Research - (2022) Volume 10, Issue 1
Prevalence of Type of Sublingual Concavity and its Correlation with the Visibility of Mandibular Canal in Panoramic View in South Indian Population-A CBCT Study
Gaurav N Ketkar1, Sankari Malaiappan* and Rajeshkumar S
*Correspondence: Sankari Malaiappan, Department of Periodontics, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Chennai, India, Email:
Abstract
Background: Sound anatomic knowledge and thorough treatment planning is necessary to avoid complications in the surgical field. With the help of the recent advances in radiographic 3D imaging (Cone Beam Computed Tomography-CBCT) it is possible to plan and carry out the intended treatment with minimal possibility of risks. Aim: The present study was aimed at assessing the lingual concavities in the submandibular fossa region also the location of mandibular canal in patients requiring dental implants with the help of cone beam computed tomography (CBCT) and to correlate it with the visibility of the mandibular canal (MC) in the panoramic view. Material and methods: 200 CBCT scans and panoramic radiographs were evaluated. SF depth types were classified as type I (0-1mm); type II (2-3mm) and type III (>3mm) on CBCT. Visibility of SF and the cortication of MC on panoramic radiographs were compared with the depth of SF on CBCT. Distances between MC and mandibular inferior, buccal, and lingual cortices were measured. Results: Sixty two percent of the selected population fell under the type II group, whereas 31% and 6% under type I and type III groups respectively. Conclusion: Within the limits of the study, it can be concluded that implant placement can be done with minimal risk of perforation in the mandibular posterior region in the selected population. No significant correlation was found between visibility of the MC in panoramic view and the type of sublingual concavity. A marked radiolucent submandibular fossa on a panoramic image does not undoubtedly indicate a deep fossa, which emphasizes the importance of 3-D imaging in implant planning.
Keywords
CBCT, Sublingual concavity, Mandibular canal, Implants
Introduction
Dental implants are replacement tooth roots. Implants provide a strong foundation for fixed (permanent) or removable replacement teeth that are made to match your natural teeth. Accurate determination of anatomical landmarks during the treatment plan is crucial for the clinician to avoid surgical complications. Among these structures, the location of submandibular fossa (SF) and mandibular canal (MC) must be thoroughly evaluated by the clinicians before implant placement in the mandible. Severe haemorrhage and subsequent hematoma which have life-threatening consequences due to upper airway obstruction are few of the major complications faced following the perforations and damage to the sublingual concavity [1,2]. Paraesthesia and permanent nerve injury are one of the important consequences of the improperly administered inferior alveolar nerve blocks [3]. To avoid these complications clinicals are forced to place shorter implants in improper angulations due to inadequate anatomical knowledge and lack of accessibility to modern diagnostic tools. Thus, a comprehensive preoperative treatment planning including three-dimensional radiographic examination is essential for implant placement in appropriate position with optimal length and width to obtain favourable surgical and prosthetic outcomes.
As a fundamental principle of diagnostic radiology, the patients must be exposed to as low as reasonably achievable (ALARA) radiation. High levels of radiation exposure are the foremost disadvantage of CT scans. Guidelines published by European Association for Osseointegration, states that medical exposure to ionizing radiation must always be justified and results in a net benefit to the patient [4]. hence only cases with high chances of complications without a 3D imaging should be referred for the 3D imaging. CBCT is an excellent alternative to minimise the radiation exposure of the patient.
Previous periodontal disease or atrophy due to long-term non-function can cause changes in the mandibular dimensions, the availability of the bone and location of the canal with respect to the alveolar crest. Correlation between the concavity type, MC location and visibility on the panoramic image will help the clinician to accurately diagnose and to decide whether 3D imaging is a necessity in a particular case [5,6].
Cone beam computed tomography (CBCT) has been suggested as the golden standard for evaluation of alveolar bone, since it allows three-dimensional analysis of investigated regions with high accuracy by providing high-quality images with submillimetre resolution and a low radiation dose [7].
The present study was aimed at assessing the lingual concavities in the submandibular fossa region also the location of mandibular canal in patients requiring dental implants with the help of cone beam computed tomography (CBCT) and to correlate it with the visibility of the mandibular canal (MC) in the panoramic view.
Materials and Methods
This prospective radiographic study was performed at the outpatient department of periodontology and implantology of Saveetha institute of Medical and technical sciences from October 2020 to April 2021. The study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013. Ethical clearance was obtained from the Institutional Review Board (IHEC/SDC/PERIO-1901/21/43), and Informed consent was obtained from the study participants. Sample size was determined using the mean and standard deviation values of previous study, at a power of 90% (G power 3.0 software). A total of 200 CBCT scans of patients who were indicated for implant surgery were chosen and assessed.
The exclusion criteria included CBCT scans showing congenital and/or developmental disorders, abnormal morphology resulting from trauma and pathologic conditions which potentially affected the area of interest and panoramic radiographs with image deformity and displaying obvious dental pathology affecting the area of interest.
Radiographic examination
A CBCT scanner with a flat panel detector was used in all cases (CS 9600 Carestream flat panel detector) with an exposure volume set at 102 mm diameter and 102 mm height. Manufacturer recommended settings of 120 kV and 6.3 mA were employed with an exposure of 796 mGy/cm2 for 15 seconds. DICOM files of the axial images were imported and analyzed using the planning provided by the same company software 3D Image Light Carestream and Galileos by Serona. All the measurements were taken in the 2nd molar region on the right and left side. The deepest part of the SF was determined from cross-sectional images and used for measurements. A line was placed on the most prominent superior and inferior points of the lingual concavity, and a second line was drawn from the deepest point of the concavity perpendicular to the first line. SF types were classified as: Type I, a flat impression <1 mm deep; Type II, a 2 to 3 mm concavity; and Type III, a concavity >3 mm (Figure 1). Visibility of the MC was checked in panoramic view for the same patient as shown in the figure. Panoramic interpretations were made based on the presence and absence of an apparent radiolucency indicating the visibility of sublingual fossa (SF) and the cortication of MC in the SF region. These data were then compared with the depth of SF in CBCT. Two independent investigators (A and B) performed the computerised tomographic assessment of Alveolar antral anastomosis. The measurement was further cross checked by a senior periodontist (C).
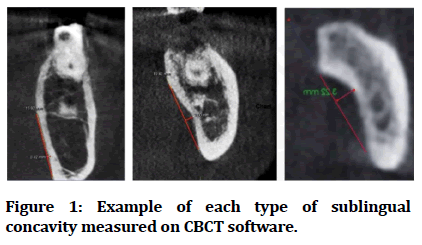
Figure 1: Example of each type of sublingual concavity measured on CBCT software.
Statistical analysis
Data analysis of measurements from CBCT scans of 200 patients was performed using the SPSS software version 21. Two-way mixed ANOVA was used to model side (left/ right), measurement type (depth), and gender, with side and type taken as within-subject variables, gender as between-subject variables. Differences between two independent groups were evaluated by Student t test. The Type-I error rate was set at a=0.05.
Results
As seen in Table 1 the mean depth of the sub mandibular fossa on right side and left side was found to be 1.7 and 1.8 mm respectively. The mean distance of the mandibular canal (MC) was minimum from the lingual border suggesting the lingual route of the mandibular canal (MC) (table 1). Table 2 denotes the distribution of the included individuals over the three groups which was 32%, 62% and 6% in type 1, type 2 and type 3 respectively (Table 2). No correlation was found in the sex and the type of concavity in the individuals (Table 3). Weak positive correlation was found when type of concavity was correlated with the complete canal visibility in panoramic view (Figure 2).
| Sr. Number | Measurement | Mean ± Standard deviation (mm) |
|---|---|---|
| 1 | Mean depth of SF right side | 1.73 ± 0.89 |
| 2 | Mean depth of SF left side | 1.81 ± 0.88 |
| 3 | Mean distance of MC from buccal cortical plate | 5.16 ± 0.22 |
| 4 | Mean distance of MC from lingual cortical plate | 1.26 ± 0.17 |
| 5 | Mean distance of MC from inferior cortical border | 5.32 ± 0.61 |
| Where SF- submandibular fossa; MC- mandibular canal | ||
Table 1: Showing mean and standard deviation of submandibular fossa (SF) right side, left side. Average distance of mandibular canal from buccal, lingual and inferior border.
| Sr. Number | Type of sublingual fossa | Frequency of cases | Percentage (%) |
|---|---|---|---|
| 1 | Type 1 (0-1mm) | 64 | 32% |
| 2 | Type 2 (2-3mm) | 124 | 62% |
| 3 | Type 3 (>3mm) | 12 | 6% |
Table 2:Showing frequency of the occurrence of type of concavity (SF) in the selected population.
| Sex | Total | |||||
|---|---|---|---|---|---|---|
| Male | Female | |||||
| Type of concavity | Type 1 (0-1mm) | 40 | 24 | 64 | 82 | 200 |
| Type 2 (2-3mm) | 72 | 52 | 124 | |||
| Type 3 (>3mm) | 6 | 6 | 12 | |||
| Total | 118 | |||||
Table 3: showing the distribution of the type of concavity in the males and females.
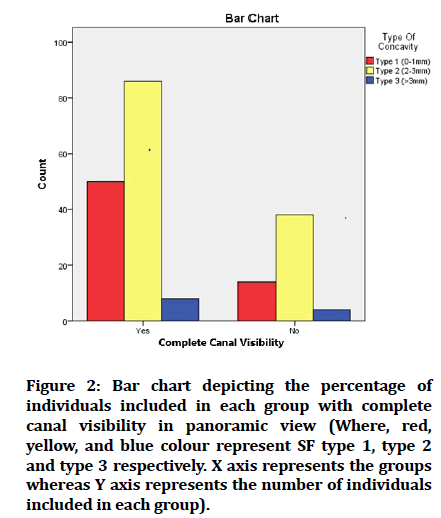
Figure 2: Bar chart depicting the percentage of individuals included in each group with complete canal visibility in panoramic view (Where, red, yellow, and blue colour represent SF type 1, type 2 and type 3 respectively. X axis represents the groups whereas Y axis represents the number of individuals included in each group).
Average distance of mandibular canal from buccal, lingual and inferior border.
Discussion
Aims of the study were to
To determine possible association between the visibility of SF and mandibular canal cortication on panoramic radiographs and SF depth on CBCT
To assess the possible correlations between the depth of SF and the vertical-horizontal locations of the MC.
Although panoramic radiographs are the most used and relied upon imaging modality by clinicians and their relatively low cost and widespread availability, there are inherent fundamental limitations due to its modality such as superimpositions, magnifications, distortions and low image quality. Further it is difficult to interpret 3D structures on a 2-dimensional radiograph [8,9].
The blood supply of the premolar–molar region that originates from submental artery and mylohyoid artery. Major bleeding during implant surgery can occur if these structures are damaged. The mylohyoid artery runs on the medial surface of the mandible in the mylohyoid
groove and continues supplying the mylohyoid muscle. The mylohyoid branch of the inferior alveolar artery can be injured after perforating the mandibular lingual cortex in the molar region [10–12].
The mandibular canal detection of the panoramic view depends highly on the modality and skill of the operator a weak correlation was expected. Study done by Olivera- Santos et al states that the trabecular pattern in the SF region hampers the visibility of the MC in the SF region [13,14]. In assessing the relation between the depth of the submandibular fossa, the visibility of the SF and mandibular canal on panoramic images, we found only a weak positive correlation, a deeper submandibular fossa did not yield the way for better visibility of the mandibular canal and the fossa on panoramic images. Race and gender do not seem to influence the position of the mandibular canal in the bucco-lingual plane [15].
Souza et al stated that the depth of the SF reaches its maximum in the second molar on both sides and it decreases in mesial and distal directions to reach the minimum depth in the area of the second premolar, our results are consistent with the findings of his study7. Hence, we can say that the risk of perforation of the mandibular canal in the premolar area is much lesser than that of the molar area. Our study also showed that the mandibular canal takes a lingual route (more closer to the lingual cortical plate. These results were contradictory to the results found by Kawashima et al [16], which stated that the mandibular canal takes a more buccal route. As we know, the last phase of growth of the body of the mandible is in the vertical direction. Hence the distance of MC from the inferior border was seen more in younger patients than in older patients. This can be attributed to the vertical growth of the mandible which is the last spurt in the mandibular growth also minimal vertical resorption in younger patients.
When a deep undercut is present, the lingual plate may be perforated resulting in hemorrhage during implant surgery, therefore, the angulation of the implant should accommodate the undercut [17]. Previously published study state that lingual concavity was present in 36–39 % of the cases, depth of the SF was more than 2 mm (Type 2 and Type 3 fossa) in 80 % of the study population [11,18]. Hence a sound knowledge of the vital structures is necessary to avoid any complication in the implant placement. Also, clinician should be well equipped to make the decision whether a 3D imaging is required for a particular case where possibility of complications might be higher [19].
The present study focussed on the Dravidian population. To the best of the author’s knowledge, no previous study evaluated the location of AAA in the Dravidian population. The Dravidian ethnicity comprises the people (Tamil, Malayalam, Telugu, and Kannada) in the southern part of India. The Dravidian race has distinct anatomic variations among the populations of Indian subcontinent and other populations [20,21]. In this study, we have included only the patients who had the above mentioned.
Languages as their mother tongue
Our study results are like the results of the study done by Ramaswamy et al which shows significantly deeper concavities in males. These results can be attributed to the similar ethnicity of the samples [22]. Recent advances in the implantology have suggested the use of a 3D guide to further minimise the chances of complications.
Conclusion
Within the limits of the study, it can be concluded that most of the South Indian population falls under the type I-II category where dental implants can be placed with minimal risk of complications. Patient age must be taken in consideration when planning for any dental implant procedure. It is always better to get a CBCT done when the possibility of complications is higher.
Acknowledgement
We would like to thank our director of Saveetha university dental college for his support and contribution during the period of the study.
Conflict of Interest
Author does not have any conflicts to declare.
References
- Niamtu J. Near-fatal airway obstruction after routine implant placement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92:597â??600.
- Isaacson TJ. Sublingual hematoma formation during immediate placement of mandibular endosseous implants. J Am Dent Assoc 2004; 135:168â??72.
- Dao TT, Mellor A. Sensory disturbances associated with implant surgery. Int J Prosthodont 1998; 11:462â??9.
- Jacobs R, van Steenberghe D. Radiographic planning and assessment of endosseous oral implants. Springer Sci Business Media 2012; 115.
- Weinstein GM, Zientz MT. The dental reference manual: A daily guide for students and practitioners. Springer 2016; 530.
- Bayrak S, Demirturk-Kocasarac H, Yaprak E, et al. Correlation between the visibility of submandibular fossa and mandibular canal cortication on panoramic radiographs and submandibular fossa depth on CBCT. Med Oral Patol Oral Cir Bucal 2018; 23:e105â??11.
- de Souza LA, Souza Picorelli Assis NM, Ribeiro RA, et al. Assessment of mandibular posterior regional landmarks using cone-beam computed tomography in dental implant surgery. Ann Anat. 2016; 205:53â??59.
- von Arx T, Bornstein MM. The bifid mandibular canal in three-dimensional radiography: morphologic and quantitative characteristics. Swiss Dent J 2021; 131:10â??28.
- y Baena RR, Beltrami R, Tagliabo A, et al. Differences between panoramic and Cone Beam-CT in the surgical evaluation of lower third molars. J Clin Exp Dent 2017; 9:e259â??65.
- Flanagan D. Important arterial supply of the mandible, control of an arterial hemorrhage, and report of a hemorrhagic incident. J Oral Implantol 2003; 29:165â??73.
- Watanabe H, Mohammad Abdul M, Kurabayashi T, et al. Mandible size and morphology determined with CT on a premise of dental implant operation. Surg Radiol Anat 2010; 32:343â??9.
- Dubois L, de Lange J, Baas E, et al. Excessive bleeding in the floor of the mouth after endosseus implant placement: A report of two cases. Int J Oral Maxillofac Surg 2010; 39:412â??5.
- de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investigation 2012; 16:387-93.
- Do Nascimento EH, dos Anjos Pontual ML, dos Anjos Pontual A, et al. Assessment of the anterior loop of the mandibular canal: A study using cone-beam computed tomography. Imaging Sci Dent 2016; 46:69-75.
- Tsakiris P, Kramer B, Lownie JF. A radiographic analysis of the mandibular canal of the edentulous mandible in different racial and gender groups. J Dent Assoc S Afr 1996; 51:759â??65.
- Kawashima Y, Sakai O, Shosho D, et al. Proximity of the mandibular canal to teeth and cortical bone. J Endod 2016; 42:221-4.
- Greenstein G, Cavallaro J, Tarnow D. Practical application of anatomy for the dental implant surgeon. J Periodontol 2008; 79:1833â??46.
- Parnia F, Fard EM, Mahboub F, et al. Tomographic volume evaluation of submandibular fossa in patients requiring dental implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont 2010; 109:e32-6.
- Jacobs R, Salmon B, Codari M, et al. Cone beam computed tomography in implant dentistry: Recommendations for clinical use. BMC Oral Health 2018; 18:88.
- Garn SM, Coon CS. On the number of races of mankind. Am Anthropol 1955; 57:996-1001.
- Jorde LB, Wooding SP. Genetic variation, classification and 'race'. Nat Genet 2004; 36:S28-33.
- Ramaswamy P, Saikiran C, Mrudula Raju B, et al. Evaluation of the depth of submandibular gland fossa and its correlation with mandibular canal in vertical and horizontal locations using CBCT. J Indian Academy Oral Med Radiol 2020; 32:22.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Gaurav N Ketkar1, Sankari Malaiappan* and Rajeshkumar S
1Department of Periodontics, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Chennai, India2Department of Pharmacology, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Chennai, India
Citation: Gaurav N Ketkar, Sankari Malaiappan, Rajeshkumar S, Prevalence of Type of Sublingual Concavity and its Correlation with the Visibility of Mandibular Canal in Panoramic View in South Indian Population-A CBCT Study, J Res Med Dent Sci, 2022, 10(1): 232-236
Received: 21-Dec-2021, Manuscript No. Jrmds-21-44368; , Pre QC No. Jrmds-21-44368 (PQ);; Editor assigned: 23-Dec-2021, Pre QC No. Jrmds-21-44368 (PQ);; Reviewed: 06-Jan-2022, QC No. Jrmds-21-44368; Revised: 10-Jan-2022, Manuscript No. Jrmds-21-44368 (R);; Published: 17-Jan-2022
