Research - (2020) Volume 8, Issue 3
Practices and Attitudes of Dental Practitioners toward Patient Management during the COVID-19 Pandemic in Saudi Arabia
*Correspondence: Abdullah Ali H. Alzahrani, Department of Dental Health, Faculty of Applied Medical Sciences, Albaha University, Saudi Arabia, Email:
Abstract
Background: Exploring practices and attitudes of dental staff toward the COVID-19 pandemic is critically important; however, little is known about this territory of research.
Aim: The aim of this study is, first, to evaluate practices and attitudes of dental practitioners during the COVID-19 outbreak and, second, to examine associations between several demographic characteristics in relation to dental workers’ practices and attitudes in Saudi Arabia.
Materials and Methods: A national dental survey using a pre-designed and validated practices and attitudes electronic questionnaire (PADPs-EQ) was conducted in Saudi Arabia between April and May 2020. Mean PADPs-EQ scores, descriptive analysis, Chi-square test, Fisher’s exact test and correlations between participants’ demographic characteristics and responses were used as appropriate. Data were analyzed using the Statistical Package for the Social Sciences ®software (version 20.0).
Results: A total of 567 participants were included. The overall mean and standard deviation of the PADPs-EQ scores was 74.5 ± 15.2, which indicates a moderate level of participants’ practices and attitudes. All demographic items significantly influenced participants’ practices and attitudes (p<0.0001). Most participants had some critical practices that were not always implemented as suggested by the Saudi Dental Emergency Protocol (SDEP) during the COVID-19 pandemic.
Conclusions: An obvious deficit in implementing the SDEP was observed. Developing effective strategies for improving dentists’ practices and attitudes may be recommended. Emphasis on updating current courses related to preventive dentistry in dental schools and an increasing number of required continuing education hours and workshops related to infection control may also be advocated.
Keywords
Coronavirus, COVID-19, SARS-CoV-2, Dentist, Dental Service
Introduction
The widespread nature of the recent novel coronavirus (COVID-19) has significantly challenged healthcare systems, including dental care delivery, worldwide. Several countries experiencing this pandemic have suspended all regular dental visits and have sought to provide only urgent and emergency dental care [1]. Studies have shown that dental practitioners are at a high risk of exposure to COVID-19 infection due to possible transmission of airborne particles through aerosols produced during dental procedures, indirect transmission through saliva, and close face-to-face contact [2,3]. However, dental practitioners are not only very acquainted with occupational health challenges, including risk assessment, hepatitis B and hepatitis C, but also with universal precautions for cross-infection control [4]. Nonetheless, from the dental public health perspective, those practitioners must not be exposed to unnecessary risk of infection unless they are well trained and experienced in dealing with the COVID-19 outbreak and with some minimalistic dental cases.
Since the first emergence of the COVID-19 in China, there has been a great clinical and medical tendency toward exploring this coronavirus and how to overcome the current pandemic evolution. A recent study has concluded that this coronavirus has not only created an enormous burden to healthcare services, but that healthcare systems globally need to prepare their infrastructure and human resources inorder to control the COVID-19 outbreak [5]. Moreover, the epidemiological aspect of the COVID-19 has also been explored. It was found that the COVID-19 incubation period was likely to be four to six days, while the serial interval was estimated to be four to eight days [6]. Nevertheless, evidence has suggested that controlling the spread of COVID-19 within three months would be possible if case isolation and contact tracing were implemented properly [7].
The nature of the international dental research that has been published in relation to COVID-19 has brought to light several research topics. Some studies have focused on infection control procedures and the implications of delivering dental care during and after the pandemic [8,9]. These studies have concluded that developing further infection control measures and making informed clinical decisions are significantly recommended. Other dental reports have explored the role of saliva and its association in the transmission of COVID-19 [3,10,11]. The urgent need to develop protective measures and implement a strategy to limit human-to-human transmission has been suggested. Furthermore, other studies have examined the impacts of COVID-19 on dental schools and dental education [12,13].
Likewise, nationally in Saudi Arabia, few studies have explored variable aspects of dentistry in relation to COVID-19. For example, Khurshid, et al. [14] suggested exploring the diagnostic opportunity of saliva and its role in the transmission of COVID-19. Two further studies have focused on establishing dental guidelines and precautions for patient management during the COVID-19 outbreak [15,16]. Moreover, Ahmed et al. [17] evaluated dentists’ anxiety while working during the COVID-19 pandemic. Recommendations for dental faculties to update their courses’ learning outcomes and include considerations of pandemics in relation to dentistry were strongly advocated [18]. Interestingly, Javed, et al. [19] carried out a cross-sectional study and found that dental faculty’s staff at Qassim University had insufficient COVID-19 knowledge, particularly in dental procedures that could maintain the health of both dentists and patients.
The Saudi Ministry of Health established its Dental Emergency Protocol (SDEP) for the COVID-19 pandemic in mid-April 2020 [20]. From a dental public health stance, exploring practices and attitudes of dental staff toward the COVID-19 pandemic is critically important. This exploration could not only lead to identifying any possible gaps in dentists’ knowledge and attitudes but also to recognizing potential dental malpractice during the period of the pandemic. Consequently, proposed interventions or strategies to overcome any challenges and obstacles could be developed. However, no studies in the dental literature have examined and explored practices and attitudes of dental practitioners during the COVID-19 pandemic, particularly in Saudi Arabia. Therefore, this study aims first to evaluate practices and attitudes of dental practitioners towards patient management during the COVID-19 outbreak and, second, to examine the associations between several demographic characteristics in relation to dental staff practices and attitudes in Saudi Arabia.
Materials and Methods
Participants and settings
A national dental survey using the Designed Practices and Attitudes of Dental Practitioners Electronic Questionnaire (PADPs-EQ) targeting all dental practitioners who work in Saudi Arabia was conducted between April and May 2020. A simple randomized sampling technique was used to determine the study sample. The statistical information about the demographic details of dental practitioners in the country was obtained from the General Authority for Statistics in Saudi Arabia according to the latest statistical report from 2018 [21]. It was found that the total number of dentists working across the country was 16,736. Considering this number, a margin of error of ± 0.05 and a confidence level of 95%, the necessary sample size for the present study was calculated to be approximately 376 dental practitioners. To compensate for any participant refusal and to improve the engagement response rate, we proposed to recruit more than 500 dental practitioners. Data collection was conducted by distributing the PADPs-EQ through text messages and emails through the heads of Saudi dental centers to all dental practitioners working across Saudi Arabia. All participants completed the proposed informed consent before their participation in this study. Then, the title and purpose of this survey, the subjects’ rights to confidentiality, anonymity and to withdraw from the study were introduced to the participants. After this, all participants went on to fill out the PADPs-EQ.
Practices and Attitudes of Dental Practitioners Electronic Questionnaire (PADPs-EQ)
The PADPs-EQ consists of two key sections. The first section focusses on covering eight demographic items, including job title/rank (academic dental staff, dental consultant, dental specialist and general dental practitioner or GDP); qualification/degree (bachelor, postgraduate, master’s, PhD and board or equivalent); main specialty (restorative dentistry, periodontics, orthodontics, endodontics, prosthodontics, pedodontics, oral surgery and dental public health); nationality (Saudi or non-Saudi); working sector (governmental or private); gender (male or female); level of working experience (less than five years, five to ten years, more than ten years); and working region (13 different regions) in the country. The second section of the PADPs-EQ consists of a set of 22 questions developed based on the SDEP protocol and focusses mainly on evaluating dental practitioners’ practices and attitudes towards patient management, including aspects of viral transmission and dental clinic considerations in addition to the implementation of the infection control protocol during the COVID-19 outbreak.
Participants valued each item in the PADPs- EQ based on whether practices and attitudes were experienced never, very rarely, rarely, occasionally, very frequently or always, coded as 0, 1, 2, 3, 4 or 5, respectively. ‘Never’ indicates a practice or attitude that has never been experienced, ‘very rarely’ indicates a practice or attitude experienced only one time, ‘rarely’ indicates a practice or attitude experienced fewer than three times, ‘occasionally’ indicates a practice or attitude experienced fewer than five times, ‘very frequently’ indicates a practice or attitude experienced more than five times and ‘always’ indicates a practice or attitude that is always experienced. The 22 PADPs-EQ items were recorded for each subject. The mean PADPs-EQ score for each group of demographic items was also calculated. The highest obtainable total score of PADPs-EQ is 101. Participants were consequently classified into three levels based on their mean PADPs-EQ scores: a modest level of practice/attitude (obtaining a score of less than 68), a moderate level of practice/attitude (obtaining a score of less than 84 but above 69) and a professional level of practice/attitude (obtaining a score of more than 85).
The internal consistency of the PADPs-EQ showed robust consistency with estimated, standardized Cronbach’s α=0.84. Table 1 describes correlations between each item of PADPs-EQ, while a reliability analysis including the corrected item-total correlation of the PADPs- EQ items and Cronbach’s alpha coefficients is illustrated in Table 2.
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Q15 | Q16 | Q17 | Q18 | Q19 | Q20 | Q21 | Q22 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | 1 | |||||||||||||||||||||
| Q2 | 0.26 | 1 | ||||||||||||||||||||
| Q3 | 0.31 | 0.18 | 1 | |||||||||||||||||||
| Q4 | 0.29 | 0.26 | 0.36 | 1 | ||||||||||||||||||
| Q5 | 0.13 | -0.08 | 0.27 | 0.15 | 1 | |||||||||||||||||
| Q6 | -0.1 | 0 | 0.27 | 0.04 | 0.22 | 1 | ||||||||||||||||
| Q7 | 0.19 | 0.09 | 0.36 | 0.31 | 0.45 | 0.34 | 1 | |||||||||||||||
| Q8 | 0.48 | 0.09 | 0.39 | 0.23 | 0.22 | 0.2 | 0.31 | 1 | ||||||||||||||
| Q9 | 0.39 | 0.27 | 0.32 | 0.3 | 0.16 | 0.16 | 0.29 | 0.39 | 1 | |||||||||||||
| Q10 | 0.38 | 0.19 | 0.36 | 0.29 | 0.19 | 0.14 | 0.3 | 0.42 | 0.67 | 1 | ||||||||||||
| Q11 | 0.24 | -0.04 | 0.48 | 0.3 | 0.55 | 0.26 | 0.43 | 0.47 | 0.37 | 0.42 | 1 | |||||||||||
| Q12 | 0.2 | 0.21 | 0.24 | 0.41 | 0.16 | 0.01 | 0.21 | 0.22 | 0.19 | 0.1 | 0.27 | 1 | ||||||||||
| Q13 | 0.25 | 0.11 | 0.38 | 0.39 | 0.4 | 0.28 | 0.57 | 0.33 | 0.38 | 0.44 | 0.48 | 0.26 | 1 | |||||||||
| Q14 | 0.17 | 0.21 | 0.18 | 0.37 | 0.19 | 0.07 | 0.13 | 0.22 | 0.42 | 0.27 | 0.12 | 0.45 | 0.34 | 1 | ||||||||
| Q15 | 0.19 | 0.22 | 0.22 | 0.15 | 0.19 | 0.04 | 0.19 | 0.2 | 0.31 | 0.12 | 0.17 | 0.42 | 0.22 | 0.26 | 1 | |||||||
| Q16 | 0.26 | 0.09 | 0.16 | 0.4 | -0.02 | -0.04 | 0.07 | 0.23 | 0.34 | 0.17 | 0.13 | 0.36 | 0.18 | 0.6 | 0.34 | 1 | ||||||
| Q17 | 0.12 | -0.05 | 0.26 | 0.16 | 0.27 | 0.19 | 0.24 | 0.28 | 0.24 | 0.28 | 0.49 | 0.1 | 0.3 | 0 | 0.1 | 0.02 | 1 | |||||
| Q18 | 0.17 | 0.06 | 0.3 | 0.25 | 0.45 | 0.22 | 0.38 | 0.19 | 0.36 | 0.32 | 0.41 | 0.36 | 0.43 | 0.35 | 0.38 | 0.22 | 0.13 | 1 | ||||
| Q19 | -0.05 | 0.05 | -0.02 | 0.13 | 0.04 | 0.11 | 0.11 | -0.12 | -0.11 | -0.09 | 0.02 | 0.14 | 0.09 | -0.02 | -0.09 | 0.04 | -0.08 | 0.15 | 1 | |||
| Q20 | 0.18 | 0.34 | 0.09 | 0.42 | -0.12 | -0.22 | -0.01 | -0.02 | 0.23 | 0.16 | 0 | 0.4 | 0.12 | 0.37 | 0.32 | 0.33 | -0.04 | 0.19 | 0 | 1 | ||
| Q21 | -0.09 | 0.1 | 0.25 | 0.11 | 0.34 | 0.31 | 0.41 | 0.12 | 0.12 | 0.2 | 0.33 | 0.14 | 0.3 | 0.06 | 0.17 | -0.08 | 0.21 | 0.3 | 0.18 | -0.03 | 1 | |
| Q22 | -0.07 | 0.22 | 0.08 | 0.12 | 0.16 | 0.09 | 0.28 | 0.05 | 0.3 | 0.28 | 0.16 | 0.19 | 0.17 | 0.14 | 0.28 | 0.08 | 0.03 | 0.19 | 0.08 | 0.18 | 0.42 | 1 |
Table 1: Correlation between each item of the PADPs-EQ.
| Scale Mean if Item deleted | Cronbach's alpha if item deleted | |
|---|---|---|
| Q1 | 69.96 | 0.838 |
| Q2 | 71.7 | 0.843 |
| Q3 | 70.67 | 0.831 |
| Q4 | 70.81 | 0.831 |
| Q5 | 71.32 | 0.837 |
| Q6 | 70.64 | 0.843 |
| Q7 | 70.06 | 0.834 |
| Q8 | 71.01 | 0.836 |
| Q9 | 69.87 | 0.835 |
| Q10 | 70.19 | 0.833 |
| Q11 | 70.74 | 0.829 |
| Q12 | 71.43 | 0.831 |
| Q13 | 70.95 | 0.826 |
| Q14 | 71.02 | 0.832 |
| Q15 | 71.5 | 0.835 |
| Q16 | 70.91 | 0.837 |
| Q17 | 71.06 | 0.84 |
| Q18 | 71.92 | 0.828 |
| Q19 | 71.44 | 0.853 |
| Q20 | 70.83 | 0.842 |
| Q21 | 72.05 | 0.839 |
| Q22 | 73.59 | 0.842 |
Table 2: Reliability analysis: Corrected item-total correlation of the PADPs-EQ and cronbach’s alpha Coefficients.
Data analysis
Data were analyzed using the Statistical Package for the Social Sciences ®software (version 20.0) (IBM, Armonk, NY). Descriptive analysis was reported using the exact number of observations and related percentages, the mean, and the standard deviation (SD) as appropriate. The Chi-square test and Fisher’s exact test, as well as correlation analysis, were also employed to explore the associations between participants’ demographic characteristics and total score of PADPs-EQ. Statistical significance was set at 0.05.
Ethical consideration
Ethical approval was obtained from the Deanship of Scientific Research at Albaha University in Saudi Arabia (approval number: 1441-41212329).
Results
Participants’ demographic characteristics
A total of 567 dental practitioners from 13 regions of Saudi Arabia participated in this study. Most of those participants were GDPs (n=290, 51.1%). Other practitioners were dental consultants, academic dental staff, and dental specialists (n =112, 19.8%; n=84, 14.8%; and n=81, 14.3%, respectively). The dental practitioners included in this study had not only different genders, nationalities, qualifications/ degrees, dental specialties and job titles/ranks; they also worked in dissimilar sectors and had different lengths of working experience, which highlights the diversity in the sample of this study. The summary of participants’ demographic characteristics is described in Table 3.
| Variable | n (%) | Variable | n (%) |
|---|---|---|---|
| All Participants | 567 (100) | Working Sector | |
| Job's Title/ Rank | Governmental | 427 (75.3) | |
| Academic Dental Staff | 84 (14.8) | Private | 140 (24.7) |
| Dental Consultants | 112 (19.8) | Gender | |
| Dental Specialist | 81 (14.3) | Male | 329 (58) |
| General Dental Practitioner (GDP) | 290 (51.1) | Female | 238 (42) |
| Qualification Degree | Working Experience | ||
| Bachelor degree | 269 (47.4) | Less than five years | 195 (34.4) |
| Postgraduate diploma | 46 (8.1) | Five to ten years | 176 (31) |
| Master degree | 60 (10.6) | More than ten years | 196 (34.6) |
| PhD degree | 72 (12.7) | Working Region/State | |
| Board or equivalent | 120 (21.2) | Al Baha Region | 42 (7.4) |
| Main Speciality | Al Jouf Region | 29 (5.1) | |
| Dental Public Health | 9 (1.6) | Assir Region | 25 (4.4) |
| Endodontics | 101 (17.8) | Eastern Region | 74 (13.1) |
| Oral Surgery | 117 (20.6) | Hail Region | 19 (3.1) |
| Orthodontics | 52 (9.2) | Jazan Region | 31 (5.5) |
| Pedodontics | 32 (5.6) | Madinah Region | 16 (2.8) |
| Periodontics | 55 (9.7) | Makkah Region | 69 (12.2) |
| Prosthodontics | 79 (13.9) | Najran Region | 32 (5.6) |
| Restorative Dentistry | 122 (21.5) | Qassim Region | 24 (4.2) |
| Nationality | Riyadh Region | 176 (31) | |
| Saudi | 390 (68.8) | Tabuk Region | 18 (3.2) |
| Non-Saudi | 177 (31.2) | The Northern Border Region | 12 (2.1) |
Table 3: Summary of the participants demographic characteristics.
Overview of practices and attitudes of dental practitioners and PADPs-EQ responses
In total, 12 out of 22 items of the PADPs-EQ were correctly answered by most of the participants. The remaining 10 PADPs-EQ questions recorded different responses, ranging from modest to moderate practices and attitudes. Moreover, most dental practitioners included in this study reported that they were not only possible susceptible hosts for transmitting COVID-19 but that they also could transmit COVID-19 to their patients, colleagues, families or community members (n=388, 68.4% and n=287, 50.6% respectively). Furthermore, the majority of participated dental workers in this study indicated that they regularly wore new disposable gown with every patient, maintained wearing Personal Protective Equipment (PPE) whenever diagnosing and treating patients, and removed immediately the PPE when leaving the treatment area (n=345, 60.8%; n= 396, 69.8%; and n=357, 63%, respectively). However, the results of this study uncovered that most participants engaged in some practices and attitudes that were not always implemented as suggested by the SDEP protocol. For example, contacting patients remotely to minimize patient contact ‘as necessary’, wearing N95 or higher respirators to perform aerosol-generating procedures and using rubber dam isolation to reduce the generation of aerosols (n=404, 71.3%; n= 432, 76.2%; and n=368, 64.9%, respectively) are recommended.
Most dental staff who participated in this study showed that they always preformed hand hygiene using the World Health Organization five movement of hand hygiene (n=400, 70.5%). Moreover, almost half of the participants stated that they were not only never forgotten to take the standard infection control precautions, but that they also always instructed their patients to use mouth rinse containing oxidative agents as a pre-procedural action (n=287, 50.6%; and n=264, 46.6%, respectively). However interestingly, the minority of dental practitioners reported that they nor always obtained appropriate consents form patients or parents neither always used a four-handed technique and high volume ejector saliva (n= 218, 38.4%; n= 192, 33.9%, respectively).
Although most participants did read the SDEP protocol (n=492, 86.8%), interestingly, most participants did not only report that they cannot always and easily differentiate between the handpieces with or without anti-retraction valves (n=384, 67.7%) but also that they would use dental handpieces without anti-retraction functions during the pandemic (n=366, 64.6%). Nevertheless, some dental practitioners believe that the SDEP protocol neither provides comprehensive knowledge nor covers all specific dental procedures that safeguard both patients and dental staff (n=214, 37.7%). If this is the case, a revision of the SDEP protocol by the local authority [20], might be recommended. A comparison between the participants’ most correct responses and other responses is illustrated in Table 4.
| PADPs-EQ item | Most Correct responses n (%) | Other responses n (%) | |
|---|---|---|---|
| Q1 | Do you think dental practitioners are possibly susceptible hosts for transmitting COVID-19? | 388 (68.4) | 179 (31.6) |
| Q2 | It is impossible that dental practitioners can transform COVID-19 to their patients, colleagues, families or any community member, isn’t it? | 287 (50.6) | 280 (49.4) |
| Q3 | Have you restricted the presence of unnecessary individuals to your clinic? | 293 (51.7) | 274 (43.3) |
| Q4 | If you have decided to undertaking treatment, have an appropriate patient or parents’ consent been obtained? | 218 (38.4) | 349 (61.6) |
| Q5 | If the patient follows up is needed, have you been contacted your patients remotely to minimize patients contact (as necessary)? | 163 (28.7) | 404 (71.3) |
| Q6 | Have you ever forgotten to take the standards infection control precautions while dealing with any patient coming to your clinic? | 287 (50.6) | 280 (49.4) |
| Q7 | Do you regularly wear a new disposable gown with every patient? | 345 (60.8) | 222 (39.2) |
| Q8 | Do you think that all dental staff who had unprotected high-risk exposure or have suggestive symptoms regardless of exposure shall stop performing their duties immediately? | 370 (65.3) | 197 (34.7) |
| Q9 | Have you maintained and worn Personal Protective Equipment (PPE) whenever diagnosing and treating patients in the dental office? | 396 (69.8) | 171 (30.2) |
| Q10 | Have you immediately removed your PPE when leaving treatment areas? | 357 (63) | 210 (37) |
| Q11 | If the patient is suspected, Have you postponed the treatment and report to infection control department? | 306 (54) | 261 (46) |
| Q12 | Have you worn respiratory protection (N95-or higher respirators) for performing aerosol generating procedures? | 135 (23.8) | 432 (76.2) |
| Q13 | If a respirator (N95-or higher respirators) for performing aerosol generating procedures is not available, have you used a combination of a surgical mask and a full-face shield? | 225 (39.7) | 342 (60.3) |
| Q14 | Have you used rubber dam isolation to minimize the generation of aerosol? | 199 (35.1) | 368 (64.9) |
| Q15 | If using rubber dam isolation is not possible, have you used manual devices such as hand scalers for caries removal and periodontal scaling to minimize the generation of aerosol? | 113 (19.9) | 454 (80.1) |
| Q16 | Would you use a four-handed technique, high volume saliva ejectors, and a rubber dam? | 192 (33.9) | 375 (66.1) |
| Q17 | Should patients with suspected or confirmed COVID-19 infection ONLY be treated in negative pressure rooms or negative pressure treatment room/Airborne infection isolation rooms? | 369 (65.1) | 198 (34.9) |
| Q18 | Can you easily differentiate between the handpieces with or without anti-retraction valve? | 183 (32.3) | 384 (67.7) |
| Q19 | Would you use dental hand-pieces without anti-retraction function during the Pandemic period of COVID-19? | 201 (35.4) | 366 (64.6) |
| Q20 | Have you instructed your patients to use mouth rinse containing oxidative agents such as 0.2% as a pre-procedural action? | 264 (46.6) | 303 (53.4) |
| Q21 | Have you performed hand hygiene using the World Health Organization (WHO) my five moments for hand hygiene? | 400 (70.5) | 167 (29.5) |
| Q22 | Have you read the Dental Emergency Protocol during COVID-19 Pandemic that established by the Saudi Ministry of Health [17]? | 492 (86.8) | 75 (13.2) |
Table 4: A comparison between the most correct responses of the participants and other responses.
Association between participants’ demographic characteristics and PADPs-EQ scores
The overall mean and standard deviation of PADPs-EQ scores was 74.5 ± 15.2. Most of the participants showed a moderate level of practices and attitudes, achieving PADPs-EQ scores lower than 84 but above 69. Demographic items included gender, working sector, and nationality were significantly influenced participants’ practices and attitudes. Male participants showed a significantly higher mean PADPs-EQ score than females (76.09 ± 14.68 and 72.22 ± 15.63, respectively, p < 0.003). Furthermore, it was found that participants who worked in the governmental sector achieved significantly higher mean PADPs-EQ scores than those who worked in the private sector (76.91 ± 14.63 and 67.00 ± 14.46, respectively, p<0.0001). Saudi dentists similarly obtained a higher mean PADPs-EQ score than non-Saudis (75.91 ± 15.22 and 71.28 ± 14.68, respectively, p < 0.001).
The findings of this study uncovered that job’s job title/rank, qualification/degree, and main specialty were also significantly influenced practices and attitudes of dental practitioners. Academic dental staff obtained significantly higher mean PADPs-EQ scores than dental consultants, specialists, and GDPs (94.14 ± 4.07, 93.54 ± 5.04, 88.20 ± 3.65, and 90.90 ± 5.32, respectively, p < 0.0001). Moreover, it was found that participants who had a PhD degree achieved significantly higher mean PADPs-EQ scores than those who had bachelor, postgraduate diploma, master, and board or equivalent (93.29 ± 4.19, 90.90 ± 5.32, 88.20 ± 1.79, 88.50 ± 4.47 and 94.38 ± 5.09, respectively, p<0.0001). Likewise, endodontists and oral surgeons acquired significantly higher mean PADPs-EQ scores than those other dental specialties (93.06 ± 5.22 and 91.25 ± 3.69, respectively, p < 0.0001). Table 5 describes the association between participants’ demographic characteristics and PADPs-EQ mean scores. The distribution of the PADPs-EQ mean scores according to modest, moderate and professional levels of participants’ practices/ attitudes is described in Figure 1.
| Job's Title/ Rank | ||||||||
| Academic Dental Staff | 84 (14.8) | 9 (10.7) | 65.22 ± 5.43 | 19 (22.6) | 76.84 ± 3.85 | 56 (66.7) | 94.14 ± 4.07 | |
| Dental Consultants | 112 (19.8) | 22 (19.6) | 60.27 ± 4.47 | 68 (60.7) | 78.18 ± 4.53 | 22 (19.6) | 93.54 ± 5.04 | <0.0001 |
| Dental Specialist | 81 (14.3) | 17 (21) | 55.83 ± 8.16 | 39 (48.1) | 75.90 ± 4.78 | 25 (30.9) | 88.20 ± 3.65 | |
| General Dental Practitioner (GDP) | 290 (51.1) | 112 (38.6) | 54.43 ± 12.78 | 137 (47.2) | 74.94 ± 4.50 | 41 (14.1) | 90.90 ± 5.32 | |
| Qualification Degree | ||||||||
| Bachelor degree | 269 (47.4) | 115 (42.8) | 54.74 ± 12.75 | 113 (42) | 75.66 ± 4.37 | 41 (15.2) | 90.90 ± 5.32 | |
| Postgraduate diploma | 46 (8.1) | 10 (21.7) | 63.00 ± 4.00 | 31 (67.4) | 74.97 ± 5.53 | 5 (10.9) | 88.20 ± 1.79 | <0.0001 |
| Master degree | 60 (10.6) | 12 (20) | 54.66 ± 9.85 | 32 (53.3) | 74.38 ± 3.52 | 16 (26.7) | 88.50 ± 4.47 | |
| PhD degree | 72 (12.7) | 0 (0) | 0 | 16 (22.2) | 79.00 ± 3.65 | 56 (77.8) | 93.29 ± 4.19 | |
| Board or equivalent | 120 (21.2) | 23 (19.2) | 59.87 ± 4.78 | 71 (59.2) | 77.24 ± 4.96 | 26 (21.7) | 94.38 ± 5.09 | |
| Main Speciality | ||||||||
| Dental Public Health | 9 (1.6) | 2 (22.2) | 58.00 ± 9.90 | 7 (77.8) | 80.57 ± 4.28 | 0 (0) | 0 | |
| Endodontics | 101 (17.8) | 22 (21.8) | 59.63 ± 5.81 | 36 (35.6) | 76.22 ± 3.67 | 43 (42.6) | 93.06 ± 5.22 | |
| Oral Surgery | 117 (20.6) | 30 (25.6) | 42.40 ± 15.30 | 55 (47) | 74.90 ± 4.65 | 32 (27.4) | 91.25 ± 3.69 | |
| Orthodontics | 52 (9.2) | 12 (23.1) | 63.00 ± 3.90 | 36 (69.2) | 77.77 ± 5.47 | 4 (7.7) | 91* | <0.0001 |
| Pedodontics | 32 (5.6) | 0 (0) | 0 | 16 (50) | 73.00 ± 3.80 | 16 (50) | 88.00 ± 2.83 | |
| Periodontics | 55 (9.7) | 22 (40) | 52.45 ± 6.46 | 22 (40) | 77.00 ± 4.76 | 11 (20) | 86.90 ± 3.80 | |
| Prosthodontics | 79 (13.9) | 36 (45.6) | 61.22 ± 5.49 | 37 (46.8) | 75.32 ± 4.53 | 6 (7.6) | 90.67 ± 5.68 | |
| Restorative Dentistry | 122 (21.5) | 36 (29.5) | 59.55 ± 9.94 | 54 (44.3) | 76.40 ± 4.34 | 32 (26.2) | 95.88 ± 4.11 | |
| Nationality | ||||||||
| Saudi | 390 (68.8) | 90 (23.1) | 55.73 ± 14.21 | 196 (50.3) | 76.28 ± 4.60 | 104 (26.7) | 92.70 ± 4.52 | |
| Non-Saudi | 177 (31.2) | 70 (39.5) | 56.31 ± 6.93 | 67 (37.9) | 75.40 ± 4.90 | 40 (22.6) | 90.55 ± 5.95 | <0.0001 |
| Working Sector | ||||||||
| Governmental | 427 (75.3) | 84 (19.7) | 55.76 ± 14.78 | 213 (49.9) | 76.32 ± 4.63 | 130 (30.4) | 91.55 ± 4.86 | |
| Private | 140 (24.7) | 76 (54.3) | 56.24 ± 6.47 | 50 (35.7) | 74.92 ± 4.78 | 14 (10) | 97.14 ± 3.61 | <0.0001 |
| Gender | ||||||||
| Male | 329 (58) | 59 (17.9) | 53.54 ± 15.74 | 180 (54.7) | 75.97 ± 4.74 | 90 (27.4) | 91.12 ± 4.69 | |
| Female | 238 (42) | 101 (42.4) | 57.42 ± 7.98 | 83 (34.9) | 76.24 ± 4.58 | 54 (22.7) | 93.72 ± 5.20 | <0.0001 |
| Working Experience | ||||||||
| Less than five years | 195 (34.4) | 102 (52.3) | 52.33 ± 12.48 | 63 (32.3) | 76.29 ± 5.59 | 30 (15.4) | 92.13 ± 5.70 | |
| Five to ten years | 176 (31) | 25 (14.2) | 63.48 ± 5.55 | 89 (50.6) | 75.73 ± 4.26 | 62 (35.2) | 92.09 ± 4.99 | <0.0001 |
| More than ten years | 196 (34.6) | 33 (16.8) | 61.60 ± 5.67 | 111 (56.6) | 76.18 ±4.47 | 52 (26.5) | 92.08 ± 4.76 | |
| Working Region/State | ||||||||
| Al Baha Region | 42 (7.4) | 2 (4.8) | 56* | 25 (59.5) | 77.20 ± 14.25 | 15 (35.7) | 89.33 ± 3.60 | |
| Al Jouf Region | 29 (5.1) | 9 (31) | 64.44 ± 3.20 | 16 (55.2) | 78.13 ± 3.42 | 4 (13.8) | 87.00 ± 1.41 | |
| Assir Region | 25 (4.4) | 8 (32) | 58.00 ±4.28 | 15 (60) | 78.33 ± 5.00 | 2 (8) | 93.50 ± 9.20 | |
| Eastern Region | 74 (13.1) | 25 (33.8) | 57.32 ± 8.71 | 29 (39.2) | 74.62 ± 4.25 | 20 (27) | 93.20 ± 6.53 | |
| Hail Region | 19 (3.1) | 5 (26.3) | 50.40 ± 3.13 | 8 (42.1) | 76.63 ± 3.38 | 6 (31.6) | 90.00 ± 5.25 | |
| Jazan Region | 31 (5.5) | 8 (25.8) | 53.50 ± 5.88 | 14 (45.2) | 76.00 ± 3.72 | 9 (29) | 93.44 ± 4.36 | |
| Madinah Region | 16 (2.8) | 4 (25) | 62* | 12 (75) | 77.66 ± 3.44 | 0 (0) | 0 | |
| Makkah Region | 69 (12.2) | 13 (18.8) | 55.92 ± 4.37 | 36 (52.2) | 73.33 ± 4.85 | 20 (29) | 91.60 ± 6.99 | <0.0001 |
| Najran Region | 32 (5.6) | 8 (25) | 48* | 0 (0) | 0 | 24 (75) | 95.00 ± 4.33 | |
| Qassim Region | 24 (4.2) | 16 (66.7) | 62.00 ± 6.20 | 8 (33.3) | 81* | 0 (0) | 0 | |
| Riyadh Region | 176 (31) | 56 (31.8) | 53.93 ± 16.92 | 88 (50) | 75.64 ± 4.64 | 32 (18.2) | 91.62 ± 4.63 | |
| Tabuk Region | 18 (3.2) | 6 (33.3) | 53* | 6 (33.3) | 84 | 6 (33.3) | 85* | |
| The Northern Border Region | 12 (2.1) | 0 (0) | 0 | 6 (50) | 71* | 6 (50) | 98* | |
† Chi-square associated with p-value calculated for comparison between participants demographic characteristics and total score of PADPs-EQ
Table 5: Association between participants demographic characteristics and PADPs-EQ scores.
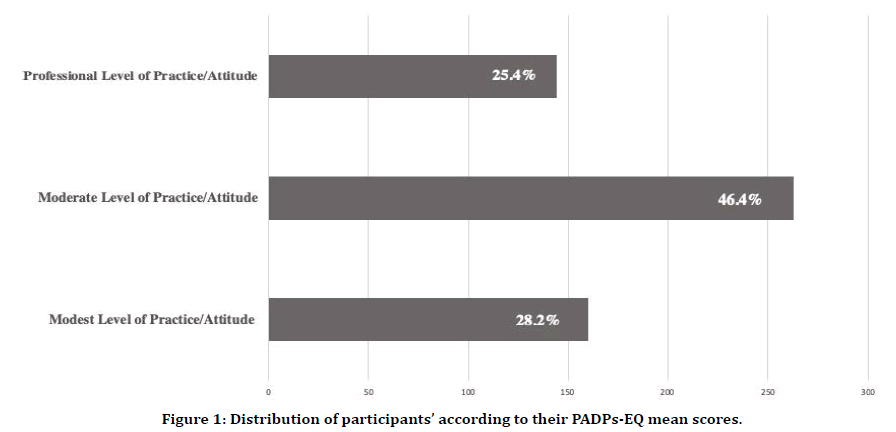
Figure 1. Distribution of participants’ according to their PADPs-EQ mean scores.
Discussion
Most dental practitioners who participated in this study appeared to have moderate levels of practices and attitudes towards patient management during the COVID-19 outbreak in Saudi Arabia. Interestingly, no studies in the dental literature have examined this territory of research, particularly in Saudi Arabia. Instead, most of the research has focused on exploring infection control procedures and implications of delivering dental care during and after the pandemic, the role of saliva and its association in the transmission of COVID-19 and the impacts of COVID-19 on dental schools and education [1,3,10-12]. Therefore, this study could be the first of its kinds to explore and examine not only the practices and attitudes of dental practitioners towards patient management during the COVID-19 outbreak but also the associations between several demographic characteristics in relation to dental staffs’ practices and attitudes in Saudi Arabia.
Our results reveal that dental practitioners show an obvious deficit in the implementation of the SDEP protocol, which may impact the delivery of optimal emergency or urgent dental care during the COVID-19 pandemic. Although the SDEP emphasizes the importance of using rubber dam isolation with every patient during the COVID-19 pandemic, most dentists in this study reported that they did not always use it (n=368, 64.9%). This corroborates other studies that have indicated that the majority of dentists are not using this isolation technique [22,23]. However, evidence has suggested that several challenges may be experienced in using rubber dams, including, but not limited to, the availability of the rubber dam, the time required to place it and the cost of the materials [24]. This may highlight that auditing the use of rubber dams within dental services is still a challenge. However, this malpractice may considerably jeopardize dental care outcomes, particularly during the COVID-19 pandemic.
Using dental handpieces without anti-retraction valves is prohibited by the SDEP protocol [20], and other dental research has also suggested not using these handpieces to prevent any possible cross-infections during the COVID-19 outbreak [2,25]. However, regrettably, only a few dentists in this study reported that they can easily differentiate between the handpieces with or without anti-retraction functions; furthermore, a minority of respondents indicated that they never use handpieces without anti-retraction functions (n=183, 32.3% and n=201, 35.4%, respectively). Nonetheless, evidence has demonstrated that using anti-retraction dental handpieces can pointedly minimize the backflow of hepatitis B virus and bacteria into the tubes of dental units [26]. Hence, to ensure proper and safe delivery of dental care during the COVID-19 pandemic, orientation programs targeting dental practitioners may be recommended, with a clear focus on differentiation between handpieces with or without anti-retraction valves and the prevention of the usage of those without antiretraction functions.
Filtering facepiece respirators, such as the N95 disposable respirator, has been shown to be most frequently used to prevent disease transmission and protect against the inhalation of COVID-19 [27]. Moreover, the SDEP protocol puts a great emphasis on wearing N95 disposable respirators with every patient during the pandemic [20]. However, undesirably, less than a quarter of the participating dentists in the present study indicated that they always wore the N95 respirator (n=135, 23.8%). Additionally, it was uncovered in this study that all the demographic characteristics studied significantly influenced participants’ practices and attitudes (p<0.0001) (Table 5). These findings are consistent with other national and international studies conducted in Saudi Arabia, the United States, France, and Japan [28-31]. Therefore, to enhance the practices of the studied population, developing effective strategies targeted at improving dentists’ infection control practices and attitudes alongside increasing amounts of required continuing education hours and workshops may be advocated.
Exploring the medical and dental literature revealed a revolution of research concerning the COVID-19 and its management [5-13]. However, the exploration of practices and attitudes of dental staff toward the COVID-19 pandemic could not only recognize any dentists’ inappropriate attitudes and malpractices during the period of the pandemic, but that proposed strategies to overcome challenges and obstacles if existed could be intervened. Therefore, it was for this reason that the present study focused on this territory of research.
This study has two key limitations. First, although the sample size of this survey was calculated as only needing 376 participants, the generalizability of the results might be considered as one of the limitations of this study. To overcome this limitation and maximize the sampling’s representation as much as possible, the recruitment was not only targeted to be more than 500 responses but, in addition, participants included in this survey represented various demographic characteristics, emphasising the diversity in the sample of this survey. A second limitation of this survey could be a lack of evaluation of other factors that may contribute to the dentists’ practices and attitudes, such as dentists’ workloads, dentists’ ethnicities, type of provided dental therapy, type of dental visit (routine, urgent, emergent) and time of dental visit. Nevertheless, the emphasis of this study is on evaluating practices and attitudes of dentists during the COVID-19 outbreak and examining associations between several demographic characteristics in relation to dentists’ practices and attitudes in Saudi Arabia.
Conclusion
The overall mean and standard deviation of the PADPs-EQ score was 74.5 ± 15.2, which implies a moderate level of dentists’ practices and attitudes. All demographic characteristics significantly influenced participants’ practices and attitudes (p<0.0001). Moreover, a clear nonadherence to applying the SDEP within the Saudi dental services was detected. In order to deliver safe and proper dental care and enhance dentists’ practices, several actions may be recommended, including the urgent development of an effective strategy or intervention that focusses on improving dentists’ practices and attitudes, emphasizing updating current courses related to preventive dentistry in dental schools and increasing the amount of required continuing education hours and workshops related to infection control, particularly during disease outbreaks.
Conflict Of Interest Statement
The author declares no conflicts of interest regarding the authorship and/or publication of this article.
Availability of Data and Material
The data supporting the findings of the article is available upon request form the main author Dr Alzahrani, email: aahalzahrani@bu.edu.sa.
Funding
This article did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Coulthard P. Dentistry and coronavirus (COVID-19)—moral decision-making. Br Dent J 2020; 228:503-505.
- Peng X, Xu X, Li Y, et al. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci 2020; 12:1-6.
- To KK-W, Tsang OT-Y, Yip CC-Y, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis 2020; 149:1-3.
- Moodley R, Naidoo S, van Wyk J. The prevalence of occupational health-related problems in dentistry: A review of the literature. J Occupa Health 2018; 60:111-125.
- Morales R, Cardona-Ospina AJ, Ocampo JAG, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infectious Dis 2020; 34:1-13.
- Park M, Cook AR, Lim JT, et al. A systematic review of COVID-19 epidemiology based on current evidence. J Clin Med 2020; 9:1-13.
- Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Global Health 2020; 8:e488-e496.
- Volgenant CMC, Persoon IF, de Ruijter RAG, et al. Infection control in dental health care during and after the SARS-CoV-2 outbreak. Oral Dis 2020; 26:1-4.
- Ather A, Patel B, Ruparel NB, et al. Coronavirus Disease 19 (COVID-19): Implications for Clinical Dental Care. J Endod. 2020; 46:584-595.
- Sharma S, Kumar V, Chawla A, et al. Rapid detection of SARS-CoV-2 in saliva: Can an endodontist take the lead in point-of-care COVID-19 testing? Int Endod J 2020; 53:1-3.
- Li Y, Ren B, Peng X, et al. Saliva is a non-negligible factor in the spread of COVID-19. Mol Oral Microbiol. 2020; 35:1-17.
- Iyer P, Aziz K, Ojcius DM. Impact of COVID-19 on dental education in the United States. J Dent Educ. 2020; 84:16-23.
- Ghai S. Are dental schools adequately preparing dental students to face outbreaks of infectious diseases such as COVID-19? J Dent Educ 2020; 84:24-31.
- Khurshid Z, Asiri FYI, Al Wadaani H. Human saliva: Non-invasive fluid for detecting novel coronavirus (2019-nCoV). Int J Environ Res Public Health 2020; 17:2225.
- Alharbi A, Alharbi S, Alqaidi S. Guidelines for dental care provision during the COVID-19 pandemic. Saudi Dent J 2020; 32:181-186.
- Turkistani KA. Precautions and recommendations for orthodontic settings during the COVID-19 outbreak: A review. Am J Orthod Dentofacial Orthop 2020; 157:591-598.
- Ahmed MA, Jouhar R, Ahmed N, et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) Outbreak. Int J Environ Res Public Health 2020; 17:2821.
- Odeh ND, Babkair H, Abu-Hammad S, et al. COVID-19: Present and future challenges for dental practice. Int J Environ Res Public Health 2020; 17:3151.
- Javed MQ, Khan AM, Nawabi S. Dental faculty’s knowledge and attitude regarding COVID-19 disease in Qassim, Saudi Arabia. Res Square 2020; 1.
- https://www.moh.gov.sa/Ministry/MediaCenter/Publications/Documents/MOH-Dental-emergency-guidline.pdf
- https://www.stats.gov.sa/en/1009
- ALI A, Aslam A, Rehman B, et al. Rubber dam use by general dental practitioners: Prevalence and obstacles to its use. Pakistan Oral Dent J 2016; 36:468-471.
- Zou H, Li Y, Lian X, et al. Frequency and influencing factors of rubber dam usage in Tianjin: A questionnaire survey. Int J Dent 2016; 2016:1-7.
- Gilbert GH, Litaker MS, Pihlstrom DJ, et al. Rubber dam use during routine operative dentistry procedures: Findings from the dental PBRN. Oper Dent 2010; 35:491-499.
- Tiwari RVC. Dental considerations in Corona Virus Infections: First review in literature. J Advan Med Dent Sci Res 2020; 8:100-103.
- Hu T, Li G, Zuo Y, et al. Risk of hepatitis B virus transmission via dental handpieces and evaluation of an antisuction device for prevention of transmission. Infect Contr Hospi Epidemiol 2007; 28:80-82.
- Umer F, Haji Z, Zafar K. Role of respirators in controlling the spread of novel coronavirus (Covid-19) among dental health care providers: A review. Int Endod J 2020; 53:1-7.
- Althomairy SA, Baseer MA, Assery M, et al. Knowledge and attitude of dental health professionals about middle east respiratory syndrome in Saudi Arabia. J Int Soc Prev Community Dent 2018; 8:137-144.
- Cleveland JL, Foster M, Barker L, et al. Advancing infection control in dental care settings: Factors associated with dentists' implementation of guidelines from the centers for disease control and prevention. J Am Dent Assoc 2012; 143:1127-1138.
- Doméjean S, Léger S, Simon A, et al. Knowledge, opinions and practices of French general practitioners in the assessment of caries risk: Results of a national survey. Clin Oral Investig. 2017; 21:653-663.
- Kakudate N, Yokoyama Y, Sumida F, et al. Use of clinical practice guidelines by dentists: Findings from the Japanese dental practice-based research network. J Eval Clin Pract 2017; 23:96-101.
Author Info
Department of Dental Health, Faculty of Applied Medical Sciences, Albaha University, Albaha, Saudi ArabiaCitation: Abdullah Ali H. Alzahrani, Practices and Attitudes of Dental Practitioners toward Patient Management during the COVID-19 Pandemic in Saudi Arabia, J Res Med Dent Sci, 2020, 8 (3):214-223.
Received: 25-Feb-2020 Accepted: 10-Jun-2020 Published: 15-Jun-2020
