Research - (2022) Volume 10, Issue 6
Preference of the Patient in Choosing Metal Ceramic Vs. all Ceramic Crowns after Undergoing Root Canal Treatment in the Upper Anterior Tooth
Debarun David and Vigneshwar T*
*Correspondence: Vigneshwar T, Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University, Chennai, Tamil Nadu, India, Email:
Abstract
Introduction: The metal-ceramic crown system is still frequently preferred because of its strength and versatility. The ability to select metals for color or strength for single units gives great flexibility, but when esthetics of the anterior region are a prime concern, the all-ceramic crown is still an excellent choice. Choice of which all-ceramic system to use is dependent on the strength demands, esthetic needs, amount of tooth structure that can be preserved, and laboratory support available. Aim: The aim of this is to assess the preference of the patient in choosing metal ceramic vs. all ceramic crowns after undergoing root canal treatment in the upper anterior tooth. Materials and methods: A Retrospective analysis of all patients that underwent root canal treatment in the anterior teeth and required a single crown. The overall data of patients visiting Saveetha Dental College from June 2019-March 2020. The data for 31 patients who preferred metal ceramic and all ceramic crowns was entered in Excel Spreadsheets. And the collected data was analysed using SPSS software version 19. Chi square test was used to statistically evaluate the results. Results: Our results shows that majority of the patients wanted all ceramic crowns, 12.90% in the age group 19-25 wanted all ceramic crowns, 3.23% wanted metal ceramic crowns. 25.81% in the age group 26-40 wanted all ceramic crown, 6.45% wanted metal ceramic crowns. 35.48% in the age group 41-60 wanted all ceramic crowns, 6.45% wanted metal ceramic. 3.23% in the age group 61-83 wanted all ceramic crowns, 6.45% wanted metal ceramic crowns. Conclusion: It was seen that most patients preferred all ceramic crowns. All-ceramic single crowns exhibit similar survival rates as metal-ceramic single crowns and is recommended in anterior regions as it needs low functional load. The main reason to use of the all-ceramics instead of metal-ceramics is based on more favorable esthetic.
Keywords
Ceramic, Metal ceramic crowns, Root canal therapy, Innovative study
Introduction
Many prosthetic treatment modalities have been suggested after the completion of the root canal therapy. Most of them involve either crowns or direct restorations such as resin composites, amalgam or cements. There is a need for a full coverage crown to prevent root fracture in endodontically treated [1]. Recent progress in the technology and research of new materials has broadened the choices for esthetic single-crown restorations. Allceramic fixed dental prostheses (FDPs) are considered an established treatment alternative to metal-ceramic FDPs in daily clinical practice [2].
The main reason to use all- ceramics instead of metalceramics is based on more favorable esthetics [3]. But, until recently it was not possible to recommend all-ceramic single or multiple-unit FDPs as clinically equivalent treatment alternatives to metal ceramic FDPs. Metal-ceramics remained to be the “gold standard” type of reconstruction. However, numerous new dental ceramic materials were developed with the aim to increase the overall stability of the all-ceramic reconstructions, while still maintaining the esthetic benefit. A recent study [4] of the failure of ceramic-based FDPs confirmed a previous estimate that less than 85% or more of fixed dental prostheses were still functional after 10 years in service. However, there was considerable variability in the number of parameters that were reported as well as the extent of details on the failures that had occurred [5].
Therefore, for the long-term performance of implantsupported crowns, it is essential to control the risk factors contributing to peri implant diseases and to ensure the patient receives an adequate maintenance program [6]. Our team has extensive knowledge and research experience that has translate into high quality publications [7-26]. The aim of that study is to assess the preference of crown after undergoing root canal treatment in the upper anterior tooth.
Materials and Methods
Study population
A retrospective study was carried out among adults reporting to Saveetha Dental College and Hospital. The study was conducted between June 2020-March 2021. The study population consists of patients who reported with Root canal treated anterior teeth that require crown.
Ethical approval
Ethical approval was obtained from the Institutional Ethical Committee and Scientific Review Board (SRB) of Saveetha Dental College.
Data collection
The data were collected by analyzing the records of 86,000 patients between June 2019-March 2020. The data consisted of patient details, tooth number and the type of crown selected.
Data analysis
The collected data were entered in an Excel sheet and subjected to statistical analysis using SPSS software. Chi square tests were done between the age, gender and preference of crown. The level of significance is p<0.05.
Results and Discussion
Dental crowns come in a variety of materials, including metals, resins, and porcelain, or a combination of these. Each offers varying degrees of strength and durability as well as cosmetic benefits. The most durable crown, metal crowns incorporate gold, nickel, palladium, or chromium. This category ranks as an ideal choice for teeth all the way in the back of the mouth that are exposed to the highest chewing forces. A negative side to this material is appearance, the metallic color means it will not mimic the esthetics of a natural tooth and is not suited for front teeth. All-Ceramic or All-Porcelain matches your natural tooth color, an all-ceramic or all-porcelain crown would be the preferred option, especially for anterior teeth. The only drawback of these types of crowns is that they’re less durable than metal crowns and may not last quite as long. Like a porcelain crown, a porcelain-and-metal fusion mimics the hue of your teeth. However, you may see a metal line in the tooth is not as natural looking, and the porcelain may be susceptible to chips and breaks. While this type of crown is still used in some offices, it is being phased out by the all ceramic crowns, which are made of stronger glass hybrids like Lithium disilicate or solid zirconia. All resin crowns are more vulnerable to chipping and breakage. Typically all resin crowns are used as provisional or temporary crowns [5]. However, Metal Ceramic crowns have been considered the gold standard in the rehabilitation of teeth and implants. However, ceramic restorations became an appropriate alternative to Metal Ceramic crowns, mainly for those patients with high esthetic needs. This meta-analysis aimed to provide information to support dental clinicians’ treatment decision-making based on the best available evidence by concluding the results of a Randomized clinical trial [27]. The null hypothesis was accepted as the result of metaanalysis did not show differences between All ceramic and Metal Ceramic crowns restorations concerning prosthesis failure, complication rates, marginal bone loss, or patient satisfaction.
In our study, the majority of the patients wanted all ceramic crowns, 22.58% female wanted all ceramic and 54.84% male patients wanted all ceramic crowns. Only a few opted for metal ceramic crowns in the anterior region, even though metal ceramic has high fracture resistance.
Recent scientific progression shows that prosthesis failure can result from implant loss after infection, overload, excess cement [17] or an un restorable prosthesis fracture [28]. The ceramic restoration experienced a mechanical complication rate similar to that of the Metal Ceramic crowns restorations as indicated by the meta-analysis. The most frequent complication associated with ceramic crowns was veneer chipping [28].
For example, the interface bond between copings and ceramic is believed to be a contributing factor [29] as too is the residual stress resulting from the cooling of zirconia and the phenomenon of ageing [30]. The material property, design, and thickness of the ceramic veneer should all be sufficient; otherwise, the use of monolithic zirconia is preferred to bilayer ceramic restoration to avoid ceramic chipping. The authors clarified that this finding might be related to the poor marginal fit of All ceramic crowns, leading perhaps to more bacterial accumulation and subsequently chronic inflammation [31].
Our results showed that the majority of the patients wanted all ceramic crowns, out of all age groups 35.48% in the age group 41-60 wanted all ceramic crowns and the least was 3.23% among the age group 61-83 wanted all ceramic crowns and 6.45% wanted metal ceramic crowns. The meta-analysis of the visual analog scale scores indicated no difference between the restoration types [31]. This finding was presumably because the selected studies evaluated the posterior area of the mouth, which may have less impact on patient satisfaction, especially among adults with increasing age. The current meta-analysis included only Randomized clinical trials considered to provide substantial evidence. Additionally, this review included studies that compared ceramic and Metal Ceramic crowns within the same study to avoid indirect comparisons.
Most of the studies had a follow-up period of just 12 months, which is not sufficient to determine implant success or failure rate. Therefore, to overcome these problems, well-designed Randomized clinical trials with follow-up periods at least of 5 years and more are recommended to evaluate the long-term influence of the prosthesis material (Figures 1-4).
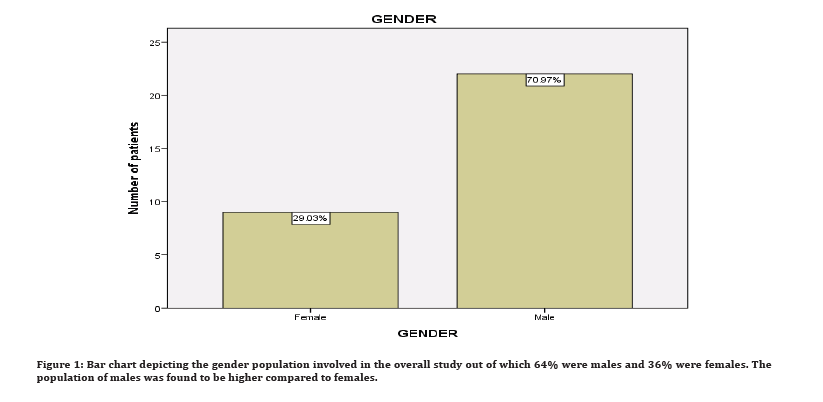
Figure 1: Bar chart depicting the gender population involved in the overall study out of which 64% were males and 36% were females. The population of males was found to be higher compared to females.
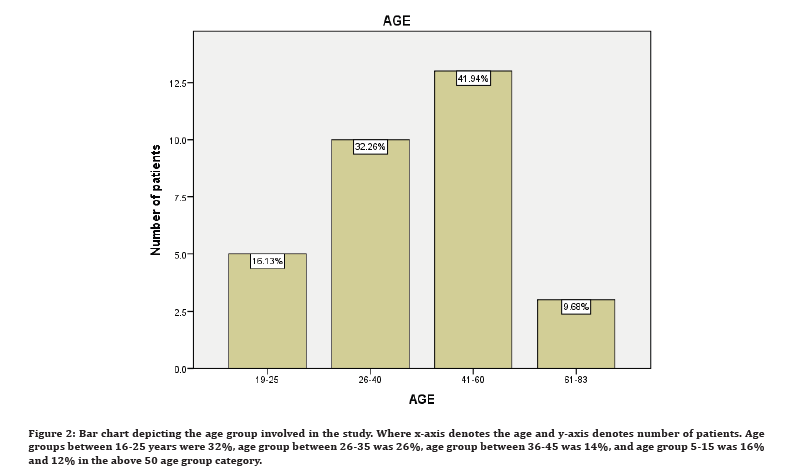
Figure 2: Bar chart depicting the age group involved in the study. Where x-axis denotes the age and y-axis denotes number of patients. Age groups between 16-25 years were 32%, age group between 26-35 was 26%, age group between 36-45 was 14%, and age group 5-15 was 16% and 12% in the above 50 age group category.
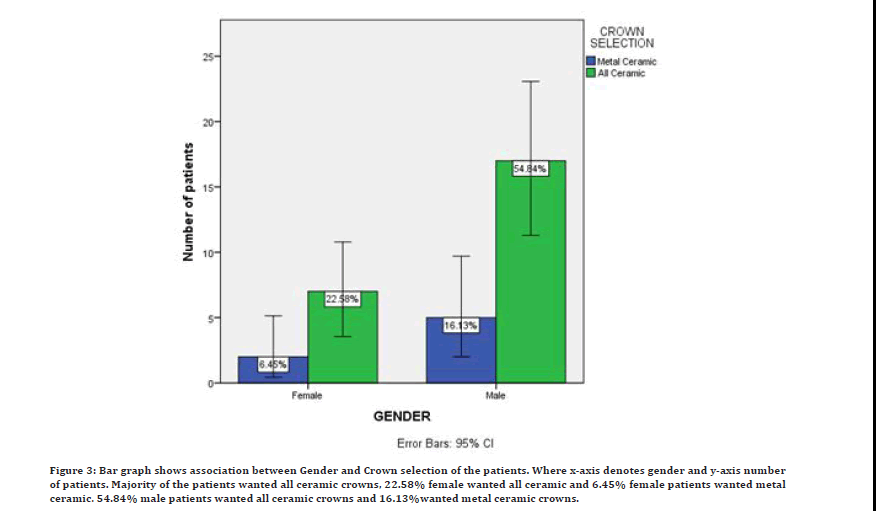
Figure 3: Bar graph shows association between Gender and Crown selection of the patients. Where x-axis denotes gender and y-axis number of patients. Majority of the patients wanted all ceramic crowns, 22.58% female wanted all ceramic and 6.45% female patients wanted metal ceramic. 54.84% male patients wanted all ceramic crowns and 16.13%wanted metal ceramic crowns.
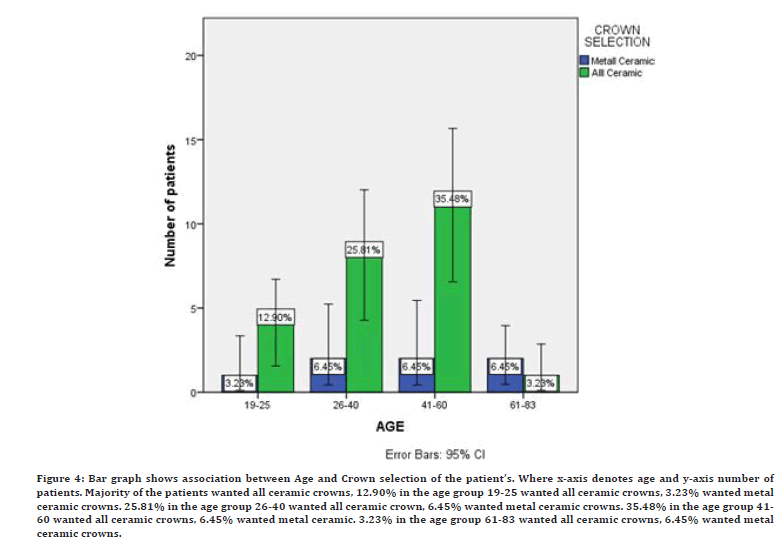
Figure 4: Bar graph shows association between Age and Crown selection of the patient’s. Where x-axis denotes age and y-axis number of patients. Majority of the patients wanted all ceramic crowns, 12.90% in the age group 19-25 wanted all ceramic crowns, 3.23% wanted metal ceramic crowns. 25.81% in the age group 26-40 wanted all ceramic crown, 6.45% wanted metal ceramic crowns. 35.48% in the age group 41- 60 wanted all ceramic crowns, 6.45% wanted metal ceramic. 3.23% in the age group 61-83 wanted all ceramic crowns, 6.45% wanted metal ceramic crowns.
Conclusion
Based on the findings of this systematic review. Data revealed that the materials analyzed (All ceramic vs. Metal ceramic crown ) have similar effects with regard to prosthesis failure, complication rates, and patient satisfaction in patients restored with single implantsupported crowns. Ceramic crowns provide the best and most natural look. They match your surrounding teeth in shape, size, and color. The best option for front teeth restorations. They are biocompatible: that means no metal is used, so they are toxic-free. The selection of material for single implant crowns depends on the dentist’s decision and the patient’s individual needs.
Acknowledgement
The authors are thankful to Saveetha Institute of Medical and Technical Sciences for providing a platform to express our knowledge.
Conflict of Interest
The author declares no conflict of interest.
Source of Funding
The present study is sponsored by:
Saveetha Institute of Medical and Technical Sciences, Saveetha Dental College and Hospitals, Saveetha University, India
Soma beverages, Trichy, India.
References
- Chamberlain BB, Razzoog ME, Robinson E. Quality of care: compared perceptions of patient and prosthodontist. J Prosthet Dent 1984; 52:744–746.
- Brisman AS. Esthetics: A comparison of dentists' and patients' concepts. J Am Den Assoc 1980; 100:345-352.
- Yu B, Lee YK. Comparison of the color stability of flowable and universal resin composites. Am J Dent 2009; 22:160–164.
- Suzuki T, Kyoizumi H, Finger WJ, et al. Resistance of nanofill and nanohybrid resin composites to toothbrush abrasion with calcium carbonate slurry. Dent Mater J 2009; 28:708–716.
- Pjetursson BE, Sailer I, Zwahlen M, et al. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: Single crowns. Clin Oral Implants Res 2007; 3:73–85.
- Abrams RA, Ayers CS, Petterson MV. Quality assessment of dental restorations: A comparison by dentists and patients. Community Dent Oral Epidemiol 1986; 317–319.
- Muthukrishnan L. Imminent antimicrobial bioink deploying cellulose, alginate, EPS and synthetic polymers for 3D bioprinting of tissue constructs. Carbohydr Polym 2021; 260:117774.
- PradeepKumar AR, Shemesh H, Nivedhitha MS, et al. Diagnosis of vertical root fractures by cone-beam computed tomography in root-filled teeth with confirmation by direct visualization: A systematic review and meta-analysis. J Endod 2021; 47:1198–1214.
- Chakraborty T, Jamal RF, Battineni G, et al. A Review of prolonged post-COVID-19 symptoms and their implications on dental management. Int J Environ Res Public Health 2021; 18.
- Muthukrishnan L. Nanotechnology for cleaner leather production: A review. Environ Chem Lett 2021; 19:2527–2549.
- Teja KV, Ramesh S. Is a filled lateral canal-A sign of superiority? J Dent Sci 2020; 15:562.
- Narendran K, Sarvanan A. Synthesis, characterization, free radical scavenging and cytotoxic activities of phenylvilangin, a substituted dimer of embelin. Indian J Pharm Sci 2020; 82:909-912.
- Reddy P, Krithikadatta J, Srinivasan V, et al. Dental caries profile and associated risk factors among adolescent school children in an Urban South-Indian City. Oral Health Prev Dent 2020; 18:379–386.
- Sawant K, Pawar AM, Banga KS, et al. Dentinal microcracks after root canal instrumentation using instruments manufactured with different NiTi alloys and the SAF system: A systematic review. Adv Sci Inst Ser E Appl Sci 2021; 11:4984.
- Bhavikatti SK, Karobari MI, Zainuddin SLA, et al. Investigating the Antioxidant and cytocompatibility of Mimusops elengi Linn extract over human gingival fibroblast cells. Int J Environ Res Public Health 2021; 18.
- Karobari MI, Basheer SN, Sayed FR, et al. An In vitro stereomicroscopic evaluation of bioactivity between Neo MTA Plus, Pro Root MTA, biodentine & glass ionomer cement using dye penetration method. Materials 2021; 14.
- Rohit Singh T, Ezhilarasan D. Ethanolic extract of Lagerstroemia speciosa (L.) Pers., induces apoptosis and cell cycle arrest in HepG2 cells. Nutr Cancer 2020; 72:146–156.
- Ezhilarasan D. Micro RNA interplay between hepatic stellate cell quiescence and activation. Eur J Pharmacol 2020; 885:173507.
- Romera A, Peredpaya S, Shparyk Y, et al. Bevacizumab biosimilar BEVZ92 versus reference bevacizumab in combination with FOLFOX or FOLFIRI as first-line treatment for metastatic colorectal cancer: A multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol 2018; 3:845–855.
- Raj RK. β‐Sitosterol‐assisted silver nanoparticles activates Nrf2 and triggers mitochondrial apoptosis via oxidative stress in human hepatocellular cancer cell line. J Biomed Materials Res 2020; 108:1899-908.
- Vijayashree Priyadharsini J. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol 2019; 90:1441–1448.
- Priyadharsini JV, Vijayashree Priyadharsini J, Smiline Girija AS, et al. In silico analysis of virulence genes in an emerging dental pathogen A. baumannii and related species. Arch Oral Biol 2018; 94:93–98.
- Uma Maheswari TN, Nivedhitha MS, Ramani P. Expression profile of salivary micro RNA-21 and 31 in oral potentially malignant disorders. Braz Oral Res 2020; 34:e002.
- Gudipaneni RK, Alam MK, Patil SR, et al. Measurement of the maximum occlusal bite force and its relation to the caries spectrum of first permanent molars in early permanent dentition. J Clin Pediatr Dent 2020; 44:423–428.
- Chaturvedula BB, Muthukrishnan A, Bhuvaraghan A, et al. Dens invaginatus: A review and orthodontic implications. Br Dent J 2021; 230:345–350.
- Kanniah P, Radhamani J, Chelliah P, et al. Green synthesis of multifaceted silver nanoparticles using the flower extract of Aerva lanata and evaluation of its biological and environmental applications. Chem Select 2020; 5:2322–31.
- Spear FM. Masters of esthetic dentistry: The metal-free practice: myth? reality? desirable goal?. J Esthetic Restorative Dent 2001; 13:59.
- Bösch A, Jung RE, Sailer I, et al. Single-tooth replacement using dental implants supporting all-ceramic and metal-based reconstructions: Results at 18 months of loading. Int J Periodont Restorative Dent 2018; 38:173–179.
- Lee JT, Lee HJ, Park SY, et al. Consecutive unsplinted implant-supported restorations to replace lost multiple adjacent posterior teeth: A 4-year prospective cohort study. Acta Odont Scandinavica 2015; 73:461-466.
- Esquivel-Upshaw JF, Clark AE, Shuster JJ, et al. Randomized clinical trial of implant-supported ceramic-ceramic and metal-ceramic fixed dental prostheses: preliminary results. J Prosthodont 2014; 23:73–82.
- Hosseini M, Worsaae N, Schiødt M, et al. A 3‐year prospective study of implant‐supported, single‐tooth restorations of all‐ceramic and metal‐ceramic materials in patients with tooth agenesis. Clin Oral Implants Res 2013; 24:1078.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Debarun David and Vigneshwar T*
Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University, Chennai, Tamil Nadu, IndiaCitation: Debarun David, Vigneshwar T, Preference of the Patient in Choosing Metal Ceramic Vs. all Ceramic Crowns after Undergoing Root Canal Treatment in the Upper Anterior Tooth, J Res Med Dent Sci, 2022, 10 (6):187-192.
Received: 26-May-2022, Manuscript No. JRMDS-22-65008; , Pre QC No. JRMDS-22-65008 (PQ); Editor assigned: 28-May-2022, Pre QC No. JRMDS-22-65008 (PQ); Reviewed: 14-Jun-2022, QC No. JRMDS-22-65008; Revised: 17-Jun-2022, Manuscript No. JRMDS-22-65008 (R); Published: 24-Jun-2022
