ray device, there was periapical radiolucency related to maxillary second premolar. The tooth has been extracted under local anesthesia and she was given antibiotics.
Lately, inspiratory stridor (noisy breathing) developed during the episodes due to collapsed tissues above the Vocal Cord (VC). Patient has been admitted following the fourth episode of stridor. The fiberoptic laryngoscopic examination demonstrated bilateral abduction failure.
An emergency tracheostomy has been done under general anesthesia to relieve her respiratory distress. Although Vocal Cord Abductor Paralysis (VCAP) rarely occurs in neurodegenerative disorders other than multiple system atrophy, attention to VCAP should be required in PSP patients.
Discussion
Progressive Supranuclear Palsy (PSP) is an uncommon and incapacitating neurodegenerative condition that mostly impacts the brain stem and basal ganglia. The condition is defined by a gradual deterioration of voluntary eye movements, specifically in vertical gaze, along with a reduction in cognitive function, problems with maintaining balance, and symptoms of parkinsonism. This case report outlines the clinical progression and treatment of a 64-year-old female patient who has been diagnosed with Progressive Supranuclear Palsy (PSP). The patient initially exhibited recurring episodes of falling and experienced difficulties with their gait and balance. Throughout the subsequent year, she experienced a gradual decrease in the speed of her vertical eye movements, stiffness, slow movement, difficulty speaking, and decline in cognitive function. These symptoms are characteristic signs of Progressive Supranuclear Palsy (PSP). The brain's Magnetic Resonance Imaging (MRI) showed distinct signs, such as shrinkage in the midbrain tegmentum and the superior cerebellar peduncles, confirming the diagnosis of PSP.
This case report emphasizes the significance of promptly identifying the clinical characteristics of PSP, since this can direct the appropriate diagnostic investigation and treatment. The authors emphasize that although there is no remedy for PSP, a comprehensive strategy comprising neurologists, physical therapists, occupational therapists, and speech-language pathologists can effectively address the symptoms and enhance the patient's quality of life. Nevertheless, no noticeable effect was observed following the administration of Levodopa-Carbidopa (Sinemet). It is mostly utilized to mitigate the symptoms of Parkinson's Disease, although it does not impede or halt its progression. Similarly, a prior case study examines the utilization of pharmacological therapies, such as levodopa and cholinesterase inhibitors, which can offer limited alleviation from symptoms in certain patients [15]. Nevertheless, the authors highlight that the primary approach to managing PSP is supportive, with an emphasis on preserving mobility, reducing falls, and addressing cognitive and behavioral disorders.
Conclusion
We outline the difficulties in diagnosing PSP at an early stage, examine conditions that may resemble PSP, and explore the use of tests to rule out these conditions. Additionally, we analyze the many pharmacological and non-pharmacological approaches for managing the typical and difficult symptoms of PSP. This case report offers an important contribution to the existing body of knowledge, showcasing the clinical advancement of PSP and emphasizing the significance of a thorough, interdisciplinary approach to patient treatment. As our comprehension of the fundamental pathophysiology of PSP progresses, the pursuit of more efficient therapy approaches remains a crucial focus of continuing research.
References
- Barer Y, Chodick G, Cohen R, et al. Epidemiology of progressive supranuclear palsy: Real world data from the second largest health plan in Israel. Brain Sci. 2022; 12:1126.
[Crossref] [Google Scholar] [PubMed]
- Factor SA, Esper CD. Progressive supranuclear palsy (PSP): Clinical features and diagnosis. UpToDate. 2020.
- Armstrong MJ. Progressive supranuclear palsy: An update. Curr Neurol Neurosci Rep. 2018; 18:1-9.
[Crossref] [Google Scholar] [PubMed]
- Kobylecki C, Jones M, Thompson JC, et al. Cognitive-behavioural features of progressive supranuclear palsy syndrome overlap with frontotemporal dementia. J Neurol. 2015;262(4):916-22.
[Crossref] [Google Scholar] [PubMed]
- Fernández-Ferreira R, García-Santos RA, Rodríguez-Violante M, et al. Progressive supranuclear palsy as differential diagnosis of Parkinson's disease in the elderly. Rev Esp Geriatr Gerontol. 2019; 54:251-6.
[Crossref] [Google Scholar] [PubMed]
- Alster P, Madetko N, Koziorowski D, et al. Progressive supranuclear palsy—parkinsonism predominant (PSP-P)—a clinical challenge at the boundaries of psp and Parkinson's disease (PD). Front Neurol. 2020; 11:508368.
[Crossref] [Google Scholar] [PubMed]
- Ali F, Martin PR, Botha H, et al. Sensitivity and specificity of diagnostic criteria for progressive supranuclear palsy. Mov Disord. 2019; 34:1144-53.
[Crossref] [Google Scholar] [PubMed]
- Long L, Cai XD, Wei XB, et al. Progressive supranuclear palsy: What do we know about it? Curr Med Chem. 2015; 22:1182-93.
[Crossref] [Google Scholar] [PubMed]
- Dickson DW, Rademakers R, Hutton ML. Progressive supranuclear palsy: Pathology and genetics. Brain Pathol. 2007; 17:74-82.
[Crossref] [Google Scholar] [PubMed]
- Davis AA, Leyns CE, Holtzman DM. Intercellular spread of protein aggregates in neurodegenerative disease. Annu Rev Cell Dev Biol. 2018; 34:545-68.
[Crossref] [Google Scholar] [PubMed]
- von Gunten A, Nogueira E, Parmentier H, et al. Neurocognitive disorders in old age: Alzheimer’s disease, frontotemporal dementia, dementia with Lewy bodies, and prion and infectious diseases. Primary Care Mental Health in Older People: A Global Perspective. 2019; 251-98.
- Koziorowski D, Figura M, Milanowski LM, et al. Mechanisms of neurodegeneration in various forms of parkinsonism-Similarities and differences. Cells. 2021; 10:656.
[Crossref] [Google Scholar] [PubMed]
- Stamelou M, Höglinger G. A review of treatment options for progressive supranuclear palsy. CNS Drugs. 2016; 30:629-36.
[Crossref] [Google Scholar] [PubMed]
- Wen Y, Jiao B, Zhou Y. The application of deep brain stimulation for progressive supranuclear palsy: A systematic review. Front Neurol. 2022; 13:827472.
[Crossref] [Google Scholar] [PubMed]
- Ikram S, Parra-Payano VD, Kammaripalle TK, et al. Progressive supranuclear palsy: A case report and literature review. Arch Clin Med Case Rep. 2021; 5:838-45.
Author Info
Department of Restorative Dentistry, Prince Sultan Medical Military City, Riyadh, Saudi ArabiaCitation: Reema A Sharaf, Progressive Supranuclear Palsy: What We Need to Know and What are the Treatment Options for this Neurological Disorder, J Res Med Dent Sci, 2024, 12 (4): 001-006
Received: 10-May-2024, Manuscript No. JRMDS-24-138869; , Pre QC No. JRMDS-24-138869 (PQ); Editor assigned: 17-May-2024, Pre QC No. JRMDS-24-138869 (PQ); Reviewed: 31-May-2024, QC No. JRMDS-24-138869; Revised: 07-Jun-2024, Manuscript No. JRMDS-24-138869 (R); Published: 14-Jun-2024
