Research - (2021) Volume 9, Issue 10
Pharmacotherapy Prescribed for Oral Candidiasis in an Outpatient Population-An Institutional Study
Deepika R and Lakshminarayanan Arivarasu*
*Correspondence: Lakshminarayanan Arivarasu, Saveetha Dental College & Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University, India, Email:
Abstract
Introduction: Oral candidiasis is one of the most common human opportunistic fungal infections caused by C.albicans of the oral cavity. The incidence of candidiasis is associated with some predisposing factors that include the use of dentures, xerostomia, and prolonged therapy with Antibiotics and found as a major clinical feature with HIV. This pathology has a wide variety of treatments which has been studied until these days. Objective: The aim of this study is to evaluate the prevalence of drugs prescribed for candidiasis patients in an outpatient population. Materials and methods: A cross sectional study was conducted among 67 candidiasis patients at the clinic of Saveetha dental college. The data was collected from Dias and is statistically analysed using spss software. Results and discussion: From the results obtained we conclude that males are more prone to candidiasis than females (68.66%) due to the predisposing factors and causes. The drugs commonly prescribed for candidiasis were clotrimazole (64.18%) as a topical antifungal drug than amphotericin B (4.48) and fluconazole (46.27%) as a systemic antifungal drug than ketoconazole due to their benefits. Conclusion: The study provides the prevalence of oral candidiasis among the out patients and assesses the drug of choice for the treatment of oral candidiasis .Thus this study may guide to establish a better clinical approach and helps in assessing the treatment of choice for oral candidiasis.
Keywords
Clotrimazole, Fluconazole, Ketoconazole, Oral candidiasis, Pharmacotherapy
Introduction
Oral candidiasis is one of the most common human opportunistic fungal infections caused by Candida albicans of the oral cavity. The oral Candidiasis can also be termed as oral thrush [1]. Candida albicans (C. albicans) represents around 80% of contaminations and they tend to build as colonies either alone or as groups with other species, including Candida glabrata and Candida tropicalis [2]. The oral candidiasis is commonly seen among children, people with immune deficiency and those who use steroid sprays for asthma [3]. The incidence of candidiasis is also associated with some predisposing factors that include the use of denture wearers, xerostomia, smoking, poor oral hygiene maintenance, prolonged therapy with Antibiotics, and patients under the medication of immunosuppressive agents for a long period [4]. The oral candidiasis is normally characterised by creamy whitish patches seen on the buccal cheek region, tongue, tonsils and sometimes over the palatal region of the oral cavity [5]. People with oral candidiasis may also experience bad breath, burning mouth syndrome, dryness, abnormality of taste, difficulty in swallowing, or redness. It is acknowledged that the histopathological evidence of a given clinical feature, can also provide an exact evaluation of the findings [6]. Candidiasis is typically mild and rarely causes serious problems [7]. But in people with weakened immune systems, it can spread to other parts of the body and cause potentially serious complications. Candidiasis is found as a major clinical feature with HIV [8]. This pathology has a wide variety of treatments which has been studied until recently. Candidiasis in the mouth, throat, or esophagus is usually treated with antifungal medications. These medications include clotrimazole, fluconazole, miconazole, or nystatin [9].
Previous studies have also mentioned that candida species cause oral thrush when a patient's host immunity becomes disrupted which is due to the local, secondary to oral corticosteroid use [10]. The candidiasis has to be confirmed histopathologically as to differentiate from other clinical diagnoses such as oral hairy leukoplakia, angioedema, aphthous stomatitis, herpes gingivostomatitis, herpes labialis, measles (Koplik spots), Steven-Johnsons syndrome, histiocytosis, blastomycosis, lymphohistiocytosis, syphilis and streptococcal pharyngitis was highlighted by Ashman in his article [11,12]. A study by Aun suggested that oral candidiasis prevalent in immunocompetent host, can lead to certain complication that incorporate dysphagia, respiratory distress and candida esophagitis, which is particularly a common complication of oral candidiasis in those with HIV/AIDS [13].
The lacunae of this study include the sample size which was taken within a limited geographical area. The other factors also include that there is no restriction of age mentioned and the study only concentrated on the people who were affected with Candidiasis .The challenges faced also include that patients are restricted to a geographic location, being an institutional study in an outpatient population. In some cases, the external factors can also cause an impact and safety measures have to be ensured for prevention. Our team has extensive knowledge and research experience that has translate into high quality publications [14–33]. Thus the aim of the study was to evaluate the prevalence of drugs prescribed for candidiasis patients in an outpatient population.
Material and Method
A cross sectional study was conducted in an outpatient patient population of Saveetha dental college, Chennai, India. Ethical approval was obtained from the international review board prior to the start of the study. The study consists of one reviewer, one accessor and one guide.
Inclusion criteria:
This study included the patients who reported to Saveetha dental college with Candidiasis.
Exclusion criteria:
The patients reported with other dental complications and maxillofacial surgery was also excluded from this study.
Sampling technique
The study was based on a random sampling method. To minimise the sampling bias all the cases were reviewed properly and included.
Data collection and tabulation
Data collection was done using the patient database with the time frame work of 1 January 2020 to February 2021. The data was obtained from DIAS (Dental information Archiving software), after assessment in the university patient data registry, case records of 67 patients clinically diagnosed with Candidiasis were included and evaluated in the study. Cross verification of the data was done by the reviewer. The collection data was tabulated based on the following parameters:
• Patient chief complaint –Candidiasis.
• Medications prescribed for those patients.
• Review of those patients.
Statistical analysis
The collected data was compiled using excel and data analysis was carried out using SPSS software version 21. Chi square test was used for test associations between categorical variables. Variables were expressed in terms of frequency, percentage, bar graphs were plotted and the p value < than 0.05 was considered as significant.
Results
Results are explained through Figures (Figures 1 to Figure 3).
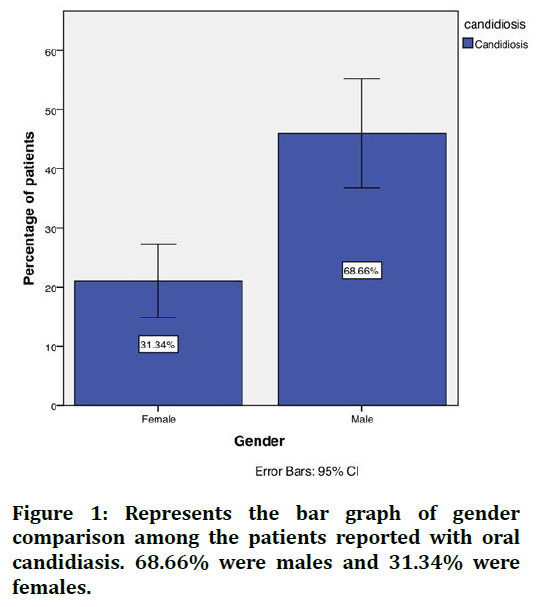
Figure 1. Represents the bar graph of gender comparison among the patients reported with oral candidiasis. 68.66% were males and 31.34% were females.
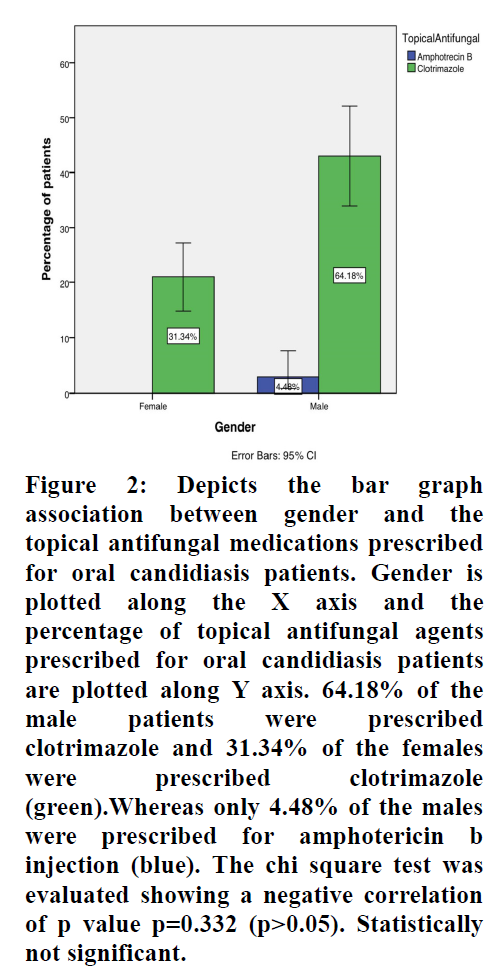
Figure 2. Depicts the bar graph association between gender and the topical antifungal medications prescribed for oral candidiasis patients. Gender is plotted along the X axis and the percentage of topical antifungal agents prescribed for oral candidiasis patients are plotted along Y axis. 64.18% of the male patients were prescribed clotrimazole and 31.34% of the females were prescribed clotrimazole (green).Whereas only 4.48% of the males were prescribed for amphotericin b injection (blue). The chi square test was evaluated showing a negative correlation of p value p=0.332 (p>0.05). Statistically not significant.
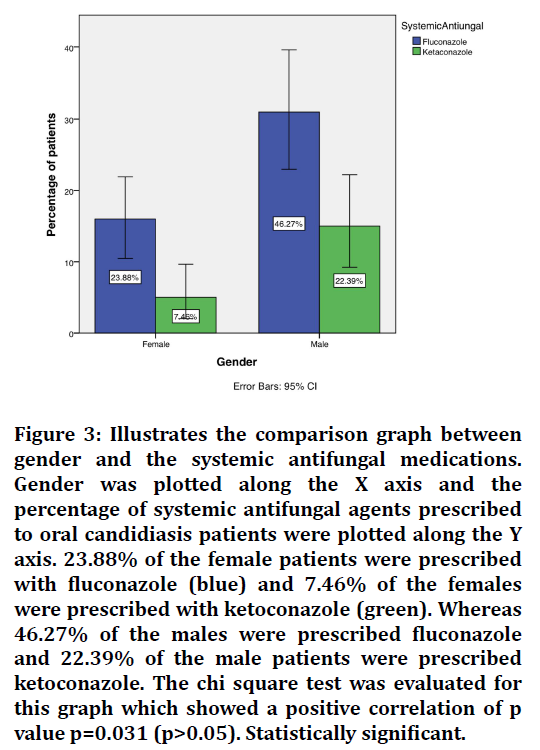
Figure 3. Illustrates the comparison graph between gender and the systemic antifungal medications. Gender was plotted along the X axis and the percentage of systemic antifungal agents prescribed to oral candidiasis patients were plotted along the Y axis. 23.88% of the female patients were prescribed with fluconazole (blue) and 7.46% of the females were prescribed with ketoconazole (green). Whereas 46.27% of the males were prescribed fluconazole and 22.39% of the male patients were prescribed ketoconazole. The chi square test was evaluated for this graph which showed a positive correlation of p value p=0.031 (p>0.05). Statistically significant.
Discussion
From the results we observe that males (68.66%) were prevalently affected with oral candidiasis than females (31.34%). Males have been more commonly involved with habits such as smoking, drinking, poor oral hygiene maintenance, minimum visit to dentists and sometimes due to their drug intake that causes immunosuppression. This proves to be a major risk and thus owing to oral candidiasis prevalent among males [34]. The patients with oral candidiasis have to be treated effectively to prevent the recurrence of the infection. As a topical antifungal agent it was found that clotrimazole (64.18%) was the most predominant medication prescribed among the patients. Clotrimazole lozenge is absorbed by the body and begins to treat oral thrush within 30 to 60 minutes after taking the dose by the patients. Most patients begin to feel relief in about a week, but it takes 2 weeks to completely get rid of the fungus causing your infection [35,36]. Many studies also suggest clotrimazole as the most common drug to prescribe for oral candidiasis than the oral drugs such as miconazole, or nystatin [37]. The systemic antifungal medications commonly prescribed include fluconazole (46.27%) and ketoconazole (22.39%). Many authors have focused on evaluating the efficacy and safety of fluconazole oral solution for the treatment of oropharyngeal candidiasis, especially pseudomembranous type. Further, when dealing with immunocompromised patients, such as HIVinfected, or cancerous patients, fluconazole and ketoconazole drugs have good effects when doubling the dose [38]. The dose was individualized for each patient depending on the severity and type of candidiasis. In recent years many dentists prescribe chlorhexidine mouthwashes along with antifungal agents [39]. Chlorhexidine works as an antimicrobial agent and also helps in preventing Candida species [40]. In addition the dentist has to ensure the predisposing factors of a patient reporting for dental treatment, also proper oral hygiene instructions along with instructing them to remove the dentures at night and placing in water, thereby will benefit the removal of the biofilm layer generated in the prosthetic surface. Thus, Regular oral and dental hygiene with periodic oral examination will prevent most cases of oral candidiasis, so it is needed to make the patient aware of oral hygiene measures.
Conclusion
From this study we observe that oral candidiasis is more prevalent among the males in the study population. Clotrimazole and fluconazole were found to be the most common drugs prescribed with less adverse effects for the treatment of oral candidiasis. Hence preventive measures, campaigns and dental awareness have to be created among the common people to control and resist the occurrence of the oral candidiasis. Thus this study may guide to establish a better clinical approach and helps in assessing the treatment of choice for oral candidiasis.
References
- Miceli MH, Díaz JA, Lee SA. Emerging opportunistic yeast infections. Lancet Infect Dis 2011; 11:142-51.
- Pfaller MA, Pappas PG, Wingard JR. Invasive fungal pathogens: Current epidemiological trends. Clin Infect Dis 2006; 43:3-14.
- Al-Daamy AA, Abd-Al Ameer H, Zuher H. Antifungal activity of propolis against dermatophytes and Candida albicans isolated from human mouth. J Contemp Med Sci 2015; 1:4-8.
- Coronado-Castellote L, Jiménez-Soriano Y. Clinical and microbiological diagnosis of oral candidiasis. J Clin Exp Dent 2013; 5:e279.
- Patil S, Rao RS, Majumdar B, et al. Clinical appearance of oral Candida infection and therapeutic strategies. Front. Microbiol 2015; 6:1391.
- Jaisankar AI, Arivarasu L. Free radical scavenging and anti-inflammatory activity of chlorogenic acid mediated silver nanoparticle. J Pharm Res Int 2020; 106–112.
- Epstein JB. Antifungal therapy in oropharyngeal mycotic infections. Oral Surg Oral Med Oral Pathol 1990; 69:32-41.
- Guida RA. Candidiasis of the oropharynx and esophagus. Ear Nose Throat J 1988; 67:832-840.
- https://books.google.co.in/books/about/Candida_and_Candidosis.html?hl=&id=LKNrAAAAMAAJ&redir_esc=y
- larkson JE, Worthington HV, Eden OB. Interventions for preventing oral candidiasis for patients with cancer receiving treatment. Cochrane Database Syst Rev 2007; CD003807.
- Ashman RB, Farah CS. Oral candidiasis: Clinical manifestations and cellular adaptive host responses. Fungal Immunol 2005; 59-83.
- Karthik V, Arivarasu L, Rajeshkumar S. Hyaluronic acid mediated zinc nanoparticles against oral pathogens and its cytotoxic potential. J Pharm Res Int 2020; 113-117.
- Crawford B, Kasmidi M, Korompis F, et al. Factors influencing progress in establishing community-based marine protected areas in Indonesia. Coast Manag 2006; 34:39-64.
- Rajeshkumar S, Kumar SV, Ramaiah A, et al. Biosynthesis of zinc oxide nanoparticles using Mangifera indica leaves and evaluation of their antioxidant and cytotoxic properties in lung cancer (A549) cells. Enzyme Microb Technol 2018; 117:91-95.
- Nandhini NT, Rajeshkumar S, Mythili S. The possible mechanism of eco-friendly synthesized nanoparticles on hazardous dyes degradation. Biocatal Agric Biotechnol 2019; 19:101138.
- Vairavel M, Devaraj E, Shanmugam R. An eco-friendly synthesis of Enterococcus sp.–mediated gold nanoparticle induces cytotoxicity in human colorectal cancer cells. Environ Sci Pollut Res 2020; 27:8166-8175.
- Rajkumar PV, Prakasam A, Rajeshkumar S, et al. Green synthesis of silver nanoparticles using Gymnema sylvestre leaf extract and evaluation of its antibacterial activity. S Afr J Chem Eng 2020; 32:1-4.
- Rajasekaran S, Damodharan D, Gopal K, et al. Collective influence of 1-decanol addition, injection pressure and EGR on diesel engine characteristics fueled with diesel/LDPE oil blends. Fuel 2020; 277:118166.
- Santhoshkumar J, Sowmya B, Venkat Kumar S, et al. Toxicology evaluation and antidermatophytic activity of silver nanoparticles synthesized using leaf extract of Passiflora caerulea. S Afr J Chem Eng 2019; 29:17–23.
- Raj R K. β‐Sitosterol‐assisted silver nanoparticles activates Nrf2 and triggers mitochondrial apoptosis via oxidative stress in human hepatocellular cancer cell line. J Biomed Mater Res A 2020; 108:1899-908.
- Saravanan M, Arokiyaraj S, Lakshmi T, et al. Synthesis of silver nanoparticles from Phenerochaete chrysosporium (MTCC-787) and their antibacterial activity against human pathogenic bacteria. Microb Pathog 2018; 117:68-72.
- Gheena S, Ezhilarasan D. Syringic acid triggers reactive oxygen species–mediated cytotoxicity in HepG2 cells. Hum Exp Toxicol 2019; 38:694-702.
- Ezhilarasan D, Sokal E, Najimi M. Hepatic fibrosis: It is time to go with hepatic stellate cell-specific therapeutic targets. HBPD Int 2018; 17:192-197.
- Ezhilarasan D. Oxidative stress is bane in chronic liver diseases: Clinical and experimental perspective. Arab J Gastroenterol 2018; 19:56-64.
- Gomathi AC, Rajarathinam SX, Sadiq AM, et al. Anticancer activity of silver nanoparticles synthesized using aqueous fruit shell extract of Tamarindus indica on MCF-7 human breast cancer cell line. J Drug Deliv Sci Technol 2020; 55:101376.
- Dua K, Wadhwa R, Singhvi G, et al. The potential of siRNA based drug delivery in respiratory disorders: Recent advances and progress. Drug Dev Res 2019; 80:714-30.
- Ramesh A, Varghese S, Jayakumar ND, et al. Comparative estimation of sulfiredoxin levels between chronic periodontitis and healthy patients–A case‐control study. J Periodontol 2018; 89:1241-1248.
- Yan H, Yu C. Repair of full-thickness cartilage defects with cells of different origin in a rabbit model. Arthroscopy 2007; 23:178-187.
- Joseph B, Prasanth CS. Is photodynamic therapy a viable antiviral weapon against COVID-19 in Dentistry? Letter to the editor. Oral Surg Oral Med Oral Pathol Oral Radiol 2021.
- Ezhilarasan D, Apoorva VS, Ashok Vardhan N. Syzygium cumini extract induced reactive oxygen species‐mediated apoptosis in human oral squamous carcinoma cells. J Oral Pathol Med 2019; 48:115-121.
- Duraisamy R, Krishnan CS, Ramasubramanian H, et al. Compatibility of nonoriginal abutments with implants: Evaluation of microgap at the implant–Abutment interface, with original and nonoriginal abutments. Implant Dent 2019; 28:289-295.
- Gnanavel V, Roopan SM, Rajeshkumar S. Aquaculture: An overview of chemical ecology of seaweeds (food species) in natural products. Aquaculture 2019; 507:1-6.
- Markov A, Thangavelu L, Aravindhan S, et al. Mesenchymal stem/stromal cells as a valuable source for the treatment of immune-mediated disorders. Stem Cell Res Ther 2021; 12:1-30.
- Cannon RD, Holmes AR, Mason AB, et al. Oral Candida: Clearance, colonization, or candidiasis?. J Dent Res 1995; 74:1152-1161.
- Rodloff AC, Koch D, Schaumann R. Epidemiology and antifungal resistance in invasive candidiasis. Eur J Med Res 2011; 16:187-195.
- Shankar SB, Arivarasu L, Rajeshkumar S. Biosynthesis of hydroxy citric acid mediated zinc nanoparticles and its antioxidant and cytotoxic activity. J Pharm Res Int 2020; 108-112.
- Williams D, Silva SC, Malic S et al. Candida biofilms and oral candidosis: Treatment and prevention. Periodontol 2011; 55:250-265.
- Abu-Elteen KH, Abu-Alteen RM. The prevalence of Candida albicans populations in the mouths of complete denture wearers. New Microbiol 1998; 21:41-48.
- Varshini A, Arivarasu L. Herbal sources used by the public against infections. Int J Pharm Res 2020; 84-92.
- Shree MK, Arivarasu L, Rajeshkumar S. Cytotoxicity and antimicrobial activity of chromium picolinate mediated zinc oxide nanoparticle. J Pharm Res Int 2020; 28-32.
Author Info
Deepika R and Lakshminarayanan Arivarasu*
Saveetha Dental College & Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, IndiaCitation: Deepika R, Lakshmi Narayanan, Pharmacotherapy Prescribed for Oral Candidiasis in an Outpatient Population-An Institutional Study, J Res Med Dent Sci, 2021, 9(10): 194-198
Received: 09-Sep-2021 Accepted: 12-Oct-0021
