Research Article - (2022) Volume 10, Issue 10
Processing the Extracted Tooth to Graft the Fresh Socket (Split Mouth Prospective Clinical Study)
Farah Abid Yousif* and Saif Saadedeen Abdulrazaq
*Correspondence: Dr. Farah Abid Yousif, Department of Oral and Maxillofacial Surgery, Dental Teaching Hospital, College of Dentistry, University of Baghdad, Bab-Almoadham, Baghdad, Iraq, Email:
Abstract
Background: The dimensional change of alveolar ridge is normal effect of teeth extraction, with unfavourable functional and esthetical outcomes that might jeopardize implant placement. To reduce the biological effects of the dimensional changes of alveolar ridge, various surgical procedures have been recommended, called alveolar ridge preservation. In the previous decade, autogenously teeth have been proposed as bone graft substitution in fresh extraction socket with successful results, yet with various preparation protocols.
Aim: Evaluate the formation of new bone derived from the freshly extracted teeth that are grafted immediately in the post extraction sockets, in comparison with sockets without graft filling, by using CBCT and to compare the vertical and horizontal contraction of alveolar ridge between both groups.
Materials and methods: Twenty patients with an overall of 40 extraction sockets were selected for this study from department of oral and maxillofacial surgery. These cases were divided in two groups, control group (20 extraction sockets left to heal by clot formation) and study group (20 extraction sockets grafted with autogenously teeth particulates). The extracted teeth were processed immediately with smart dentin grinder device. CBCT scans were taken on one week after extraction as baseline image and four months later.
Results: All extraction sites healed uneventfully. Reduction of ridge height and width were lower in grafted sites compared with sites left healed naturally. The bone healing density in grafted sites was statistically significantly higher that of sites healed naturally.
Conclusion: The application of autogenously tooth bone graft (Auto BTG) in to fresh extraction socket is efficient in preservation of alveolar ridge by minimizing vertical and horizontal ridge loss and promoting healing of bone for up to 4 months as shown radio graphically.
Keywords
Tooth extraction, Autogenously teeth, Alveolar ridge Preservation, CBCT imaging
Introduction
Tooth extraction is indicated when a tooth is nonrestorable or cannot be preserved in long extent of time in terms of aesthetics or functions [1]. Tooth extractions promote a sequence of effects that further cause reduction of height and width of alveolar ridge, especially in the buccal wall and horizontally [2-5]. The alveolar bone loss may occur up to first year post tooth extraction with two third of bone loss take placing with in the first three months of the healing period [6]. This may cause challenging in two situations: it can produce aesthetics complication in fabrication of fixed prosthesis and jeopardize the placement of dental implant and requiring Guided Bone Regeneration (GBR) [7].
To overcome this problem, the preservation of alveolar ridge in extraction socket is a fully explained surgical procedure to reduce bone resumption [8,9]. Various graft materials has been used in ARP including: auto graft, allograft, xenon graft and alloplastic materials.
Three main properties required for perfect bone graft materials: osteoconduction (the capability to supply scaffold for bone formation), osteoinduction (the ability of recruitment of bone forming cells and regeneration of bone from these cells), and osteogenesis (existence of cells that stimulate bone formation) [10,11]. For a long time, autogenously bone is extensively agreeable as the gold standard bone graft material due to its osteoconductivity, osteoinductvity, and osteogenecity characteristics, but it may have some complications such as morbidity of donor area and surgery, high rate of resumption and availability is limited [12].
Recently, all extracted teeth discarded as they are considered to be dental waste [13]. Human teeth could be processed to produce bone graft biomaterial that can ride the disadvantages of autogenously graft and other types of bone grafts [14]. Both dentin and alveolar bone have the same embryologic origin (same neural crest); this might exhibit ability of dentin for bone formation. Additionally, dentin and bone share the similar chemical composition [15]. With osteoinductive and osteoconductive matrix and for this reason is an applicable for bone grafting [16]. The first introduction of dentin graft was in 1967, in a study applied Decalcified Dentin Graft (DDG) in mandibular osseous defects and alveolar socket, the study revealed exact promising outcomes [17].
The present study explains a clinical method that uses freshly extracted teeth and processing them in to sterilized particles of autogenously mineralized dentin for immediate filling of socket. The extracted teeth were recycled in to dentin particulates by using smart dentin grinder device.
Material and Methods
Study design and ethical approval: This was split mouth prospective clinical study. All materials and procedures were submitted and approved by ethical committee of the collage of dentistry, university of Baghdad (protocol reference number 210120). All patients involved in this study were signed written informed consent before the start of study. The present study was conducted between December 2020 and August 2021.
Patient selection and treatment protocol: Twenty Patients with an overall of 40 extraction sockets were selected for this research from department of oral and maxillofacial surgery. These cases were divided in two groups, control group (20 extraction sockets left to heal by clot formation) and study group (20 extraction sockets grafted with autogenously teeth particulates). The patient involved the following inclusion criteria: older than 18 years, no history of any systemic or local conditions compromised healing of bone, the teeth without acute infection, and any bilateral compromised teeth in both upper or lower jaws included in study. Patients who were with history of radiotherapy to either maxilla or mandible, pregnant and lactating females, those on drug that interfere with bone healing such as corticosteroids or bisphosphonates, traumatic tooth extraction, endodontic treated teeth, and those incapable to return for follow up and study recall were excluded from the study. Oral panoramic radiograph, viral screens (HBS Ag, anti-HCV, HIV and COVID-19) were done preoperatively.
Surgical procedure: Under local anaesthesia (lidocaine hydrochloride 2% local anaesthetic carpels 1.8 ml with adrenaline 1:80,000) both study and control sides were extracted at the same visit.
Teeth extractions were carried out with the gentle application of an elevator and a forceps to reduce the amount of trauma to the surrounding bone and soft tissue. Flaps were not elevated. The sockets after extraction were debrided to eliminate granulation tissue then irrigated with saline solution.
Autogenously tooth bone graft was processed according to manufacture recommendations. Firstly, extracted teeth were mechanically cleaned by high speed fissure carbide bur. All caries, filling material, discoloured dentin, periodontal ligaments and calculus were removed before grinding. The clean tooth was dried well by air syringe and placed in the grinding chamber of smart dentin grinder unit (Kometa Bio Inc., Cresskill, NJ, USA). Then setting the grinding time to three seconds and sorting time to ten seconds. The particles extracted by pull out the upper drawer, which contains particles of between 300-1200 microns, Figure 1. The particles were placed in dentin cleanser for five minutes to dissolve bacteria and all organic remnants, and then dehydrated by using sterile gauze. Washing the particles by using phosphate buffered saline and left in solution for 3 min, then dehydrated by new sterile gauze. This process repeated again in order to neutralize level of PH. The particles were placed in the socket and condensing well to fill the socket completely, Figure 2. Finally, the margins of the socket approximated by continuous suturing technique. In control groups: the extraction sockets were debrided, irrigated by normal saline and sutured by using continuous suturing technique.
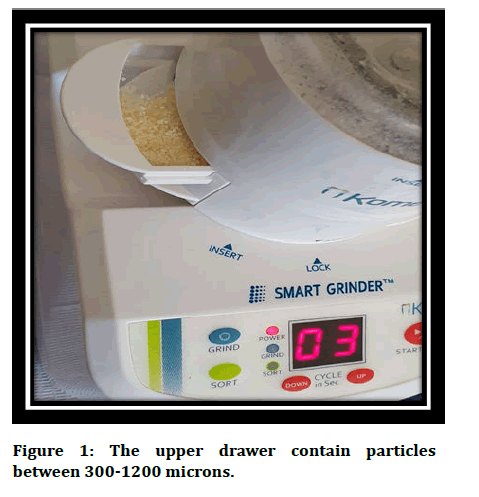
Figure 1: The upper drawer contain particles between 300-1200 microns.
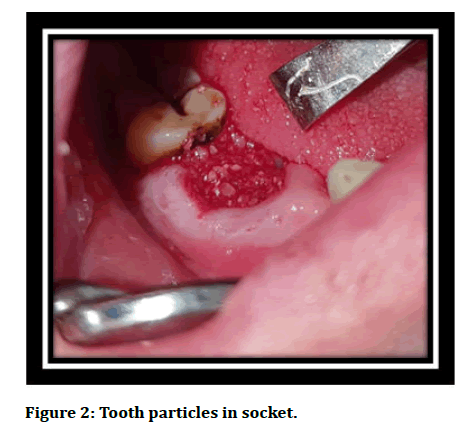
Figure 2: Tooth particles in socket.
Postoperative follow up and data collection
Clinical examination: All patients were attended after 7 days for suture removal and check-up healing, if there were any postoperative complication occurred.
Radiographic Assessment: Radiographic estimation was done by CBCT, set at 90 Kv, 9.2 mA and 8.1 s with (13 × Ø15) c FOV and 0.3 mm slice thickness, captured at two steps; first step 7 days after procedure as standard image, and second step after four months to be compared to the standard image, to estimate variations in width and height of ridge, variations in density of bone in the first week after extraction and after four months.
Measurement of ridge height and horizontal ridge width: The changes of radiographic alveolar bone of Horizontal Ridge Width (HRW), Buccal Bone Height (BBH), Lingual Bone Height (LBH) and Bone Density (BD) were estimated by external examiner on CBCT. The measurements were created at baseline image and after four months using the identical reference lines and points. To locate a reference, the most apical point of extraction socket and two reference lines were determined in baseline CBCT. The first line was drawn vertically from the apical reference point through the socket centre. The second line was drowning horizontally at most apical point of the extraction socket perpendicular to vertical line. Height of ridge was measured at mid buccal/labial and mid lingual/palatal aspects from most coronal area to apical reference point of socket parallel to vertical reference line, as seen in Figure 3. The Horizontal Ridge Width (HRW) was measured at the most coronal aspect of alveolar bone crest parallel to horizontal reference line.
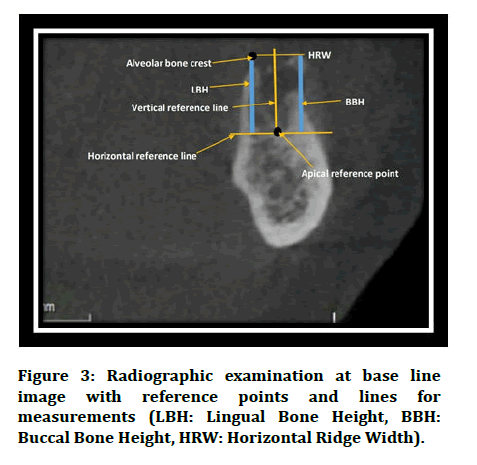
Figure 3: Radiographic examination at base line image with reference points and lines for measurements (LBH: Lingual Bone Height, BBH: Buccal Bone Height, HRW: Horizontal Ridge Width).
Statistical analysis
The statistical package for social science (SPSS Version 26) was used to analyse data. The paired t-test was used in measurements of vertical height, horizontal ridge width, and bone density changes. A level of P value <0.05 was considered significant.
Result
An overall of 40 extraction sockets (20 maxilla and 20 mandibles) from 20 participants 7 females, 17 males) age range (19 to 67 years) with the mean age (37.20 years) were involved in the study. The causes for tooth extraction were advance caries, tooth fracture after restoration and prosthodontics reasons. The sample is divided in tow groups control group extraction socket left heal normally without grafting and study group extraction socket grafted with Auto BTG.
On the 7th day follow up visit, satisfactory healing was showed in all patient at all grafted and non-grafted sites. All the sockets with Auto BTG were healed without any clinical manifestations of infection or graft rejection. After 4 months favourable healing was noticed in all patients. Clinically, the grafted sites exhibited less alveolar ridge width and height reduction compared with non-grafted sites as seen in Figure 4.
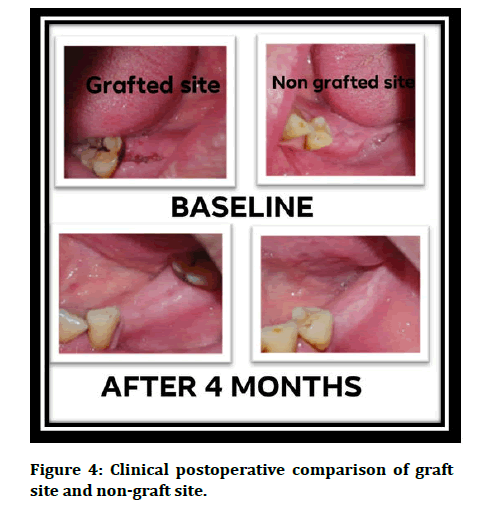
Figure 4: Clinical postoperative comparison of graft site and non-graft site.
Radiographic Analysis
Baseline CBCT was taken after one week of tooth extraction and 4 months postoperative image was taken for radiographic estimation, Figure 5. Mean baseline and 4 months alveolar ridge height and width and bone density are explained in Table 1 and Table 2.
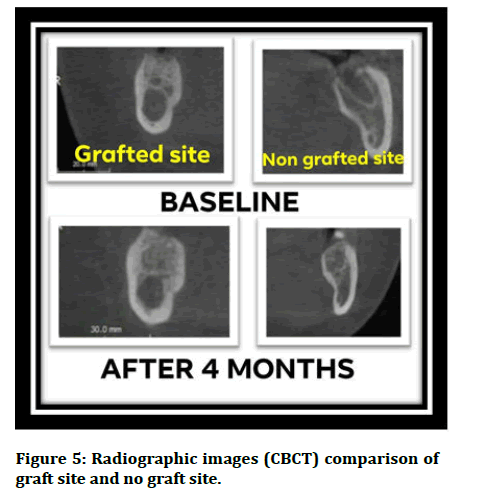
Figure 5: Radiographic images (CBCT) comparison of graft site and no graft site.
| Variables | Group type | No. of cases | Initial value | p value | Final value Mean mm ± SD | P value | P value |
|---|---|---|---|---|---|---|---|
| BBH | Control | 20 | 11.9 (0.9) | 0.7 | 11.4 (1.1) | 0.7 | 0 |
| BBH | Study | 20 | 11.8 (1.1) | 11.5 (1.1) | 0 | ||
| LBH | Control | 20 | 11.6 (1.0875) | 0.67 | 11.5 (1.0) | 0.97 | 0 |
| LBH | Study | 20 | 11.6 (1.1) | 11.5 (1.1) | 0 | ||
| HRW | Control | 20 | 8.8 (1.5) | 0.74 | 8.2 (1.6) | 0.77 | 0 |
| HRW | Study | 20 | 8.7 (1.7) | 8.4 (1.6) | 0 |
Abbreviations: BBH: Buccal Bone Height; LBH: Lingual Bone Height; HRW: Horizontal Ridge Width; SD: Standard Deviation; P: Probability; Sig: Significant p<0.05.
Table 1: The initial and final radiographic measurements of (buccal bone height, lingual bone height, and horizontal ridge width) in control and study group.
| Variables | Group type | No. of cases | Initial value Mean Hu ± SD |
p value | Final value Mean Hu ± SD | P value | P value |
|---|---|---|---|---|---|---|---|
| BD | Control | 20 | 122.6 (120.8) | 0 | 360.9 (123.9) | 0 | 0 |
| BD | Study | 20 | 459.6 (204.9) | 503.0 (120.9) | 0.32 |
Abbreviations: BD: Bone Density; SD: Standard Deviation; P: Probability; Hu: Hounsfield Unit; Sig: Significant p <0.05
Table 2: The initial and final radiographic measurements of bone density in control and study group
Dimensional changes
The losses in the vertical and horizontal dimensions of alveolar ridge were calculated by subtracting final measurements from baseline measurements and were explained in mm Table 3. The control group displayed losses of 0.7 mm and 0.3 mm, while the study group exhibited losses of 0.3 mm and 0.1 mm for BBH and LBH,respectively. In spite of the loss of vertical dimension in both groups, even so, the losses of Buccal Bone Height (BBH) and Lingual Bone Height (LBH) in non-grafted group were statically significant higher than in grafted group. Regarding the HRW loss, the control group showed a mean loss of 0.8 mm, while the study group showed a mean value of 0.3 mm. There was significant loss of Horizontal Ridge Width (HRW) in both groups but the rate of resumption was higher in control group compared with study group.
| Control group | Study group | P value | |
|---|---|---|---|
| Mean ± SD mm | Mean ± SD mm | ||
| BBH | 0.7 (0.3) | 0.3 (0.1) | 0 |
| LBH | 0.3 (0.2) | 0.1 (0.1) | 0 |
| HRW | 0.7 (0.3) | 0.3 (0.1) | 0 |
Abbreviations: BBH: Buccal Bone Height; LBH: Lingual Bone Height; HRW: Horizontal Ridge Width; SD: Standard Deviation; P: Probability
Table 3: The rate of change in BBH, LBH, HRW, BD post 4 months.
Bone density assessment
The Bone Density (BD) was measured by selecting five points inside the socket and read the Voxel Value (VV), these points include: Two points in top (coronally), at buccal and lingual aspects of the sockets, two points in the middle, at buccal and lingual aspects of the sockets and one point in most apical area of the socket. The mean of these five points of VV. number estimated to be dependent as mean bone density of the newly formed bone in the extraction socket. Throughout the 4 months period, the mean change of bone healing density (-238.6 ± 136.4) in control group was much lower than in study group (-43.5 ± 191.6). However, the outcomes were statically significant increase during 4 months (p<0.05).
Discussion
Preservation of alveolar ridge is a popular clinical procedure carried out to reduce resumption of alveolar ridge post tooth extraction to allow subsequently placement of implant or to maintain pontic area. Ideal properties of grafting materials are biocompatibility, osteoconductivity, osteoniductivity, and biodegradability that allow alveolar contour preservation, porosity and surface characteristics that encourage angiogenesis and lastly formation of bone. Additionally, the material should be cost effective and easy for chair side application [18].
When autogenously dentin is used in grafting, during regenerative time the formed new bone invested directly on the grafted surface will make a mineralized matrix association between present bone, new bone, and dentin particles (alkalosis) [6,19,20]. In this study, smart dentin grinder device (Kometa Bio Inc., Cresskill, NJ, USA) was used for processing extracted teeth.
In our study, the use of the autogenously tooth bone graft particles in the extraction socket showed being able to reduce the rate of resumption slightly of the vertical and horizontal dimensions in grafted sites when compared with non-grafted sites after four months of graft placement. Additionally, the density in extracted socket was higher in grafted sites than non-grafted sites.
Tooth graft was previously stated as bone substitute before implant installation [21,22]. After 4 months period, the extraction site filled with autogenously tooth bone graft demonstrating satisfactory ridge architecture and without signs of graft rejection. Regarding the use of autogenously tooth as bone substitutes, different studies have reported successful findings when use tooth particles as bone graft material for alveolar bone preservation. Concerning the outcomes of radiographic bone density, this study presented satisfactory results. Gomes, et al. stated that the healing process of the third molar socket grafted with Autogenously Demineralized Dentin Matrix (ADDM) coated with Polytetrafluoroethylene (PTFE) for 3 months. The healing process demonstrated that the healing better in ADDM+PTFE sockets than in non-grafted sockets [23]. The radiographic density of bone in the site was filled with ADDM similar to that of the adjacent natural bone on the 3 months.
The past study demonstrated that even with different ridge preservation procedures; there will finally some loss of bone [24]. Concerning the results of present study, the use of autogenously tooth bone graft could be to some extent preserve the dimensions of ridge post extraction, but it would lastly be undergo to some resumption as explained in previous researches.
Regarding the change rate of vertical dimension in this study after 4 months, the mean values of BBH and LBH loss were in non-grafted sites (0.7 ± 0.3 mm; 0.3 ± 0.2 mm, respectively). While in grafted sites the mean values of BBH and LBH loss were 0.3 ± 0.1 mm; 0.1 ± 0.1 mm, respectively. The rate of height loss was more in buccal/ labial aspect than lingual/palatal aspect in both groups. This probably refer to the higher percentage of loss prone bundle bone in buccal side, which in ordinary extraction may demonstrate some degree of bone defect. Our result show significant difference between grafted and non-grafted groups regarding the change rate of BBH and LBH. The results of this study corresponding to result of the study reported by Elfana, et al. who demonstrated no significant difference when used Autogenously Whole Tooth Graft (AWTG) and Autogenously Demineralized Dentin Graft (ADDG) for preservation of ridge, after 6 months the reduction was 0.61 ± 0.20 mm and 0.71 ± 0.27 mm in buccal ridge height and 0.66 ± 0.31 mm and 0.56 ± 0.24 mm in lingual bone height for AWTG and ADDG groups, respectively. In versus, other study revealed the vertical dimension was exhibited increase in vertical volume after 4 months of preservation with autogenously tooth derived particulate graft [25,26].
Concerning the change of horizontal dimension, our result showed loss of horizontal bone in grafted and nongrafted groups, the HRW reduction was 0.8 ± 0.3 mm and 0.3 ± 0.1 mm for control and study groups, respectively. There was significant difference between both groups. Similar to present study Valdec, et al. and Jung et al. reported in their researches the horizontal width reduction was 1.1 mm and 0.78 mm after 4 months of ridge preservation with tooth graft, respectively [27,28]. Joshi, et al. Conducted close outcomes to this study when compared between non-grafted sites, Beta-trialcium phosphate-grafted site, and autogenously tooth grafted site. They observed the mean horizontal change for autogenously tooth grafted sites was lesser statistically when compared to non-grafted sites and beta-tricalcium phosphate-grafted sites (0.15 ± 0.08 mm, 2.29 ± 0.40 mm, and 1.45 ± 0.40 mm, respectively) [29].
Clinical and histological study has provided evidence in support to the fact that ridge preservation techniques minimize the dimensional change of bone compared with extraction sites without ridge preservation techniques [30]. Nevertheless, systematic review establish, in spite of providing evidence based ridge preservation techniques, a totally prevention of horizontal and vertical bone loss is an unpredictable event. The outcomes of present study are in correspondence with these findings as there was some reduction of ridge height and width in study group although carried out ridge preservation procedure. Therefore, procedures of ridge preservation do not result in fully dimensional stability but are performed decrease resumption of alveolar ridge compared to sites left to heal naturally post extraction of tooth. In current study, with the change of horizontal and vertical dimension was less in the grafted group than non-grafted group after 4 months of ridge preservation. There was little increase of BD in study group along the study time. This little increase may be demonstrated by new bone formation with in particles of tooth graft and slow resumption proportion results in residual toot particles with high dentin density. This finding can interpret the statically significant difference in BD between control and study groups after 4 months. The split mouth design performed in this study had advantages of eliminating inter participant variability. In contribution to complications of this study, generally no intraoperative complications in this study. The healing process was satisfactory, all the sockets with Auto BTG were healed without any clinical manifestations of infection, graft rejection and wound dehiscence.
Conclusion
The application of autogenously tooth bone graft (Auto BTG) in to a fresh extraction socket is efficient in preservation of alveolar ridge by minimizing vertical and horizontal ridge loss and promoting healing of bone for up to 4 months as shown radio graphically.
References
- Juodzbalys G, Stumbras A, Goyushov S, et al. Morphological Classification of Extraction Sockets and Clinical Decision Tree for Socket Preservation/Augmentation after Tooth Extraction: a Systematic Review. J Oral Maxillofac Res 2019; 10:e3.
- Avila-Ortiz G, Chambrone L, Vignoletti F. Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis. J Clin Periodontol 2019; 46:195–223.
- Jambhekar S, Kernen F, Bidra AS. Clinical and histologic outcomes of socket grafting after flapless tooth extraction: A systematic review of randomized controlled clinical trials. J Prosthet Dent 2015; 113:371–382.
- Tan WL, Wong TLT, Wong MCM, et al. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res 2012; 23:1–21.
- Troiano G, Zhurakivska K, Lo Muzio L, et al. Combination of Bone Graft and Resorbable Membrane for Alveolar Ridge Preservation: A Systematic Review, Meta-analysis and Trial Sequential Analysis. J Periodontol 2017; 89:46–57.
- Pohl S, Binderman I, Tomac J. Maintenance of Alveolar Ridge Dimensions Utilizing an Extracted Tooth Dentin Particulate Autograft and PlateletRich Fibrin: A Retrospective Radiographic ConeBeam Computed Tomography Study. Materials 2020; 13:1083.
- Ramanauskaite A, Sahin D, Sader R, et al. Efficacy of autogenous teeth for the reconstruction of alveolar ridge deficiencies: A systematic review. Clin Oral Investig 2019; 23:4263–4287.
- Bassir S, Alhareky M, Wangsrimongkol B, et al. Systematic Review and Meta-Analysis of Hard Tissue Outcomes of Alveolar Ridge Preservation. Int J Oral Maxillo fac 2018; 33:979–994.
- Stumbras A, Kuliesius P, Januzis G, et al. Alveolar Ridge Preservation after Tooth Extraction Using Different Bone Graft Materials and Autologous Platelet Concentrates: A Systematic Review. J Oral Maxillofac Res 2019; 10:1–15.
- Gual-Vaques P, Polis-Yanes C, Estrugo-Devesa A, et al. Autogenous teeth used for bone grafting: A systematic review. Med Oral Patol Oral Cir Bucal 2018; 23:112–119.
- Albrektsson T, Johansson C. Osteoinduction, osteoconduction and osseointegration. Eur Spine J 2001; 10:S96–S101.
- Minetti E, Giacometti E, Gambardella U, et al. Socket Preservation with Different Autologous Graft Materials: Preliminary Results of a Multicenter Pilot Study in Human. Materials 2020; 13:1153.
- Dwivedi A, Kour M. A neoteric procedure for alveolar ridge preservation using autogenous fresh mineralized tooth graft prepared at chair side. J Oral Biol Craniofac Res 2020; 10:535-541.
- Kabir MA, Murata M, Shakya M, et al. Bio-Absorption of Human DentinDerived Biomaterial in Sheep CriticalSize Iliac Defects. Materials 2021; 14:223.
- Andrade C, Camino J, Nally M, et al. Combining autologous particulate dentin, L-PRF, and fibrinogen to create a matrix for predictable ridge preservation: a pilot clinical study. Clin Oral Investig 2020; 24:1151-1160.
- Kim YK, Lee J, Um IW, et al. Tooth-derived bone graft material. J Korean Assoc Oral Maxillofac Surg 2013; 39:103.
- Yeomans J, Urist M. Bone induction by decalcified dentine implanted into oral, osseous and muscle tissues. Arch Oral Biol 1967; 12:999-1008.
- Sanz M, Dahlin C, Apatzidou D, et al. Biomaterials and regenerative technologies used in bone regeneration in the craniomaxillofacial region: Consensus report of group 2 of the 15th European Workshop on Periodontology on Bone Regeneration. J Clin Periodontol 2019; 46:82–91.
- Binderman I, Bahar H, Yaffe A. Strain Relaxation of Fibroblasts in the Marginal Periodontium Is the Common Trigger for Alveolar Bone Resorption: A Novel Hypothesis. J Periodontol 2002; 73:1210–1215.
- Grado GFD, Keller L, Idoux-Gillet Y, et al. Bone substitutes: A review of their characteristics, clinical use, and perspectives for large bone defects management. J Tissue Eng 2018; 9:1–18.
- Chen ST, Wilson TG Jr, Hammerle CH. Immediate or early placement of implants following tooth extraction: Review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants 2004; 19:12-25.
- Ouyyamwongs W, Akarawatcharangura B, Suttapreyasri S. Demineralized tooth matrix used as a bone graft in ridge preservation: A case report. J Dent Assoc Thai 2017; 67:143–151.
- Gomes MF, Abreu PP, Morosolli AR. Densitometric analysis of the autogenous demineralized dentin matrix on the dental socket wound healing process in humans. Braz Oral Res 2006; 20:324–330.
- Ten Heggeler JM, Slot DE, Van der Weijden GA. Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: A systematic review. Clin Oral Implants Res 2011; 22:779–788.
- Elfana A, El-Kholy S, Saleh HA, et al. Alveolar ridge preservation using autogenous whole-tooth versus demineralized dentin grafts: A randomized controlled clinical trial. Clin Oral Implants Res 2021; 32:539-548.
- Radoczy-Drajko Z, Windisch P, Svidro E, et al. Radiographical and histological evaluation of alveolar ridge preservation with an autogenous tooth derived particulate graft in ED's class 3-4 defects. BMC Oral Health 2021; 21:63.
- Valdec S, Pasic P, Soltermann A. Alveolar ridge preservation with autologous particulated dentind A case series. Int J Implant Dent 2017; 3:12–21.
- Jung GU, Jeon TH, Kang MH, et al. Volumetric, radiographic, and histologic analyses of demineralized dentin matrix combined with recombinant human bone morphogenetic protein-2 for ridge preservation: a prospective randomized controlled trial in comparison with xenograft. Appl Sci 2018; 8:1288.
- Joshi CP, Dani NH, Khedkar SU. Alveolar ridge preservation using autogenous tooth graft versus beta-tricalcium phosphate alloplast: A randomized, controlled, prospective, clinical pilot study. J Indian Soc Periodontol 2016; 20:429-434.
- Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: A clinical and histologic study in humans. J Periodontol 2003; 74:990–999.
Author Info
Farah Abid Yousif* and Saif Saadedeen Abdulrazaq
Department of Oral and Maxillofacial Surgery, Dental Teaching Hospital, College of Dentistry, University of Baghdad, Bab-Almoadham, Baghdad, IraqCitation: Farah Abid Yousif, Saif Saadedeen Abdulrazaq, Processing the Extracted Tooth to Graft the Fresh Socket (Split Mouth Prospective Clinical Study), J Res Med Dent Sci, 2022, 10 (10): 079-085.
Received: 02-Aug-2022, Manuscript No. JRMDS-22-54337; , Pre QC No. JRMDS-22-54337(PQ); Editor assigned: 04-Aug-2022, Pre QC No. JRMDS-22-54337(PQ); Reviewed: 18-Aug-2022, QC No. JRMDS-22-54337; Revised: 06-Oct-2022, Manuscript No. JRMDS-22-54337(R); Published: 18-Oct-2022
