Research - (2020) Volume 8, Issue 6
Pregnancy Success Predictive Value of Endometrial and Uterine Doppler Markers When Using Oral Ovarian Induction Medication in Subfertile Patients
Median Atia Alkhalaf Almamou1,2* and Asim Kurjak3
*Correspondence: Median Atia Alkhalaf Almamou, Sarajevo Medical School, Sarajevo School of Science and Technology University, Croatia, Email:
Abstract
Background: Most of the studies evaluating doppler use in endometrial receptivity and infertility management were in IVF cycles. None or few done to evaluate them with oral ovulation induction. We think that doppler can predict success rate with oral infertility management.
Methods: This study is a randomized prospective study. Infertile Patients with PCOS or unexplained subfertility were recruited from couples following with the infertility unit at Al-Moosa Hospital in Al-Ahsa in the Kingdom of Saudi Arabia. Randomization is done to use either clomiphene or letrozole. On the hCG trigger day and the mid-luteal day, we compared sub endometrial arteries and uterine artery doppler markers, Applebaum scoring system, endometrial thickness and blood vessels flow, the pattern between positive and negative test groups.
Results: On the trigger day, there was sufficient evidence to suggest that the endometrial width influences pregnancy success rate with a p-value of 0.0004. While, on the mid-luteal day, evidence was enough to suggest that type A endometrial pattern and zone 2 vascularity are associated with increased pregnancy success rate with a p-value of .021, 0.02, respectively. We prove that we can Predict success pregnancy rate using Applebaum Scores with a p-value of .0002. Uterine arteries PI and RI on the trigger day is associated with higher pregnancy rate with a p-value of .0005, 0.001, respectively. Finally, the pregnancy rate in our study was 18.52%.
Conclusions: On the trigger day, uterine artery PI and RI, Applebaum scoring system and endometrial thickness was predictive of pregnancy. Endometrial pattern and vascularity on the mid-luteal day are correlated with positive pregnancy success rate.
Keywords
Pregnancy, Oral ovulation induction, PCOS, Endometrial, Ovulation
Introduction
The main use of sonography in subfertility is follicular diameter monitoring. Unfortunately, the use of doppler sonography is still uncommon due to many factors such as the need for good training and insufficient studies justifying its use in infertility. We aim to increase doppler use by proving its advantages in infertility and ovulation induction. The most used treatments for ovulation induction are clomiphene citrate and letrozole. Although there is debate on which one is better in oral ovulation induction, most studies favour letrozole over clomiphene citrate [1]. Mainly, clomiphene works through antagonizing estrogen receptors [2]. Estrogen receptors antagonization will stimulate the hypothalamus-pituitary axis to increase the secretion of gonadotrophins [3]. Even it causes extremely high ovulation rate; its pregnancy rate is low. Endometrial thinning with its use may be the reason for that [4] besides decreased quality and quantity of cervical mucus [5]. However, suppression of androgen aromatization is the mode of the main action for letrozole. This action will cause low estrogen production, which in turn causes positive feedback on the hypothalamuspituitary axis. Increased gonadotropin levels will stimulate follicular growth. It is suggested that higher endometrial diameter is associated with better pregnancy rate [6].
Objective
To assess ultrasound doppler use in the management of subfertile couples.
Hypothesis
There is a difference between positive and negative pregnancy success groups in subfertile couples in terms of ultrasound markers (Endometrial thickness, pattern, blood flow, endometrial receptivity scoring system and doppler indices of uterine and sub endometrial arteries).
Materials and Methods
Selection of study subjects
We did a randomized prospective comparative study. All couples were given detailed information about the study, and their permission was insured through informed consent, and they sign for that. The ethical committee of Al Moosa Specialist Hospital gave our study ethical approval. The infertile couples' cases were collected from the outpatient department in the IVF unit of Al Moosa Specialist Hospital.
Inclusion criteria
Age range: 18-38 years.
Normal Hysterosalpingography.
Normal semen study.
Informed consent.
Exclusion criteria
Pelvic disease (PID, endometriosis, etc.).
Pelvic surgery.
Large fibroids (>4 cm) or sub endometrial fibroids.
Uterine distortion due to anomalies or surgeries.
Intra pelvis adhesions.
Primary amenorrhea.
Primary ovarian insufficiency.
Pituitary or hypothalamic causes of hypogonadism.
Male infertility.
Unmanaged Thyroid diseases or hyperprolactinemia.
Non-responsive cases or cases with early ovulation (before triggering).
Obesity.
Using 2003 Modified Rotterdam consensus, we diagnose PCOS [7] and all doppler sonography studies were done by the same doctor to avoid the inter-observer variability. The ultrasound machine used was GE Voluson P80 with a transvaginal probe of 5-9 MHz.
Randomization was done into two groups
Group A: group induced with clomiphene.
Group B: group induced with letrozole.
No coffee, tea, smoking, medications, or herbal products were allowed within 6-8 hours before each sonography study. All studies were done with lithotomy position and an empty bladder. Letrozole was given starting from the third day of the periods with an amount of 2 tablets once daily for five days while we gave two tablets of clomiphene citrate once daily for five days from the third day of the cycle.
Evaluation of study subjects
A basic vaginal sonography study was done at day two or three of the period to assess pelvic structures and to do randomization of induction treatment.
The criteria for triggering was when the leading follicle reaches 18 mm in size or more. the follicular size was assessed using the mean of two diameters intersecting at right angles [8].
Triggering was done using intermuscular 10000 units of Choriomon or Pregnyl in the morning of the same day. Timing of coitus was doubled to be at 1 and 1.5 days from triggering.
We cancelled the cycle all follicles are less than 12 mm at 16 days from the start of the period. On the trigger day, we did a sonographic study of the endometrial diameter, pattern, blood vascularity, Applebaum receptivity scoring system, uterine and sub endometrial arteries PI and RI.
The endometrial diameter assessment was done at the widest thickness at the median plane, on the external edges from side to side.
A pattern of the endometrium was stratified using a Gonen and Casper system [9]
Type "A": Endometrial hyperechogenic with no visible midline.
Type "B": endometrial myometrial-like echogenicity with no visible medline.
Type "C": A trilaminar endometrium with hyperechogenicity in the external edges and the medline and hypoechogenicity in between.
Endometrial and sub endometrial vascularity was studied on the hCG trigger day and about seven days post ovulation.
Zones of vascularity were divided into four zones on the day of trigger
Zone one: blood flow surrounds the outer edge of the endometrium with no vascularity in the endometrium.
Zone two: blood flow reaches the hyperechoic outer layer.
Zone three: blood flow reaches the hypoechoic layer.
Zone four: blood flow reaches the midline.
Zones of vascularity on the mid-luteal day were divided into two zones
Zone one: blood flow surrounds the outer edge of the endometrium
Zone two: blood flow reaches the endometrium.
The Applebaum Scoring System parameters are [10]
Diameter of the endometrium
14 mm=1
10-14 mm=3
7-9=2
<7 mm=0
Layers of the endometrium
Absent of layers=0
Blurred 5-lines=1
Clear 5-lines=3
Waves of the endometrium: (endometrial motion waves detected using a high-speed playback)
Less than three waves in 60 seconds=0
Three or more waves in 60 seconds=3
Homogeneity of the myometrium
Inhomogeneity=1
homogeneous myometrium=2
Uterine artery PI
>2.99=0
2.5-2.99=0
2.2-2.49=1
< 2.2 =2
Zone 3 vascularity of the endometrium
No vascularity=0
Scattered vascularity=2
Multifocal vascularity=5
Myometrial vascularity (spiral arteries)
Absent=0
Present=2
sub endometrial arteries doppler indices (RI and PI) studied at 1-2 mm lateral to the outer edges of the endometrium. Uterine artery PI and Ri were recorded from the uterine artery main branch on the lateral edges of the cervix. We used the least possible filter PRF (for uterine artery 1.3 PRF and 0.3 for PRF of the sub endometrial arteries). For the doppler indices (PI, RI), we used the mean of both sides of the uterine arteries.
We used Dydrogesterone (Duphaston) 10 mg twice daily orally for 14 days starting from day three after the day of the trigger. A serum pregnancy test was requested 16 days after hCG triggering. We did a pelvic scan at four weeks from the day of the trigger to confirm embryo viability. The same steps can be repeated (up to 2 successive cycles) in unsuccessful cycles if the couple agrees.
Data analysis
In the statistical tests, we used Excel and SPSS. The G Power software was used for calculating expected sample size and power.
Results
Fisher's exact test sample size was calculated using G Power software with control group proportion of .05, experimental group proportion of .4, two-sided α error of .05, the power value of 80% and an allocation ratio of 1. The calculated sample size was 48 cycles.
The sample size of the point biserial correlation test was calculated to be 52 cycles. We also used G Power software with an α error of .05, moderate effect size of .37 and an 80% power.
In our study, we used 54 cycles of ovulation induction; 27 cycles were done in each group. The differences in the mean BMI (p=.153) and the mean age (p=.109) were not significant in both groups (Table 1).
| Protocol | ||||||
|---|---|---|---|---|---|---|
| Clomiphene citrate group | Letrozole group | |||||
| Mean | N | Std. Deviation | Mean | N | Std. Deviation | |
| Age | 26.4 | 27 | 4.9 | 28.3 | 27 | 4.5 |
| BMI | 25.6 | 27 | 5.1 | 27.9 | 27 | 6.2 |
Table 1: Age and BMI with letrozole and clomiphene citrate groups.
The comparison included the endometrial width, vascularity and pattern, sub endometrial arteries PI and RI, Uterine artery PI and RI and Applebaum Uterine Scoring System.
For the categorical data, we used Fisher's Exact Test. While we applied point-biserial correlation to calculate the correlation between the normally distributed continuous variables and the dichotomous variable (positive or negative test group); otherwise Rank-biserial Spearman's correlation was used.
The evidence was adequate to suggest that there is a moderate relationship between endometrial thickness on the day of trigger and pregnancy success rate with a p-value of 0.0004 and an Rs of .463. The mean mid-cycle width of the endometrium was higher with the positive test group (positive group 10.84 ± 2.18 vs. 8.06 ± 1.84 for the negative group).
The mean mid-luteal width of the endometrium was higher with positive test group (12.89 ± 3.56 for positive test group vs 11.57 ± 2.89 for the negative test group), but the difference was not statistically significant with a P-value of 0.099 (Figure 1).
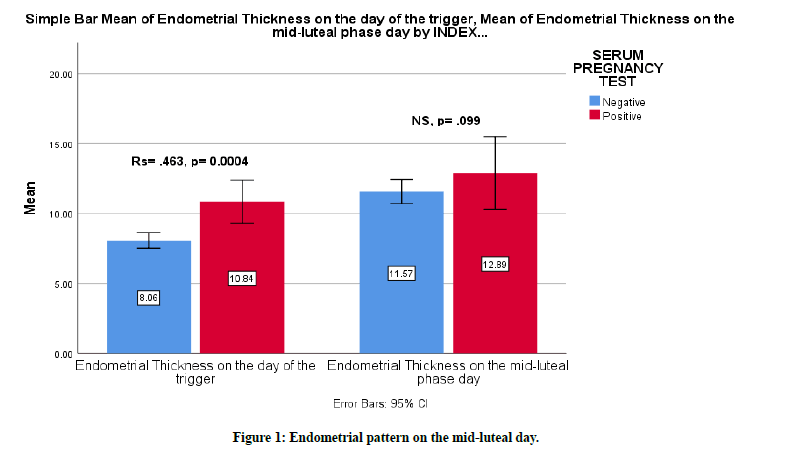
Figure 1. Endometrial pattern on the mid-luteal day.
The effect of endometrial pattern on pregnancy success rate was studied using Fisher's Exact Test. On the day of trigger, there was no sufficient evidence to suggest that there is an effect of endometrial pattern on pregnancy success rate (type A p=1, type B p=.674, type C p=1). While, on the mid-luteal day, We found a pregnancy rate of 27.8% in type A endometrium and there was sufficient evidence to suggest that there is a moderate relationship between type A endometrium and pregnancy success rate with a p-value of 0.021 and a Phi value of 0.337 (Figure 2).
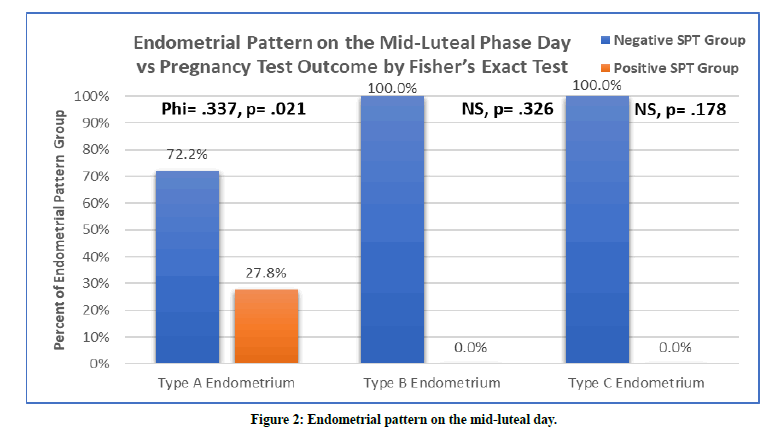
Figure 2. Endometrial pattern on the mid-luteal day.
Endometrial blood flow vascularity was studied using Fisher's Exact Test. On the trigger day, there was no sufficient evidence to suggest that there is an effect of the vascularity zones on pregnancy rate (zone 1 p=1, zone 2 p=0.667, zone 3 p=0.291, zone 4 p=1). While on the mid- luteal day, we found 26,32% success rate with zone 2 and there was sufficient evidence to suggest that there is a moderate relationship. The p-value for the two-sided Fisher's Exact test was 0.024, with moderate phi test effect size of 0.309. The endometrial vascularity on the midluteal day was more prominent with the positive test group (Figure 3).
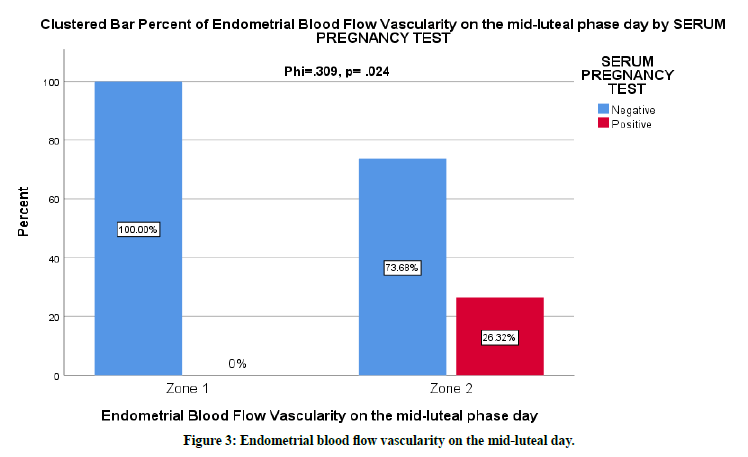
Figure 3. Endometrial blood flow vascularity on the mid-luteal day.
The mean of the Applebaum Endometrial Receptivity Scoring System was higher with the positive pregnancy test group (14.7 ± 1.34 for the positive group vs 11.27 ± 3.14 for the negative group). There was evidence to suggest that there is a correlation between Applebaum score and pregnancy rate, rs=0.485, p=0.0002 (Figure 4).
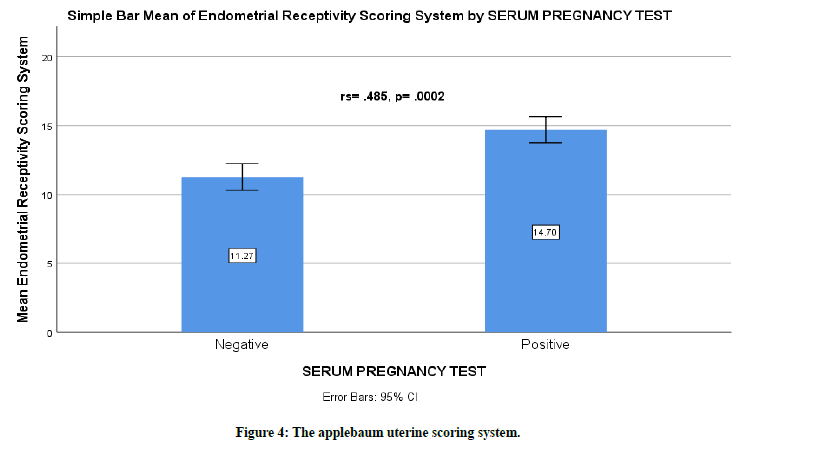
Figure 4. The applebaum uterine scoring system.
On the trigger day, there was no sufficient evidence to suggest that sub endometrial artery PI & RI has a rule in predicting pregnancy success with a p-value of 0.11, 0.19, respectively (Table 2).
| On the trigger day | Positive Group | Negative Group | rs | p-value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Sub endometrial artery PI | 1.14 | 0.54 | 1.23 | 0.32 | -0.11 | 0.11 |
| Sub endometrial artery RI | 0.62 | 0.1 | 0.66 | 0.09 | -0.18 | 0.19 |
| Mean uterine artery PI | 2.29 | 0.41 | 2.91 | 0.41 | -0.46 | 0.0005 |
| Mean uterine artery RI | 0.84 | 0.04 | 0.89 | 0.04 | -0.42 | 0.001 |
Table 2: The trigger day doppler indices.
The mean of uterine arteries PI on the trigger day was lower with the positive pregnancy test group 2.29 (SD=0.41) vs 2.91 (SD=0.41) for the negative pregnancy test group. There was evidence to suggest that with lower uterine artery PI, the possibility of pregnancy increases. There was a moderate correlation between pregnancy success rate and uterine artery PI, rs=-0.46, p=.0005 (Figure 5).
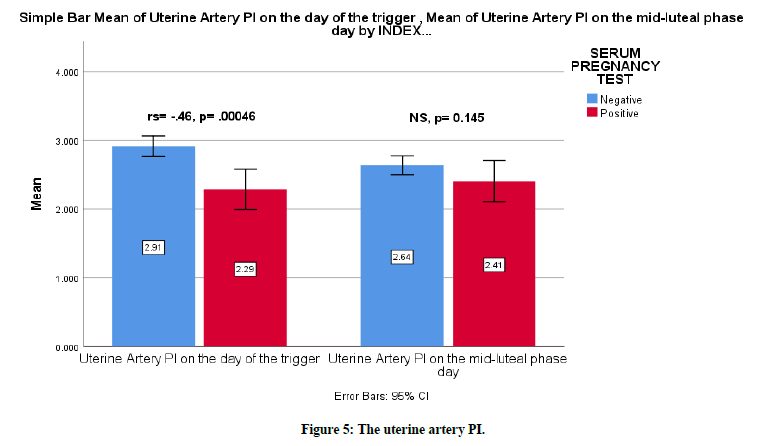
Figure 5. The uterine artery PI.
The mean of uterine arteries RI on the day of the trigger was lower with the positive pregnancy test group 0.84 (SD=0.04) vs .89 (SD=0.04) with the negative pregnancy test group. There was evidence to suggest that with lower uterine artery RI, the possibility of pregnancy increases. There was a moderate correlation between pregnancy success rate and uterine artery PI, rs=-0.42, p=0.001 (Figure 6). On the mid-luteal day, there was no sufficient evidence to suggest that there is an effect on pregnancy success rate neither from sub endometrial artery PI or RI nor from mean of uterine arteries PI or RI with a p-value of 0.22, 0.11, 0.145, 0.2 respectively (Table 3).

Figure 6. The RI doppler indices.
| On the mid-luteal day | Positive Group | Negative Group | rs | p-value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Sub endometrial artery PI | 1.38 | 0.32 | 1.24 | 0.35 | 0.17 | 0.22 |
| Sub endometrial artery RI | 0.71 | 0.08 | 0.66 | 0.08 | 0.22 | 0.11 |
| Mean uterine artery PI | 2.41 | 0.42 | 2.64 | 0.45 | -0.2 | 0.145 |
| Mean uterine artery RI | 0.84 | 0.04 | 0.86 | 0.04 | -0.18 | 0.199 |
Table 3: The mid-luteal day doppler indices.
Finally, the total pregnancy rate was 18.52%. The pregnancy rate in the clomiphene group was 14.8% vs 22.2% for letrozole group. However, Fisher's Exact Test was performed to examine the relationship between the ovulation induction medication and pregnancy rate. The evidence was not sufficient to suggest that there is a relationship with a p-value of 0.728 (Figure 7).
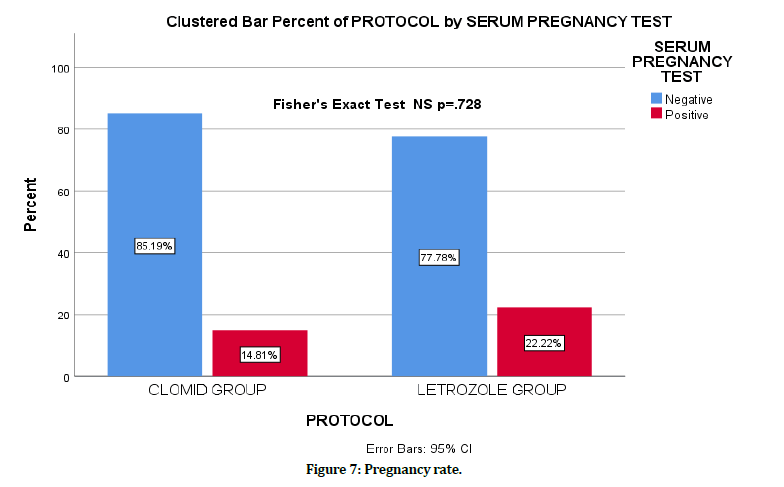
Figure 7. Pregnancy rate.
Discussion
Endometrial perfusion is thought to be a regulatory factor of the receptiveness of the endometrium. Uterine resistance PI and RI are significantly lower in the positive pregnancy test group. Before embryo transfer, the receptiveness of the endometrium can be predicted by the spiral artery doppler indices [11]. Also, Steer et al. and Cacciatore et al. think that uterine artery PI and RI is lower in IVF infertile couples with the positive pregnancy test group [12,13].
On the other hand, many studies found no evidence that PI and RI values in IVF cycles significantly different between groups for the failed and the successful pregnancy test [14,15]. It was suggested that the highest pregnancy rate occurred uterine arteries PI is between 2-3 [16,17]. All of the studies of uterine and sub endometrial perfusion conduct so far were in the setting of IVF or IUI, and none of them was done with oral ovulation induction setting. This study aims to evaluate uterine blood flow in subfertile couples to reveal the possible role of the uterine doppler parameters in infertility management.
Consequently, we hypothesized that abnormal uterine and sub endometrial blood flow might be a crucial causative element in infertile ladies. There are many suggested invasive ways to predict the receptiveness of the endometrium, including biopsy and immunohistochemical studies. The use of doppler ultrasonography is a non-invasive way of studying the impedance of the uterus.
We found in this study that neither endometrial pattern nor endometrial vascularity on the trigger day has a rule in predicting successful pregnancy. While endometrial width on the trigger day was thicker in the positive test group and can be used as a predictor of pregnancy, on the mid-luteal day endometrial thickness has no role in predicting successful pregnancy while endometrial pattern (type A) and endometrial vascularity (zone 2) can be used as predictors of a successful pregnancy. There was satisfactory evidence that Applebaum score is higher in the successful pregnancy group so that we can use it as well as an indicator of implantation and successful pregnancy.
On the trigger day, we also found that sub endometrial artery PI & RI has no rule in predicting pregnancy success while the mean of the uterine arteries PI & RI has. We can use uterine arteries PI & RI in infertility management to predict the successful cycles. On the mid-luteal day, none of the doppler parameters has a rule in infertility management. Our data indicates that pregnancy rates were 18.52 %. It was higher with the letrozole group (22.2% vs 14.8%), but the difference has no statistical significance.
Conclusion
We can use uterine PI and RI and endometrial width on the trigger day to predict positive pregnancy. Also, we can predict pregnancy using endometrial width on the trigger day. On the mid-luteal day, type A endometrial pattern and zone 2 endometrial vascularity were seen more with Positive pregnancy test group. There was good evidence that Applebaum scoring system is a useful tool in infertility management.
Acknowledgment
The authors would be keen on expressing gratitude to the members of the school of Science and Technology (SSST) university and the administration of Almoosa Specialist Hospital for their support towards making this research a success.
Ethical Considerations
A consent to be involved in the research was taken from every single couple. Moreover, the approval of the ethical and research Committee in Almoosa specialist hospital was obtained.
Funding
The authors bore the entire cost of the research and did not obtain any economic assistance from any organization.
Conflict of Interest
The authors state no conflicts of interest.
References
- Legro RS, Brzyski RG, Diamond MP, et al. Clomiphene versus letrozole for infertility in the polycystic ovary syndrome. New England J Med 2014; 371:119-129.
- Practice committee of the american society for reproductive medicine. Use of clomiphene citrate in women. (2003). Fertil Steril 2003; 80:1302–1308.
- Kettel LM, Roseff SJ, Berga SL, et al. Hypothalamic-pituitary-ovarian response to clomiphene citrate in women with polycystic ovary syndrome. Fertil Steril 1993; 59:532-538.
- Gadalla MA, Huang S, Wang R, et al. Effect of clomiphene citrate on ovulation, endometrial thickness, and live birth in anovulatory women: systematic review and meta-analysis. Ultrasound Obstetrics Gynecol 2017; 51:64–76.
- Thompson LA, Barratt CLR, Thornton SJ, et al. The effects of cyclofenil and clomiphene citrate on cervical mucus volume and receptivity over the periovulatory period. Fertility and Sterility, 1993; 59:125–129.
- Kovacs P, Matyas SZ, Boda K, et al. The effect of endometrial thickness on IVF/ICSI outcome. Hum Reprod 2003; 18:2337–2341.
- Revised 2003 consensus on polycystic ovary syndrome diagnostic criteria and long-term health risks related to it. Fertil Steril 2004; 81:19–25.
- Schild RL, Knobloch C, Dorn C, et al. Assessing receptivity of endometrium in an in vitro fertilization program by endometrial thickness, endometrial volume, spiral artery blood flow and uterine artery blood flow. Fertil Steril 2001; 75:361–366.
- Gonen Y, Casper RF. Prediction of implantation by the sonographic appearance of the endometrium during controlled ovarian stimulation for in vitro fertilization (IVF). J In Vitro Fert Embryo Transf 1990; 7:146–152.
- Applebaum M. The uterine biophysical profile. Ultrasound Obstet Gynecol 1995; 5:67–68.
- Gong X, Lı Q, Zhang Q, et al. Predicting endometrium receptivity with parameters of spiral artery blood flow. Huazhong University Sci Technol J 2005; 25:335–338.
- Steer CV, Tan SL, Dillon D, et al. Vaginal colour doppler assessment of uterine artery impedance correlates with immunohistochemical markers of endometrial receptivity required for the implantation of an embryo. Fertil Steril 1995; 63:101–118.
- Cacciatore B, Simberg N, Fusaro P, et al. Transvaginal doppler study of uterine artery blood flow in in vitro fertilization-embryo transfer cycles. Fertil Steril 1996; 66:130–134.
- Favre R, Bettahar K, Grange G, et al. Predictive value of transvaginal uterine doppler assessment in an in vitro fertilization program. Ultrasound Obstet Gynecol 1993; 3:350–353.
- Bassil S, Magritte JP, Roth J, et al. Uterine vascularity during stimulation and its correlation with implantation in in-vitro fertilization. Hum Reprod 1995; 10:1497–1501.
- Zaidi J, Shaker A, Pittrof R, et al. Uterine artery blood flow assessment on the day of HCG administration by transvaginal colour doppler ultrasound in an in vitro fertilization program. Fertil Steril 1996; 65:377–381.
- Tsai YC, Chang JC, Tai MJ, et al. Relationship of uterine perfusion to the outcome of intrauterine insemination. J Ultrasound Med 1996; 15:633–636.
Author Info
Median Atia Alkhalaf Almamou1,2* and Asim Kurjak3
1Sarajevo Medical School, Sarajevo School of Science and Technology University, Sarajevo, Bosnia and Herzegovina, Balkans, Croatia2IVF Unit, Obstetrics and Gynaecology Department, Almoosa Specialist Hospital, Saudi Arabia
3Medical School, Universities of Zagreb and Sarajevo, Zagreb, Croatia
Citation: Median Atia Alkhalaf Almamou, Asim Kurjak, Pregnancy Success Predictive Value of Endometrial and Uterine Doppler Markers When Using Oral Ovarian Induction Medication in Subfertile Patients, J Res Med Dent Sci, 2020, 8 (6): 232-240.
Received: 04-Sep-2020 Accepted: 30-Sep-2020
