Research - (2020) Advances in Dental Surgery
Prevalence of Temporomandibular Joint Disorders in Patients with Impacted Teeth: An Institutional Study
Keerthika S and Santhosh Kumar MP*
*Correspondence: Santhosh Kumar MP, Department of Oral and Maxillofacial Surgery, Saveetha Dental COLLEGE and Hospitals, Saveetha Institute of Medical and Technical Science, Saveetha University, Chennai, India, Email:
Abstract
Temporomandibular joint (TMJ) is one of the structures of the stomatognathic system. Temporomandibular joint is a ginglymoarthrodial joint composed of synovial cavity, articular cartilage and a capsule that covers the same joint. Temporomandibular joint disorder (TMD) has multifactorial etiology, and the commonly reported ones are emotional tension, occlusal interference, teeth loss, postural deviation, masticatory muscular dysfunction, internal and external changes in Temporomandibular structures. Removal of the third molars has been propounded as a factor with the potential to damage TMJ. Trauma resulting from the surgery of third molars has been reported to be a predisposing factor in the progression of TMD symptoms. The aim of this study was to assess the prevalence of TMJ disorders in patients with impacted teeth. A prospective study was conducted in the department of oral and maxillofacial surgery in Saveetha Dental College and Hospital from October 2019-December 2019. The study population included 28 patients with impacted teeth and 28 patients without impacted teeth. Thus, the sample size included a total of 56 patients who were evaluated for the presence of clinical findings of TMD. Data was collected and statistical analysis was performed. Microsoft Excel 2016 (Microsoft office 10) data spreadsheet was used to collect data and later exported to SPSS IBM (version 23.0). Descriptive statistics and chi square test were employed with a level of significance set at p<0.05. In the current study out of 56 patients, it was seen that the symptoms of Temporomandibular joint disorders were more prevalent in female patients (58.06%). Clicking sound of TMJ was more prevalent in patients without impaction (56.52%) when compared to patients with impaction (43.48%). Association between clinical findings of TMD and impacted teeth was statistically not significant. p value=0.273. Within the limits of the study, temporomandibular joint disorders were present both in patients with and without impacted teeth, and impacted teeth had no significant influence on the development of temporomandibular Joint disorders.
Keywords
Associated factors, Chewing, Pain, Quality of life, TMD, impacted teeth, Clicking, Trismus
Introduction
Temporomandibular joint (TMJ) is one of the structures of the stomatognathic system [1,2]. Temporomandibular joint is a ginglymoarthrodial joint composed of synovial cavity, articular cartilage and a capsule that covers the same joint [3]. Through its complex movements on different orthogonal planes and multiple rotation axes it coordinates various functions such as mouth opening, swallowing, breathing and various facial expressions along with dental structures including mandible, muscle tenons, salivary glands etc. [4-7]. Temporomandibular joint disorders (TMD) are a class of degenerative musculoskeletal conditions associated with morphological and functional deformity [8]. This condition commonly comprises issues such as masticatory muscle fatigue, impaired jaw movements and articular sounds [9,10]. Temporomandibular joint disorder has multifactorial etiology, and the commonly reported ones are emotional tension, occlusal interference, teeth loss, postural deviation, masticatory muscular dysfunction, internal and external changes in Temporomandibular structures etc. [11,12].
Dental impaction refers to a tooth that resides totally or partially embedded (unerupted) in the bone of jaw or under gingival tissue. Different etiology of impaction includes insufficient space for eruption, defects, pathologies, and trauma. The most common dental impactions reported were third molars. Removal of the third molars has been propounded as a factor with the potential to damage TMJ [13]. Trauma resulting from the surgery of third molars has been reported to be a predisposing factor in the progression of TMD symptoms. The reason is that the process of removing the third molars involves extensive mouth opening for a long time and exertion of considerable forces to the mandible [14]. Each of these factors contributes to the development of muscular and articular pains due to the stretching muscles and ligaments, subluxation of the condyle, and disc dislocation [15]. De Angelis et al. suggested that TMD symptoms are common in patients who were referred to the wisdom tooth extraction [9]. Due to the limited studies on the relationship between extracting the third molars and incidence of TMD, the present study was conducted with the aim of determining prevalence of TMJ disorders in patients with impacted teeth. With a rich case bank established over 3 decades we have been able to publish extensively in our domain [16-25]. Based on this inspiration we aim to assess prevalence of TMJ disorders in patients with impacted teeth.
Materials and Methods
Study design and study setting
This prospective study was conducted in Saveetha dental college and hospital, Saveetha university, Chennai, to evaluate the prevalence of temporomandibular disorders in patients with impacted teeth among dental patients reporting to the outpatient department of oral and maxillofacial surgery from October 2019 to December 2019. The study was initiated after approval from the institutional review board of the University.
Study population and sampling
Inclusion criteria for the study was adult patients with and without impacted teeth. 56 patients were included in the study by a simple random sampling method to minimize sampling bias. These included 28 patients with impacted teeth, and 28 patients without impacted teeth. All missing or incomplete data, and medically compromised patients were excluded from the study.
Data collection and tabulation
Relevant data such as patients name, age, sex, clinical features such as clicking, pain on palpation and maximum mouth opening were recorded according to RDC-TMD criteria for clinical assessment of TMD. Presence and absence of impacted third molars was also recorded by clinical and radiographic evaluation. Data was verified by an external reviewer.
Statistical analysis
The collected data was validated, tabulated and analysed with Statistical Package for Social Sciences for Windows, version 23.0 (SPSS Inc., Chicago, IL, USA) and results were obtained. Descriptive analysis was done to assess the prevalence of TMD among gender and in patients with and without impacted teeth. Chi-square test was used to test association between impacted teeth and clinical findings of TMD. P value < 0.05 was considered statistically significant.
Results and Discussion
In the current study out of 56 patients, twentyeight patients had impacted teeth and in twentyeight patients there were no impacted teeth and they were evaluated for the presence of clinical findings of TMD. It was observed that TMD were present among all the patients in our study population. It was seen that the symptoms of Temporomandibular joint disorders are more prevalent in female patients (58.06%) when compared to male patients (41.9%) (Figure 1).
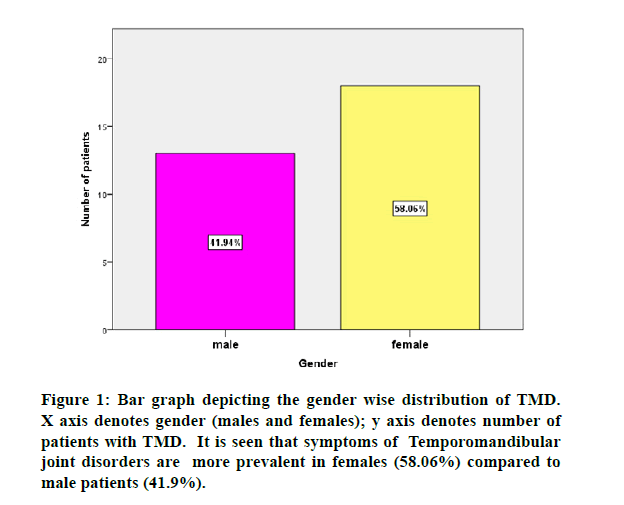
Figure 1: Bar graph depicting the gender wise distribution of TMD. X axis denotes gender (males and females); y axis denotes number of patients with TMD. It is seen that symptoms of Temporomandibular joint disorders are more prevalent in females (58.06%) compared to male patients (41.9%).
In relation to prevalence of clicking sound in TMJ among the study population, it was seen that clicking is more prevalent in patients without impaction (56.52%) when compared to patients with impaction (43.48%) (Figure 2).
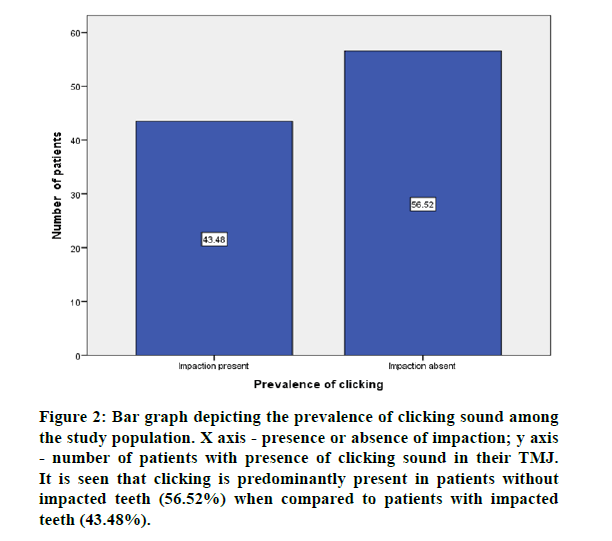
Figure 2: Bar graph depicting the prevalence of clicking sound among the study population. X axis - presence or absence of impaction; y axis - number of patients with presence of clicking sound in their TMJ. It is seen that clicking is predominantly present in patients without impacted teeth (56.52%) when compared to patients with impacted teeth (43.48%).
It was observed that equal prevalence of pain on palpation in TMJ was present in patients with (50%) and without impaction (50%) (Figure 3).
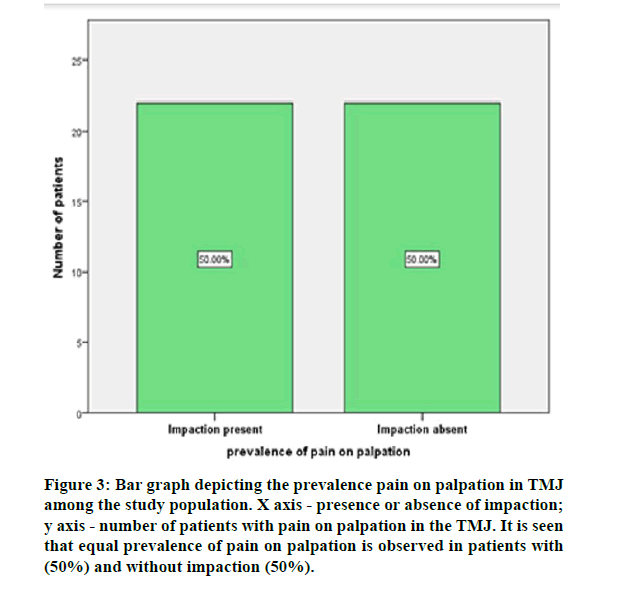
Figure 3: Bar graph depicting the prevalence pain on palpation in TMJ among the study population. X axis - presence or absence of impaction; y axis - number of patients with pain on palpation in the TMJ. It is seen that equal prevalence of pain on palpation is observed in patients with (50%) and without impaction (50%).
In relation to prevalence of restricted mouth opening among the study population, it was observed that restriction in mouth opening was predominantly present in patients with impaction (53.85%) than in patients without impaction (46.15%) (Figure 4).
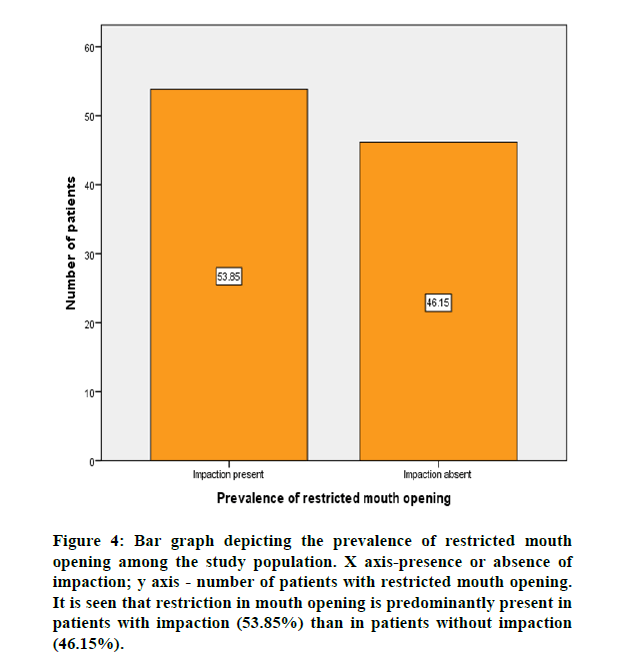
Figure 4: Bar graph depicting the prevalence of restricted mouth opening among the study population. X axis-presence or absence of impaction; y axis - number of patients with restricted mouth opening. It is seen that restriction in mouth opening is predominantly present in patients with impaction (53.85%) than in patients without impaction (46.15%).
On evaluating the association between clinical findings of TMD and impaction teeth, the results were statistically not significant. Pearson Chisquare=2.594, p value=0.273 (>0.05). Among patients with impaction 25% had clicking, followed by pain on palpation (50%) and restricted mouth opening (66.67%). Among patients without impaction 75% had clicking, followed by pain on palpation (50%) and restricted mouth opening (33.33%) (Figure 5). Thus, clinical findings of TMD were present both in patients with and without impaction and the results were statistically not significant.
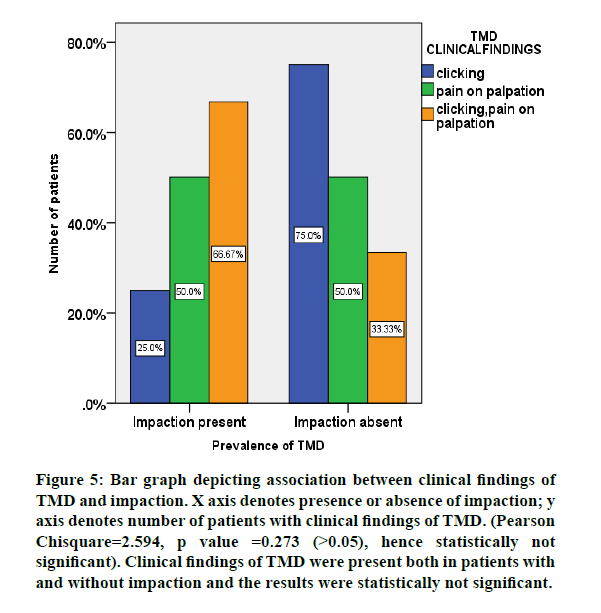
Figure 5: Bar graph depicting association between clinical findings of TMD and impaction. X axis denotes presence or absence of impaction; y axis denotes number of patients with clinical findings of TMD. (Pearson Chisquare=2.594, p value =0.273 (>0.05), hence statistically not significant). Clinical findings of TMD were present both in patients with and without impaction and the results were statistically not significant.
In the current study it is seen that clicking is more prevalent in patients without impaction (56.52%) when compared to patients with impaction (43.48%). This is supported in a study by Barbosa that investigated the relationship between TMD and surgery of third molars and indicated that the experience of third molars removal is associated with the joint click and limited opening of the mouth [26]. Furthermore, in a cross-sectional study, a relationship was observed between TMD symptoms and a history of third molar extraction [27]. However, in a prospective study, no difference was found between the click before and after third molar surgery.
On the contrary, Kurita et al. stated that the presence or absence of clicking should not be the unique factor considered during the diagnosis of disk displacement with and without reduction and additional examinations as MRIs are needed to get a precise diagnosis. Also, it was found that the presence of impacted third molars had no significant effect on the development of TMJ clicking or sounds. Thus, according to this study, the impacted third molar was considered a nonexacerbated factor in the occurrence of TMJ clicking. This may be because of the possibility that there were other factors in addition to the impacted third molars may be responsible for the development of TMJ sounds or clicking in spite of the detection of some cases with TMJ clicking.
Importance of performing less traumatic surgery has been emphasized to reduce the risk of joint and muscle problems. Based on the results of the present study, TMD had a higher prevalence among the females. Grossi et al reported that gender was one of the predictive factors of postoperative complaints [28]. To determine the causal relations between the extraction of third molars and incidence of TMD, diagnosis of TMD cases should be done before the third molar surgery. In this study, it was performed through clinical examinations. However, it was recommended that use of clinical examinations and RDC-TMD questionnaire concurrently for efficient diagnosis and treatment planning [29]. The limitations of the study include small sample size, single-centered study, and examiner’s subjectivity. The future scope of study is to do extensive research and to achieve successful diagnosis and treatment outcomes.
Conclusion
Within the limits of the study, temporomandibular joint disorders were present both in patients with and without impacted teeth, and impacted teeth had no significant influence on the development of temporomandibular Joint disorders.
Acknowledgement
I wish to express my deep sense of gratitude and professional thanks to my research guide Dr. Santhosh Kumar, Department of Oral and Maxillofacial Surgery, Saveetha Dental College and my college management for their keen interest, inspiring guidance, constant encouragement with my work during all stages to complete this study.
References
- Bender ME, Lipin RB, Goudy SL. Development of the pediatric temporomandibular joint. Oral Maxillofac Surg Clin North Am 2018; 3:1–9.
- Venugopal A, Maheswari TNU. Expression of matrix metalloproteinase-9 in oral potentially malignant disorders: A systematic review. J Oral Maxillofac Pathol 2016; 20:474.
- Juhl GI, Jensen TS, Norholt SE, et al. Incidence of symptoms and signs of TMD following third molar surgery: A controlled, prospective study. J Oral Rehab 2009; 36:199–209.
- Cuccia AM, Caradonna C, Caradonna D. Manual therapy of the mandibular accessory ligaments for the management of temporomandibular joint disorders. J Am Osteo Assoc 2011; 111:102–112.
- Varol A, Sencimen M, Gulses A, et al. Diagnostic importance of MRI and CT scans for synovial osteochondromatosis of the temporomandibular joint. J Craniomandibular Practice 2011; 29:313–317.
- Chaitanya NC, Muthukrishnan A, Babu DB, et al. Role of vitamin E and vitamin A in oral mucositis induced by cancer chemo/radiotherapy- A meta-analysis. J Clin Diagnostic Res 2017; 11:ZE06–ZE09.
- Subashri A, Uma Maheshwari TN. Knowledge, and attitude of oral hygiene practice among dental students. Res J Pharm Technol 2016; 9:1840-1842.
- Alamoudi N. Correlation between oral parafunction and temporomandibular disorders and emotional status among saudi children. J Clin Pediatr Dent 2001; 26:71–80.
- DeAngelis AF, Chambers IG, Hall GM. Temporomandibular joint disorders in patients referred for third molar extraction. Australian Dent J 2009; 54:323–325.
- Eapen BV, Baig MF, Avinash S. An assessment of the incidence of prolonged postoperative bleeding after dental extraction among patients on uninterrupted low dose aspirin therapy and to evaluate the need to stop such medication prior to dental extractions. J Maxillofac Oral Surg 2017; 16:48–52.
- Misra SR, Shankar YU, Rastogi V, et al. Metastatic hepatocellular carcinoma in the maxilla and mandible, an extremely rare presentation. Contemporary Clin Dent 2015; 6:S117–21.
- Mahan PE. TMJ disorders and orofacial pain. The role of dentistry in a multidisciplinary diagnostic approach. Dentomaxillofac Radiol 2003; 212–213.
- Huang GJ, Rue TC. Third-molar extraction as a risk factor for temporomandibular disorder. J Am Dent Assoc 2006; 137:1547–1554.
- Steed MB, Perciaccante VJ. (2007) Complications of third molar surgery. Oral Maxillofac Surg 2007; 19:117-128.
- Susarla SM, Blaeser BF, Magalnick D. Third molar surgery and associated complications. Oral Maxillofac Surg Clin North Am 2003; 15:177–186.
- Wahab PA, Nathan PS, Madhulaxmi M, et al. Risk factors for post-operative infection following single piece osteotomy. J Maxillofac Oral Surg 2017; 16:328–332.
- Patil SB, Durairaj D, Kumar GS, et al. Comparison of extended nasolabial flap versus buccal fat pad graft in the surgical management of oral submucous fibrosis: A prospective pilot study. J Maxillofac Oral Surg 2017; 16:312–321.
- Jain M, Nazar N. Comparative evaluation of the efficacy of intraligamentary and supraperiosteal injections in the extraction of maxillary teeth: A randomized controlled clinical trial. J Contemporary Dent Practice 2018; 19:1117–1121.
- PC J, Marimuthu T, Devadoss P, et al. Prevalence and measurement of anterior loop of the mandibular canal using CBCT: A cross sectional study. Clin Implant Dent Related Res 2018; 20:531–534.
- Marimuthu M, Andiappan M, Wahab A, et al. Canonical Wnt pathway gene expression and their clinical correlation in oral squamous cell carcinoma. Indian J Dent Res 2018; 29:291–297.
- Wahab PA, Madhulaxmi M, Senthilnathan P, et al. Scalpel versus diathermy in wound healing after mucosal incisions: A split-mouth study. J Oral Maxillofac Surg 2018; 76:1160–1164.
- Abhinav RP, Selvarasu K, Maheswari GU, et al. The patterns and etiology of maxillofacial trauma in south India. Annals Maxillofac Surg 2019; 9:114–117.
- Ramadorai A, Ravi P, Narayanan V. Rhinocerebral mucormycosis: A prospective analysis of an effective treatment protocol. Annals Maxillofac Surg 2019; 9:192–196.
- Senthil Kumar MS, Ramani P, Rajendran V, et al. Inflammatory pseudotumour of the maxillary sinus: clinicopathological report. Oral Surg 2019; 12:255–259.
- Sweta VR, Abhinav RP, Ramesh A. Role of virtual reality in pain perception of patients following the administration of local anesthesia. Annals Maxillofac Surg 2019; 9:110–113.
- Barbosa C, Gavinha S, Soares T, et al. Coincidence and awareness of the relationship between temporomandibular disorders and jaw injury. Orthodontic Treatment third and third molar removal in university students. J Oral Facial Pain Headache 2016; 30:221–227.
- Akhter R, Hassan NM, Ohkubo R, et al. The relationship between jaw injury, third molar removal, and orthodontic treatment and TMD symptoms in university students in Japan. J Orofac Pain 2008; 22:50–56.
- Grossi GB, Maiorana C, Garramone RA, et al. Assessing postoperative discomfort after third molar surgery: A prospective study. J Oral Maxillofac Surg 2007; 65:901–917.
- Mesgarzadeh AH, Hasanpur KA, Jafari M. (2013) Effect of surgical removal of impacted third molars on trismus value. Jundishapur Sci Med J 2013.
Author Info
Keerthika S and Santhosh Kumar MP*
Department of Oral and Maxillofacial Surgery, Saveetha Dental COLLEGE and Hospitals, Saveetha Institute of Medical and Technical Science, Saveetha University, Chennai, IndiaCitation: Keerthika S, Santhosh Kumar MP, Prevalence of Temporomandibular Joint Disorders in Patients with Impacted Teeth: An Institutional Study, J Res Med Dent Sci, 2020, 8 (7): 322-326.
Received: 16-Oct-2020 Accepted: 04-Nov-2020 Published: 11-Nov-2020
