Review - (2019) Volume 7, Issue 2
Predictive Factors for Participation in Colorectal Cancer Screening: A Systematic Review
Shirin Barzanjeh Atri1, Mina Hosseinzadeh2, Mohamad Asghari Jafarabadi3, Mohammad Hasan Sahebihagh4,5 and Leila Ebadi6*
*Correspondence: Leila Ebadi, Community Health Nursing, Tabriz University of Medical Sciences, Iran, Email:
Abstract
Background: Colorectal cancer (CRC) is one of the prevalent diseases that can be diagnosed timely using appropriate screening programs. This study aimed to review the predictive factors for participation in colorectal cancer screening.
Methods: International databases including PubMed, ISI and Scopus were considered for search of English articles by 30 December, 2018. Thirty-one published articles were finally entered into the study. Keywords were “colorectal cancer”, “colorectal neoplasm”, “predictor”, “screening”, “Fecal Occult Blood Test (FOBT)”, “Fecal Immunochemical Test (FIT)”, “education”, “smoking”, “obesity” or a combination of them in the title/abstracts.
Findings: There were 367,248 subjects reviewed in this systematic review of 31 published articles consisted of two cohorts, one quasi-experimental; one mixed method, three randomized trial and twenty-six cross-sectional design.
Conclusion: According to the results, knowledge, income, being married and female, trust to physician and kindly contact of health providers, counselling centres disorders were the main predictive factors for participation in the CRC screening programs.
Keywords
Colorectal cancer, Colorectal neoplasm, Predictor, Screening, FOBT, FIT
Introduction
Cancer is one of the prevalent diseases that account for a large volume of lethal consequences as well as care efforts [1-5]. Among them, Colorectal Cancer (CRC) is now responsible for a large part of the burden of cancer and the fourth leading cause of cancer death worldwide [6]. The CRC is the second most common cancer in women [7,8] and after breast cancer is the most common cause of death in women [9,10]. Meanwhile, it can also be considered as the third most common cancer in men worldwide. It is estimated that the incidence and mortality rate of the CRC will increase by 77% and 80% by 2030, respectively [7].
The incidence and mortality rate of this cancer varies in different regions [11,12], which is more common in developing countries than in the rest of the world [13]. Fortunately, its mortality rate is declining in many western countries [7]. Cancer is also the third leading cause of death in Iran, so that the incidence of CRC has increased during the past 25 years in Iran especially among younger people [14,15].
Various risk factors have been reported for colorectal cancer, including aged more than 50 years, family history, nutrition patterns, obesity, inactivity, and cigarette smoking. However, the main cause of it has not been accurately known [9,16-19].
The survival rate of the CRC is reported 5 years after diagnosis [13], which is highly dependent on the time of diagnosis, so secondary prevention, which is the early diagnosis of cancer, is important [6,14]. The CRC is suitable for screening because it is a challenging health problem and there are some tests that can diagnose it earlier [20]. Initial and necessary measures for screening colorectal cancer often include training and advice for screening tests [21]. Regular screening is one of the best and most valuable early detection methods in the CRC [22-26].
Fecal Occult Blood Test (FOBT] and colonoscopy are the most commonly used tests for colorectal cancer screening [4]. One of the reasons for the low CRC screening rate is the lack of participation in these programs [27]. In addition, standard educational materials for promoting CRC screening have also been unfortunately unsuccessful [28]. Three major categories of screening agents have been reported in various sources including; 1) demographic characteristics such as race, ethnicity, level of education and age; 2) psychological effects such as knowledge, risk perception and health behaviors, and 3) health system factors such as health insurance coverage, physician advice and the usual source of health care. Also, studies have shown that people who are involved in unhealthy behaviors, such as smoking and physical inactivity, are less likely to use screening tests recommended for cancers [29].
In a study entitled "Factors Associated with the Fecal Occult Blood Testing for Colorectal Cancer Screening", the results showed that in the referred group, the majority of the subjects were married with higher education and appropriate economic status [15]. There are some systematic reviews entitled "Weight loss as a predictor of cancer in primary care", "A systematic review examining quality of life following pelvic evisceration for locally advanced and recurrent rectal cancer" and "How useful is thrombocytosis in predicting an underlying cancer in primary care" focusing on the CRC [30-32].
Considering the importance of the CRC and the lack of comprehensive systematic reviews in this field led us to review the predictive factors for participating in the CRC screening programs. Indeed, no study included all related factors for prediction of participation in the CRC screening, so that the novelty of this paper is due to its comprehensiveness.
Materials and Methods
Search strategy
International databases including PubMed, ISI and Scopus were considered for search of English articles from year 2000 to 30 December, 2018. Thirty-one published articles were finally entered into the study. Keywords were “colorectal cancer”, “colorectal neoplasm”, “predictor”, “screening”, “FOBT”, “Fecal Immunochemical Test (FIT)”, “education”, “smoking”, “obesity’ or a combination of them in the title/abstracts. For example search strategy in PubMed database was as following with 15079 studies:
(Colorectal cancer [Title/Abstract] OR Colorectal Neoplasm [Title/Abstract]] AND (Predictor [Title/ Abstract] OR Screening [Title/Abstract] OR FOBT [Title/ Abstract] OR FIT [Title/Abstract] OR Education [Title/ Abstract] OR Smoking [Title/Abstract] OR Obesity [Title/ Abstract]]
Selection of articles
After collection of articles of interest, references imported to Endnote software and removed duplicate titles. Then, after browsing titles, studies with irrelevant purpose were removed, and then the remaining studies assessed by two independent investigators.
The selected studies were performed on humans and published in English. The selection process using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA] statement can be seen in Figure 1.
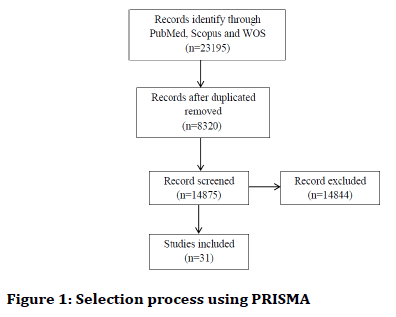
Figure 1. Selection process using PRISMA
Data extraction
Information dealing with the selected articles (the author's last name, year of publication, study design, sample size and the results of each article were taken by two independent investigators.
The differences observed in this process corrected by a third investigator who was independent with the two previous investigators.
Findings
There were 367248 subjects reviewed in this systematic review of 31 published articles consisted of two cohorts, one quasi-experimental, one mixed method, three randomized trial and twenty-six cross-sectional designs.
The summary of the articles included in this review is available in the Table 1.
| Reference | Title | Sample | Age (year) | Design | Conclusion |
|---|---|---|---|---|---|
| Saraste et al. [33] | Initial participation as a predictor for continuous participation in population-based colorectal cancer screening. | 48959 | Range: 60-69 | Cross-sectional | One of the strong predictor to participate in subsequent screening is participation in the first round of screening. |
| Shin et al. [34] | Perceptions of colorectal cancer screening and recommendation behaviors among physicians in Korea. | 379 | Range: 30 to ≥ 65 | Cross-sectional | Strong belief in the screening efficacy of FOBT is very important. |
| Kim et al. [35] | Promoting colorectal cancer screening in foreign-born Chinese-American women: Does racial/ethnic and language concordance matter? | 198 | Range: 50-65 | Quasi-experimental | One of the strong predictor to participate in the screening is education. The effectiveness of the education does not decrease using an interpreter. |
| Nikbakht et al. [36] | Demographic characteristics and the first program of colorectal cancer (CRC) screening in north of Iran | 924 | Mean: 59.38 | Cross-sectional | The prevalence of positive IFOBT increases with age indicating the importance of the screening among elderly population. |
| Juon et al. [37] | Predictors of colorectal cancer knowledge and screening among asian americans aged 50-75 years old. | 274 | Range: 50-75 | Cross-sectional | Lack of the CRC screening knowledge is considered as an important barrier for screening, and it is necessary to increase the knowledge of population. |
| McGuiness et al. [38] | Thinking style as a predictor of men's participation in cancer screening. | 585 | Range: 50-74 | Cross-sectional | The subject "thinking style" about healthy behaviors should be further studied. |
| Ko et al. [39] | The impact of medical tourism on colorectal screening among Korean Americans: A community-based cross-sectional study. | 193 | Range: 50-75 | Community-based, cross-sectional | Medical tourism is related to the CRC screening. |
| Itzhaki [40] | Knowledge and feelings about colorectal cancer among the Jewish adult population in Israel: A mixed methods study. | 196 | Mean: 43.86; SD:15.38 | Mixed method | Increasing knowledge related to CRC is accompanied with reduction in the negative feelings about CRC. |
| Davis et al. [41] | An investigation of the emotion of disgust as an affective barrier to intention to screen for colorectal cancer. | 148 | Range: 40-70 | On-line survey | Evidence indicates fecal disgust can contribute to avoid the screening for CRC. |
| Chouhdari et al. [42] | Association between socioeconomic status and participation in colonoscopy screening program in first degree relatives of colorectal cancer patients. | 200 | Mean: 51.4 | Cross-sectional | Low socioeconomic status contributes the avoidance in the participation of colonoscopy screening program. Also, reduction in the costs of the colonoscopy test is a meaningful priority for policymakers. |
| Hanske et al. [43] | The influence of marital status on the use of breast, cervical, and colorectal cancer screening. | 239,509 | Marrieds: 59.8; Divorced/widowed/separated: 61.6; Single: 58.1 | Cohort | Breast, colorectal, and cervical cancer screening is associated with increased marital status (high in married people). |
| Brittain et al. [44] | African American patients' intent to screen for colorectal cancer: Do cultural factors, health literacy, knowledge, age and gender matter? | 817 | Mean: 57.3; SD: 6.2 | Cross-sectional | Results showed that cultural factors remain important even after emigration to other place. |
| Gupta et al. [45] | Patient trust in physician influences colorectal cancer screening in low-income patients. | 998 | Range: 50-79 | Clustered randomized trial | Trust in PCP is the only meaningful driver for implementation of the CRC screening program in low-income patients. |
| Boguradzka et al. [46] | The effect of primary care physician counseling on participation rate and use of sedation in colonoscopy-based colorectal cancer screening program-A randomized controlled study. | 182 | Range: 50-65 | Randomized trial | PCP's counseling increases the participation rate of colonoscopy screening. |
| Dear et al. [47] | Perception of colorectal cancer risk does not enhance participation in screening. | 234 | Range: 55-74 | Cross-sectional | Health promotion strategies improve knowledge affecting population screening rates. |
| Walter et al. [48] | Impact of age and comorbidity on colorectal cancer screening among older veterans. | 27,068 | Range: 70 to 80> | Cohort | Age is inversely related to the colorectal cancer screening, but comorbidity diseases are a poor predictor. |
| Cole et al. [49] | Psychosocial variables associated with colorectal cancer screening in South Australia. | 894 | Range: 50-69 | Cross-sectional | Non-participation in the FOBT screening is influenced with psychosocial disorders. |
| O'Donnell et al. [50] | Adherence to mammography and colorectal cancer screening in women 50-80 years of age the role of psychological distress. | 905 | Range: 50-80 | Cross-sectional | Psychological disorders contribute the avoidance of people to participate in the screening programs. |
| Curry et al. [51] | Academic detailing to increase colorectal cancer screening by primary care practices in Appalachian Pennsylvania. | 323 | >50 | Multi-site, practice-based, intervention study | Our evidence suggests that academic detailing is acceptable and may be efficacious in increasing recent CRC screening rates in Appalachian practices which could be tested through a randomized controlled study. |
| Walsh et al. [52] | Colorectal cancer screening: What do women from diverse ethnic groups want? | 492 | Range: 50-80 | Cross-sectional | The majority of women are willing to undergo screening for personal benefit. Asians were less likely, and Latinas more likely, to accept colonoscopy. Most are also willing to undergo screening for public health benefit. Self-perceived risk of CRC was the most consistent predictor of willingness and intention to be screened for either personal or public health benefit. |
| Koc et al. [53] | Screening behaviors, health beliefs, and related factors of first-degree relatives of colorectal cancer patients with ongoing treatment in Turkey. | 400 | 37.7 | Cross-sectional | Nurses working with CRC patients must develop strategies to increase FDRs' knowledge of, awareness of, and motivation for CRC screening tests. Risk counseling of FDRs during the treatment period might increase screening rates. |
| Deng et al. [54] | Colorectal cancer screening behavior and willingness: An outpatient survey in China. | 1200 | ≥ 18 | Outpatient-based face-to-face survey | Patient's level of knowledge and income should be taken into consideration when conducting a feasible CRC screening. |
| Ho et al. [55] | The influence of physicians on colorectal cancer screening behavior | 4615 | >75 | Cross-sectional | Contact with physicians and the quality of this interaction are associated with screening behavior. Interventions to improve these provider-related factors may promote CRC screening. |
| Koo et al. [56] | Knowledge of, attitudes toward, and barriers to participation of colorectal cancer screening tests in the Asia-Pacific region: A multicenter study. | 7915 | >50 | Person-to-person interviews | In the Asia-Pacific region, considerable differences were evident in the participation of CRC tests, physician recommendations, and knowledge of, attitudes toward, and barriers to CRC screening. Physician recommendation was the uniform predictor of screening behavior in all countries. Before implementing mass screening programs, improving awareness of CRC and promoting the physicians' role are necessary to increase the screening participation rates. |
| Fisher et al. [57] | Race and colorectal cancer screening: a population-based study in North Carolina. | 598 | Range: 50-59 | Cross-sectional | Ethnicity is not a strong predictor of screening behavior. Age, having a family physician and regular check-up are significant predictors of screening. |
| Gilbert et al. [58] | Colorectal cancer screening: Physician recommendation is influential advice to Marylanders. | 2994 | Range: 50-64 | Cross-sectional | Increasing clinician recommendation for screening is the most practical method to improve colorectal cancer screening. |
| Gili et al. [59] | Psychosocial factors associated with the adherence to a colorectal cancer screening program. | 90 Sibling with CRC | Mean: 61.1; SD:6 | Cross-sectional | Knowledge, social support and advice from health increase the rate of the CRC screening. |
| Carcaise-Edinboro et al. [60] | Influence of patient-provider communication on colorectal cancer screening. | 8488 | <50 | Cross-sectional | The improvement of the communication worldwide increases CRC screening rates. |
| Lian et al. [61] | Geographic variation and effect of area-level poverty rate on colorectal cancer screening. | 4688 | Range: 50-64 | Cross-sectional | Geographic accessibility affects the CRC screening as well as poverty rate, is a main predictor in this regard. |
| Sutton et al. [62] | Predictors of attendance in the United Kingdom flexible sigmoidoscopy screening trial. | 2758 | Range: 27-58 | Cohort | Attitudes and beliefs affect the attendance of people for screening. |
| Sentell et al. [63] | Low health literacy and cancer screening among Chinese Americans in California: A cross-sectional analysis. | 1446 | Range: 21-75 | Population-based survey | LHL and LEP are associated with cancer screening, in spite of the recent physician visit. |
Table 1: The summary of reviewed articles in this systematic study
Discussion
Various risk factors have been reported for colorectal cancer, including age more than 50 years, familial history, nutrition patterns, obesity, inactivity, and cigarette smoking. However, the main cause of it has not been accurately known [9]. The survival rate of the CRC is highly dependent on the time of diagnosis, so secondary prevention, which is the early diagnosis of cancer using screening programs, is important [6,15]. This study aimed to review the predictive factors for participation in colorectal cancer screening.
A study by Wee et al., on the factors associated with the CRC screening from the United States families, found that half of the subjects reported having a history of the CRC screening in the last 10 years. After adjusting age, gender, body mass index, access to health care and national territory, Spaniards were less likely to participate in screening tests than whites and people with less education. However, non-whites and people with less education reported fewer counseling from health care providers to take the screening tests. Of the respondents who did not participate in the FOBT, the most reason was the lack of knowledge, but pain, discomfort and not counseling by a physician were effective. The results also showed that the low prevalence of the CRC screening was due to low awareness and inadequate counseling by health providers about the low screening acceptance of the patients [64].
A review study in the United States was conducted by Beydoun et al. and reviewed the predictive factors for colorectal cancer screening among high-risk individuals (over 50 years of age]. The results showed that the predominant predictive factors for the CRC screening included elderly, male gender, being married, high education level, high income, white race, non-Hispanic ethnicity, history of smoking, history of chronic disease, family history of colorectal cancer, common source care, physician's advice, use of other preventive health services and health insurance coverage. More psychosocial predictors were examined based on the health belief model. The most prominent were the perceived barriers for the CRC screening. Evidence has shown that the CRC screening is a complex behavior with a number of factors including individual characteristics, health insurance coverage, and the relationship between physician and patient [65].
A study was done by Yong et al. on the CRC screening: Obstacles to the FOBT and colonoscopy in Singapore using household survey and home samples. The subjects were aware of colorectal cancer screening methods and interviewed about the screening barriers. Most of the responses to not participate in the CRC screening were having no symptoms for participating in the FOBT, discomfort, having no family history of the CRC, lack of time and lack of reminders or advice. The results showed that the lack of knowledge especially the misconceptions about the lack of signs and health, were identified as the main obstacle to participate in screening [66,67].
Conclusion
According to the findings, several factor are involved to participate people in CRC screening including belief, thinking style, attitude, knowledge, accessibility to screening facilities and geographic variation, participation in the first round of screening with posteducation issues, elderly, fecal disgust, race, low socioeconomic status especially income, being married and female, trust to physician and kindly contact of health providers, counselling centres and psychosocial disorders, in such a way that these factors are effective predictors in the participation of people in the CRC screening programs. Authorities should focus on these factors to promote the health of people by participation in the CRC screening programs.
Conclusion
According to the findings, several factor are involved to participate people in CRC screening including belief, thinking style, attitude, knowledge, accessibility to screening facilities and geographic variation, participation in the first round of screening with posteducation issues, elderly, fecal disgust, race, low socioeconomic status especially income, being married and female, trust to physician and kindly contact of health providers, counselling centres and psychosocial disorders, in such a way that these factors are effective predictors in the participation of people in the CRC screening programs. Authorities should focus on these factors to promote the health of people by participation in the CRC screening programs.
Authors Contributions
All the authors have contributed towards conducting the paper and preparation of the manuscript and they all have approved the latest version of the article.
Ethical Considerations
Ethical issues observed totally by all authors of this study such as plagiarism, double publication and data fabrication.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Micheli A, Coebergh JW, Mugno E, et al. European health systems and cancer care. Ann Oncol 2003; 14:v41-60.
- Arabsalmani M, Mohammadian-Hafshejani A, Ghoncheh M, et al. Incidence and mortality of kidney cancers, and human development index in Asia; A matter of concern. J Nephropathol 2017; 6:30.
- Mousavi MSM, Beladi MSS, Hayati F, et al. The relationship between chronic kidney disease and cancer. J Nephropathol 2018; 7:115-6.
- Nasri H. On the occasion of world cancer day 2018; Breast cancer in geriatric individuals. J Negat Results Clin Exp Stud 2017; 1:e03.
- Salami A, Amiri M. On the occasion of world cancer day 2017; Breast cancer. J Ischemia Tissue Repair 2017; 1.
- Decker KM, Demers AA, Nugent Z, et al. Reducing income-related inequities in colorectal cancer screening: Lessons learned from a retrospective analysis of organised programme and non-programme screening delivery in Winnipeg, Manitoba. BMJ Open 2016; 6:e009470.
- Miles A, van Duijnhoven F, McQueen A, et al. Colorectal cancer: Advances in prevention and early detection. Biomed Res Int 2015; 2015.
- Amiri A, Rkhshany F, Farmanbar R. The Effect of educational program based on BASNEF model on healthy lifestyle of taxi drivers in langroud. JMS THUMS 2014; 1:45-54.
- Derakhshanfar A, Khourshidi H, Niayesh A, et al. Epidemiological study of colorectal cancer at Ekbatan and Besat hospitals of Hamadan during ten years (1998-2008). Iran J Surgery; 18:68-77.
- Akhtar MH, Masud K, Nazar CM, et al. Frequency of colorectal dysplasia and cancer among young patients with ulcerative colitis in a tertiary care hospital. Immunopathol Persa 2016; 3.
- James AS, Campbell MK, Hudson MA. Perceived barriers and benefits to colon cancer screening among African Americans in North Carolina: How does perception relate to screening behavior? Cancer Epidemiol Prev Biomarkers 2002; 11:529-34.
- Ahmadi A, Noroozi M, Pourhoseingholi MA, et al. Effect of metabolic syndrome and its components on survival in colorectal cancer: A prospective study. J Renal Inj Prev 2015; 4:15.
- Esna-Ashari F, Sohrabi MR, Abadi AR, et al. Colorectal cancer prevalence according to survival data in Iran-2007. Iran J Cancer Prev 2009; 2:15-8.
- Mirbazegh SF, Rahnavard Z, Rajabi F. The effect of education on dietary behaviors to prevent cancer in mothers. J Res Health 2012; 2:108-7.
- Salem R, El-Din SS, Shakweer MM, et al. Value of podocalyxin immunohistochemical expression as a prognostic marker in colorectal carcinoma; A clinicopathologic study. Immunopathol Pers 2016; 3.
- Wiwanitkit V. Estimation of cancer risk due to exposure to cadmium contamination in herbal products in Thailand. J Nephropharmacol 2015; 4:81.
- Zeighami S, Azizzadeh E, Tabatabaee HR, et al. Opium and grade of urothelial bladder cancer. J Nephropharmacol 2018; 7.
- Hajibabaei K. The role of antioxidants and pro-oxidants in the prevention and treatment of cancers. Ann Res Antioxid 2016; 1.
- Dizaji RK, Babak R, Mohammad B, et al. Evaluation of serum zinc level as a risk factor for gastrointestinal cancers. Immunopathol Pers 2017; 4.
- World Health Organization. 58th World health assembly approved resolution on Cancer prevention and control WHA 58.22. Geneva, Switzerland: World Health Organization 2005.
- Javadzade SH, Reisi M, Mostafavi F, et al. Factors associated with the fecal occult blood testing for colorectal cancer screening based on health belief model structures in moderate risk individuals, Isfahan, 2011. J Edu Health Promot 2012; 1.
- Anderson JC, Fortinsky RH, Kleppinger A, et al. Predictors of compliance with free endoscopic colorectal cancer screening in uninsured adults. J Gen Intern Med 2011; 26:875-80.
- Hinkle JL, Cheever KH. Study guide for Brunner & Suddarth's textbook of medical-surgical nursing. Lippincott Williams & Wilkins 2013.
- Saito H, Soma Y, Koeda J, et al. Reduction in risk of mortality from colorectal cancer by fecal occult blood screening with immunochemical hemagglutination test. A case‐control study. Int J Cancer 1995; 61:465-9.
- Peterson SK, Vernon SW. A review of patient and physician adherence to colorectal cancer screening guidelines. In Seminars in colon and rectal surgery 2000. Philadelphia, PA: WB Saunders Co., c 1990; 11:58.
- Nasri H. Sudden onset of renal failure requiring dialysis associated with large B-cell lymphoma of colon. J Nephropathol 2012; 1:202.
- Baradaran A. The role of biomarkers to detect progression of diseases. J Negat Results Clin Exp Stud 2017; 1:e05.
- Sani MR, Asadi-Samani M, Shirzad H, et al. Biomarkers in cancer. Immunopharmacogenetics 2019; 1.
- Meissner HI, Yabroff KR, Dodd KW, et al. Are patterns of health behavior associated with cancer screening? Am J Health Promot 2009; 23:168-75.
- Nicholson BD, Hamilton W, O’Sullivan J, et al. Weight loss as a predictor of cancer in primary care: A systematic review and meta-analysis. Br J Gen Pract 2018; 68:e311-22.
- Rausa E, Kelly ME, Bonavina L, et al. A systematic review examining quality of life following pelvic exenteration for locally advanced and recurrent rectal cancer. Colorectal Dis 2017; 19:430-6.
- Bailey SE, Ukoumunne OC, Shephard E, et al. How useful is thrombocytosis in predicting an underlying cancer in primary care? A systematic review. Fam Pract 2016; 34:4-10.
- Saraste D, Öhman DJ, Sventelius M, et al. Initial participation as a predictor for continuous participation in population-based colorectal cancer screening. J Med Screen 2018; 25:126-33.
- Shin HY, Suh M, Park B, et al. Perceptions of colorectal cancer screening and recommendation behaviors among physicians in Korea. BMC Cancer 2017; 17:860.
- Kim K, Quinn M, Lam H. Promoting colorectal cancer screening in foreign-born Chinese-American women: Does racial/ethnic and language concordance matter? J Racial Ethn Health Disparities 2018; 5:1346-53.
- Nikbakht HA, Ghaem H, Shokri-Shirvani J, et al. Demographic characteristics and the first program of colorectal cancer (CRC) screening in north of Iran (2016). J Gastrointest Oncol 2018; 9:458.
- Juon HS, Guo J, Kim J, et al. Predictors of colorectal cancer knowledge and screening among Asian Americans aged 50-75 years old. J Racial Ethn Health Disparities 2018; 5:545-52.
- McGuiness CE, Turnbull D, Wilson C, et al. Thinking style as a predictor of men’s participation in cancer screening. Am J Mens Health 2017; 11:318-29.
- Ko LK, Taylor VM, Yoon J, et al. The impact of medical tourism on colorectal screening among Korean Americans: A community-based cross-sectional study. BMC Cancer 2016; 16:931.
- Itzhaki M. Knowledge and feelings about colorectal cancer among the Jewish adult population in Israel: A mixed methods study. Appl Nurs Res 2018; 43:64-8.
- Davis M, Oaten M, Occhipinti S, et al. An investigation of the emotion of disgust as an affective barrier to intention to screen for colorectal cancer. Eur J Cancer Care 2017; 26:e12582.
- Chouhdari A, Yavari P, Pourhoseingholi MA, et al. Association between socioeconomic status and participation in colonoscopy screening program in first degree relatives of colorectal cancer patients. Iran J Cancer Prev 2016; 9.
- Hanske J, Meyer CP, Sammon JD, et al. The influence of marital status on the use of breast, cervical, and colorectal cancer screening. Prev Med 2016; 89:140-5.
- Brittain K, Christy SM, Rawl SM. African American patients’ intent to screen for colorectal cancer: Do cultural factors, health literacy, knowledge, age and gender matter? J Health Care Poor Underserved 2016; 27:51.
- Gupta S, Brenner AT, Ratanawongsa N, et al. Patient trust in physician influences colorectal cancer screening in low-income patients. Am J Prev Med 2014; 47:417-23.
- Boguradzka A, Wiszniewski M, Kaminski MF, et al. The effect of primary care physician counseling on participation rate and use of sedation in colonoscopy-based colorectal cancer screening program–A randomized controlled study. Scand J Gastroenterol 2014; 49:878-84.
- Dear K, Scott L, Chambers S, et al. Perception of colorectal cancer risk does not enhance participation in screening. Therap Adv Gastroenterol 2008; 1:157-67.
- Walter LC, Lindquist K, Nugent S, et al. Impact of age and comorbidity on colorectal cancer screening among older veterans. Ann Intern Med 2009; 150:465-73.
- Cole SR, Zajac I, Gregory T, et al. Psychosocial variables associated with colorectal cancer screening in South Australia. Int J Behav Med 2011; 18:302-9.
- O'Donnell S, Goldstein B, DiMatteo MR, et al. Adherence to mammography and colorectal cancer screening in women 50–80 years of age: The role of psychological distress. Women's Health Issues 2010; 20:343-9.
- Curry WJ, Lengerich EJ, Kluhsman BC, et al. Academic detailing to increase colorectal cancer screening by primary care practices in Appalachian Pennsylvania. BMC Health Serv Res 2011; 11:112.
- Walsh JM, Kim SE, Sawaya G, et al. Colorectal cancer screening: What do women from diverse ethnic groups want? J Gen Intern Med 2013; 28:239-46.
- Koc S, Esin MN. Screening behaviors, health beliefs, and related factors of first-degree relatives of colorectal cancer patients with ongoing treatment in Turkey. Cancer Nurs 2014; 37:E51-60.
- Deng SX, Gao J, An W, et al. Colorectal cancer screening behavior and willingness: An outpatient survey in China. World J Gastroenterol 2011; 17:3133.
- Ho MY, Lai JY, Cheung WY. The influence of physicians on colorectal cancer screening behavior. Cancer Causes Control 2011; 22:1659.
- Koo JH, Leong RW, Ching J, et al. Knowledge of, attitudes toward, and barriers to participation of colorectal cancer screening tests in the Asia-Pacific region: A multicenter study. Gastrointest Endosc 2012; 76:126-35.
- Fisher DA, Dougherty K, Martin C, et al. Race and colorectal cancer screening: a population-based study in North Carolina. NC Med J 2004; 65:12-5.
- Gilbert A, Kanarek N. Colorectal cancer screening: physician recommendation is influential advice to Marylanders. Prev Med 2005; 41:367-79.
- Gili M, Roca M, Ferrer V, et al. Psychosocial factors associated with the adherence to a colorectal cancer screening program. Cancer Detect Prev 2006; 30:354-60.
- Carcaise-Edinboro P, Bradley CJ. Influence of patient-provider communication on colorectal cancer screening. Medical Care 2008; 46:738-45.
- Lian M, Schootman M, Yun S. Geographic variation and effect of area-level poverty rate on colorectal cancer screening. BMC Pub Health 2008; 8:358.
- Sutton S, Wardle J, Taylor T, et al. Predictors of attendance in the United Kingdom flexible sigmoidoscopy screening trial. J Med Screen 2000; 7:99-104.
- Sentell TL, Tsoh JY, Davis T, et al. Low health literacy and cancer screening among Chinese Americans in California: A cross-sectional analysis. BMJ Open 2015; 5:e006104.
- Wee CC, McCarthy EP, Phillips RS. Factors associated with colon cancer screening: The role of patient factors and physician counseling. Prev Med 2005; 41:23-9.
- Beydoun HA, Beydoun MA. Predictors of colorectal cancer screening behaviors among average-risk older adults in the United States. Cancer Causes Control 2008; 19:339-59.
- Yong SK, Ong WS, Koh GC, et al. Colorectal cancer screening: Barriers to the faecal occult blood test (FOBT) and colonoscopy in Singapore. PSH 2016; 25:207-14.
- Norouzirad R, Khazaei Z, Mousavi M, et al. Epidemiology of common cancers in Dezful county, southwest of Iran. Immunopathol Persa 2017; 4.
Author Info
Shirin Barzanjeh Atri1, Mina Hosseinzadeh2, Mohamad Asghari Jafarabadi3, Mohammad Hasan Sahebihagh4,5 and Leila Ebadi6*
1Faculty of Nursing and Midwifery, Community Health Nursing Department, Tabriz University of Medical Sciences, Tabriz, Iran2Nursing and Midwifery Faculty, Tabriz University of Medical Sciences, Tabriz, Iran
3Road Traffic lnjury Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
4Tabriz Health Services Management Research Center, Health Management and Safety Promotion Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
5Department of Community Health Nursing, Tabriz University of Medical Sciences, Tabriz, Iran
6Community Health Nursing, Tabriz University of Medical Sciences, Tabriz, Iran
Citation: Shirin Barzanjeh Atri, Mina Hosseinzadeh, Mohamad Asghari Jafarabadi, Mohammad Hasan Sahebihagh, Leila Ebadi, Predictive factors for participation in colorectal cancer screening: A systematic review, J Res Med Dent Sci, 2019, 7(2): 109-115
Received: 13-Mar-2019 Accepted: 25-Mar-2019
