Review Article - (2023) Volume 11, Issue 2
Platelet Rich Fibrin: The Most Reliable and Autologous Biomaterial
Ritika Rathi1*, Bhairavi Kale2 and Anjali Borle3
*Correspondence: Dr. Ritika Rathi, Department of Dental Surgery, Datta Meghe Institute of Medical Sciences, Maharashtra, India, Email:
Abstract
PRF is an autologous biomaterial made up of cytokines and growth factors encapsulated within a fibrin network. It contains fibrous sealing characteristics with growth factors to create a perfect environment for tissue regeneration and wound healing. It has recently been used in dentistry by a variety of specialties in a huge variety of therapeutic techniques. The current literature review seeks to describe the important research on the approach of using Platelet rich fibrin in therapeutic interventions, with a focus on its formulation, benefits, and drawbacks. Because this is a non-intrusive technology with comparative ease and excellent clinical outcomes, PRF alone or in collaboration with other biopolymers appears to offer numerous benefits and uses in dentistry and medicine.
Keywords
Platelet rich fibrin, Platelet rich plasma, Autologous biomaterial
Introduction
To increase the healing process and also manage the inflammation, bioactive surgical additives were introduced. Healing also is such a complicated process that still we are unable to understand it completely but the fact is well known that platelets are the principal in both wound healing and hemostatic processes. Also it’s been noted that thrombocytes are second most prevalent cells found in the body fluid. Their lifespan is 7 to 10 days. They are basically cell fragments that lack the core that is derived from megakaryocytes. PRF is mainly has homogenous WBCs-platelet rich fibrin matrix, that contains a four molecule structure, along with thrombocytes, cytokines progenitors are present, which functions as an environment friendly scaffold that increments the evolution of the capillaries and vessels and can arrange epithelial cell migration to its surface [1].
PRF possesses immunological and antimicrobial capabilities, may cause leukocyte degranulation, and contains cytokines as it may stimulate revascularization and anti-inflammatory reactions, according. In practically all fields of dentistry, platelet rich fibrin is commonly employed. Several studies on platelet rich fibrin have recently been published and several situations involving the utilization of platelet rich fibrin clots and platelet rich fibrin membranes have been described. The majority of study focuses on platelet rich fibrin in oral surgery foravulsion sockets, sinus lifts, bone augmentation and periodontics forgingival recession, intrabony defects, guided bone regeneration and repair and periapical lesions, among other applications. It’s also been employed in, regenerative pulpotomies, open apex and periapical operations among other procedures [2].
Literature Review
In the 70’s, it was believed that platelets contain certain growth factors which have the potential to augment collagen production, cell mitosis, angiogenesis, engaging additional cells to arrive at the damage site as well as cell differentiation. Then later in 1997, became the first person to present the great advantages in the use of platelet-rich plasma in oral surgery as it was believed that PRF intensified the osteoblasts found in the bone of host and the bone transplant. On the other hand there were various risks associated with platelet rich plasma as it was handled by usingbovine thrombin is thought to produce antibodies against coagulation factors V, XI, and thrombin, which can cause coagulopathies and pose a lethal threat. Also, established Platelet rich fibrin in 2001, primarily in oral and maxillofacial surgery. PRF is now known as the next generation thrombocyte concentrate, and it is also thought to have anti-inflammatory properties and have more efficacy than platelet rich plasma as it has easier preparation and there is no need of any chemical interference to the blood. Hence it is entirely anhomogenousmixture [3].
Protocol for platelet rich fibrin preparation
According to the protocol for preparation of platelet rich fibrin thrombocytes and liberated cytokines are assembled in fibrin clot. PRF protocol needs only centrifuged blood with no anticoagulant or bovine thrombin was used. After that, a hematological sample is obtained with coagulant in 10 mL glass coated plastic tube and centrifuged for 10 minutes at 3,000 rpm [4].
The product obtained contains below 3 layers:
• Upper-most layer consists cellular plasma.
• Platelet rich fibrin clot below it.
• Red blood cells at the lower most layers.
Following the formation of these three layers, the platelet rich fibrin clot must be placed in a disinfected container for few minutes to let correct serum release that is present within. Described squeezing a clot between two sterile gauzes or in a particular machine to turn it into a membrane [5]. Fibrinogen is initially collected in the top portion of the tube without first being altered to fibrin by the appropriate thrombin. Coagulation starts immediately as it interacts with the glass because there is no anticoagulant present. Interaction with a glass surface is needed to start the clotting polymerization reaction. Only dry silica coated plastic tubes can be utilized in this technique. In addition, unlike bovine thrombin, which is employed to prepare platelet rich plasma, silica particles provide no cytotoxicity risk [6].
Ultimately, platelets have confined mostly in the fibrin network. Henceforth, for a useful formation of platelet rich fibrin, faster collection of blood andinstant subsequent centrifugation prior to the initial clotting events is unavoidable. A clinically viable platelet rich fibrin clot requires quick management (Figure 1) [7].
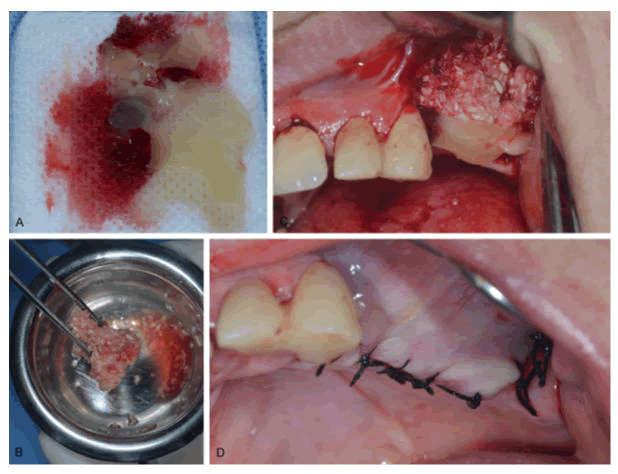
Figure 1: This image depicts the clinical relevance during a horizontal bone augmentation procedure A) For serum release, form a platelet-rich fibrin clot insterile gauze; B) Allograft clot containing PRF; C) PRF+allograft placement in the alveolar ridge to increase width. Over the bone graft, notice the platelet rich fibrin layer; D) This is the final suture. Because the mucosal margins could be bonded in this situation, it was not required to reveal the platelet-rich fibrin membrane layer.
Current applications of platelet rich fibrin in dentistry
In oral and maxillofacial surgery: According to recent research, PRF can be utilized as a restoration in extracted cavities because it acts as a durable blood clot that promotes the development of new capillaries and accelerates tissue healing. This can help individuals who are immunocompromised or diabetic heal their wounds faster. Furthermore, because platelet rich fibrin induces both clotting (with thrombospondin) and woundhealing, it can be utilized as a complement to anticoagulant medication in patients. In sinus lift treatments, platelet rich fibrin has becoming increasingly extensively employed. According to some studies, platelet rich fibrin could be used as one of the sole filler materials during sinus lift and implantation [8].
When the bony margins of avulsion sockets are undamaged, filling them with platelet rich fibrin produces excellent outcomes. In remaining defects where one or more margins are absent or obliterated, an amalgamation of platelet rich fibrin with bone replacements and additional adjuncts may be required to enable adequate bone volume restoration. Because fibrin acts as a physiologic sealant between wound tissues, platelet rich fibrin improves integrity between graft components [9].
In periodontics: platelet rich fibrin has been utilized to treat periapical lesions, intra-bony defects, gingival recession in periodontics. Inflammatory bowel illness may be treated with an amalgamation of PRF gel, hydroxyapatite graft and GTR layer, according to some research papers. In additional trials, PRF gel and PRF layer were used in conjunction with a bone graft to cure a tooth with a mixed periodontics-endodontic lesion. In certain investigations, the lesion is covered with double layer of platelet rich fibrin membrane. White blood cells and thrombocyte aggregates are thought to be coagulated at the membrane's end because the membranes are exceedingly thin and non-homogeneous. To limit the dissolution of the delicate layer and to permit the complete operating site to be revealed to the very same substances, double layer membrane in separate directions are used widely (white blood cells and platelet concentrates).
The below methods can help platelet rich fibrin enhance bony defect repair. Platelet rich fibrin additionally generates growth factors including fibrin growth element and converting growth factor, both of which stimulate wound healing [10].
In endodontic: Multiple studies have indicated that PRF can be employed as a scaffolding substance in a diseased necrotic juvenile tooth for pulp rejuvenation and to resurrect a non-vital tooth. In addition, in instances with extensive periodontal diseases, the combination of platelet rich fibrin membrane as a lattice and mineral trioxide aggregate in specification treatments has proven to be an efficient replacement for constructing artificial root end boundaries and producing rapid periodontal repair. The need of a membrane can restrict substance from being extruded. Platelet rich fibrin can also be utilized in rejuvenating pulpotomy operations, where the pulp is excised and the pulpal lesion is treated with platelet rich fibrin before being sealed with mineral trioxide aggregate and glass incomer cement. After periodontal procedures like root end removal, platelet rich fibrin has also been utilized to clog up bone deformities (Figure 2) [11].
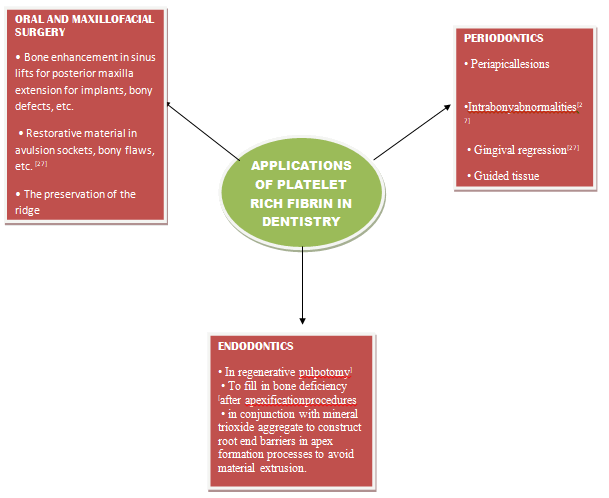
Figure 2: Applications of platelet rich fibrin in dentistry.
Platelet rich fibrin could be a good choice for reperfusion of pulp necrosis in immature permanent teeth because it includes a lot of growth factors that promote cellular differentiation and proliferation while also acting as a scaffold for tissue ingrowth. The prospective theory behind the fruitful use of platelet rich fibrin for open apex rejuvenation can be attributed to Huang et al's study, which found that platelet rich fibrin induces multiplication of Pulp Cells and raises protein concentrations as these Pulp Cells differentiate into odontoblast-like cells [12].
Discussion
Advantages of platelet rich fibrin
The following are some of the benefits of using platelet rich fibrin that have been mentioned in the literature:
• Its synthesis is a simple and effective approach, with centrifugation in just one step that is free and openly applicable to all practitioners.
• Allogenic blood sample can be used to get it.
• Modification of blood is lessening.
• It has an organic fibrin network with growth factors that can remain active for longer durations and drive tissue creation effectively.
• According to the indication, it can be utilised separately or in conjunction with bone grafts.
• The rate of bone graft healing has improved.
• When utilised in conjunction with bone grafts, it is a more cost-effective and time-saving choice than mutant tissue factor.
• When used as a membrane, it reduces the need for a donor site surgical procedure, resulting in less patient suffering during the beginning phases of wound closure.
• In comparison to platelet rich plasma, investigations show that platelet rich fibrin is more effective and has a lower level of controversy in terms of ultimate clinical findings.
• InjectablePRF has many benefits such as it is available as one entity or it can also be amalgamated with certain other biomaterials and it also reduces the risk of side effects [13].
Advantages of platelet rich fibrin over platelet rich plasma
• Platelet rich fibrin can be made in a simple and costeffective manner.
• platelet rich fibrin's gradual biological polymerization on interaction with the test tube's glass particles leads in physiologic thrombin content, but platelet rich plasma's fibrin polymerization is accelerated based upon quantity of operative supplements (thrombin and calcium chloride).
• Platelet-rich fibrin is beneficial to the immune system.
• Hemostasis is aided by platelet rich fibrin.
• An in situ investigation found that PRF is superior to PRP in relation with alkaline phosphatase activity and mineralization induction, which is driven mostly by TGF-1 and PDGF-AB production.
• Injectable Platelet rich plasma also has various disadvantages such as it requires proper centrifugation equipment, a large amount of blood sample is drawn and also the person must limit himself from doing routine activities for a few days [14].
Disadvantages of platelet rich fibrin
Platelet rich fibrin may have the following drawbacks:
• Since it is it homologos blood, the exact figure availa ble is modest
• The platelet rich fibrin protocol's efficiency rate is directly proportional to the management, which is mostly dependent on blood collection time and transferring to the centrifuge.
• To enable clot polymerization, a glass-coated tube is required.
• A probable denial of therapy due to the blood sample punctures.
• Platelet rich fibrin processing requires only a modest amount of physician expertise.
• There have been no studies on the use of autologous platelet rich fibrin in conjunction with a bone graft to correct furcation deformities [15].
Other clinical applications
• Other potential uses for platelet rich fibrin have been reported in the literature, including.
• Obtaining a probing depth decrease and radiographic fault covers in periodontal bone defects.
• The surgical sites of the third molars were reported to be responsible for 90% of osteitisdecrease in localized osteitis.
• Upon obtaining a free gingival graft, as a supplement to palatal wound healing.
• Within the alveolar defect, bone regrowth surrounds proximal implants.
• After cancer surgery, prominent deformities can be repaired.
• Platelet rich fibrin clots are frequently used to fill voids in plastic surgery or combined with a fat cell graft in a lip structure.
• Platelet rich fibrin matrix contains enough of growth factors which encourage healing of wound, therefore it is commonly used for treating trophic ulcer.
• Homogeneous platelet rich fibrin is also indicated in any other research for therapeutic use in increased size intrabony defects in different healthy disciplines in order to brace fruitful results [16].
Conclusion
The indication of PRF in various departments of dentistry such as oral surgery, periodontics and endodontic have shown promising results. It is one of the most successful approaches that can be used to correct oral maxillofacial surgery, prosthetic dentistry, and bone abnormalities in periodontics. Along with this, platelet rich fibrin has also demonstrated tremendous outcomes in the regeneration of pulp-dentin complex in the endodontic procedures. On the other hand also, the majority of the trials have yielded just short-term results. More of these controlled investigations with superior persistent outcomes are required to gain a better understanding of the effective and credible biomaterial over time and to progress its application in daily procedures. Histological investigations are necessary parallel to these medical examinations to explore more types of currently generated tissue in the wound as well as to learn exactly the biology, efficiency, and the technique of using platelet rich fibrin.
References
- Dohan DM, Choukroun J, Diss A, et al. Platelet-Rich Fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101:37-44.
[Crossref] [Google Scholar] [PubMed]
- Singer AJ, Clark RA. Cutaneous wound healing. New Eng J Med 1999; 341:738-746.
[Crossref] [Google Scholar] [PubMed]
- Gabling VL, Acil Y, Springer IN, et al. Platelet-rich plasma and platelet-rich fibrin in human cell culture. Oral Surg Oral Med Oral Pathol Oral Radiol End 2009; 108:48-55.
[Crossref] [Google Scholar] [PubMed]
- Harrison P. Platelet function analysis. Blood Rev 2005; 19:111-123.
[Crossref] [Google Scholar] [PubMed]
- Castro HC, Ferreira BL, Nagashima T, et al. Platelets: Still a therapeutical target. J Brasil de Patol Med Lab 2006; 42:321-332.
- Fernandez-Delgado N, Hernandez-Ramirez, Forrellat-Barrios M. Platelet functional spectrum: From hemostasis to regenerative medicine. Rev Cubana Hemat Inmunol Hemot 2012; 28:200-216.
- Gupta V, Bains VK, Singh GP, et al. Regenerative potential of platelet rich fibrin in dentistry: Literature review. Asian J Oral Health Allied Sci 2011;1:23-8.
- Dohan DM, Choukroun J, Diss A, et al. Platelet-Rich Fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Sur Oral Med Oral Pathol Oral Radiol Endodontol 2006; 101:45-50.
[Crossref] [Google Scholar] [PubMed]
- Choukroun J, Diss A, Simonpieri A, et al. Platelet-Rich Fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2006; 101:56-60.
[Crossref] [Google Scholar] [PubMed]
- Li Q, Pan S, Dangaria SJ, et al. Platelet-rich fibrin promotes periodontal regeneration and enhances alveolar bone augmentation. Bio Med Res Int 2013; 2013.
[Crossref] [Google Scholar] [PubMed]
- Dohan DM, Choukroun J, Diss A, et al. Platelet-Rich Fibrin (PRF): A second-generation platelet concentrate. Part III: Leucocyte activation: A new feature for platelet concentrates? Oral Sur Oral Med Oral Pathol Oral Radiol Endodontol 2006; 101:e51-e55.
[Crossref] [Google Scholar] [PubMed]
- Chang YC, Zhao JH. Effects of platelet Arich fibrin on human periodontal ligament fibroblasts and application for periodontal infrabony defects. Aus Dent J 2011; 56:365-371.
[Crossref] [Google Scholar] [PubMed]
- Kawase T, Kamiya M, Kobayashi M, et al. The heat Âcompression technique for the conversion of plateletâ?ÂÂrich fibrin preparation to a barrier membrane with a reduced rate of biodegradation. J Bio Mat Res 2015; 103:825-831.
[Crossref] [Google Scholar] [PubMed]
- Wu CL, Lee SS, Tsai CH, et al. Platelet rich fibrin increases cell attachment, proliferation and collagenâ?ÂÂrelated protein expression of human osteoblasts. Aus Dent J 2012; 57:207-212.
[Crossref] [Google Scholar] [PubMed]
- Saluja H, Dehane V, Mahindra U. Platelet-Rich fibrin: A second generation platelet concentrate and a new friend of oral and maxillofacial surgeons. Ann Maxillofac Surg 2011; 1:53.
[Crossref] [Google Scholar] [PubMed]
- Bolukbasi N, ErsanlAAS, Keklikoglu N, et al. Sinus augmentation with platelet-rich fibrin in combination with bovine bone graft versus bovine bone graft in combination with collagen membrane. J Oral Implantol 2015; 41:586-595.
[Crossref] [Google Scholar] [PubMed]
Author Info
Ritika Rathi1*, Bhairavi Kale2 and Anjali Borle3
1Department of Dental Surgery, Datta Meghe Institute of Medical Sciences, Maharashtra, India2Department of Periodontics, Datta Meghe Institute of Medical Sciences, Maharashtra, India
3Department of Prosthodontics, Datta Meghe Institute of Medical Sciences, Maharashtra, India
Citation: Ritika Rathi, Bhairavi Kale, Anjali Borle, Platelet Rich Fibrin: The Most Reliable and Autologous Biomaterial, J Res Med Dent Sci, 2023, 11 (02): 016-020.
Received: 15-Nov-2021, Manuscript No. JRMDS-21-47377; , Pre QC No. JRMDS-21-47377(PQ); Editor assigned: 18-Nov-2021, Pre QC No. JRMDS-21-47377(PQ); Reviewed: 02-Dec-2021, QC No. JRMDS-21-47377; Revised: 31-Jan-2023, Manuscript No. JRMDS-21-47377(R); Published: 28-Feb-2023
