Research - (2020) Volume 8, Issue 3
Perioperative Management of Suspected/Confirmed cases of COVID-19 in the Indian Scenario
Manasij Mitra1*, Maitraye Basu2 and Sudipta Chandra3
*Correspondence: Manasij Mitra, Department of Anesthesiology, MGM Medical College and LSK Hospital, Purab Palli, Kishanganj, Bihar, India, Email:
Abstract
The novel coronavirus, 2019-nCoV (COVID-19) a zoonotic virus is transmitted during unprotected close contact from an infected individual through droplets and fomites. The COVID-19 poses tremendous challenge for the healthcare sector globally. Anesthesiologists are at a higher risk than healthcare professionals of any other speciality because they manoeuvre the airway and ventilation and perform a whole gamut of aerosol generating procedures. Moreover, with all the emergency patients who need surgery being considered as suspects of COVID-19 under the present circumstances, there is an urgent need for development of safe medical practices and infection prevention protocol for the perioperative management of patients with COVID-19. In resource limited settings like India, where the government hospitals and the large private healthcare providers are struggling to provide adequate PPE, with many anesthesiologists working in small hospitals, it is all the more important to customise the existing guidelines according to the available infrastructure keeping the basic rationale of the precautions intact. Modifications in airway management and anesthesia practise are required to minimise aerosol generation. Regional anaesthesia should be the preferred choice wherever possible. Planned perioperative care can minimise disease transmission. Crisis capacity Strategies as per CDC recommendations to ensure smooth supply and use of Personal Protective Equipment in resource limited settings is necessary.
Keywords
COVID-19, Coronavirus, Personal protective equipment, Aerosol generating procedures
Introduction
In China, since December 2019, a novel coronavirus, 2019-nCoV, emerged as the causative agent for a collection of viral pneumonia cases. On December 30, 2019, real time PCR (RTPCR) assays of three bronchoalveolar lavage samples from a pneumonia patient of unknown etiology as per the “surveillance definition” subsequent to the SARS outbreak of 2002- 2003, in the Wuhan Jinyintan Hospital in China turned positive for a pan-Betacoronavirus. The whole genome sequence of the virus was acquired using Illumina and nanopore sequencing and subsequent bioinformatics analysis revealed that the virus had similarity with the coronavirus family and belong to the Betacoronavirus 2B lineage with closest simulation with bat SARS-like coronavirus strain BatCoV RaTG13 [1,2]. The virus was also found to have similarity with the Middle East Respiratory Syndrome (MERS-CoV) but is distinct from it as well [3].
The COVID-19 is a single-strand, positive-sense RNA virus with estimated basic reproduction number (R0) signifying number of cases generated after exposure to one patient, in the initial outbreak stage under variable host and environmental factors to be between 2.2 to 3.6. This is like SARS-CoV but higher than MERS-CoV [4]. Based on reported data, the case fatality rate was approximately 2% [5]. This is less than SARSCoV which is approximately 10% and MERS-CoV which is approximately 40% but much higher than the pH1N1 2009 which is approximately 0.026% [6-8].
Ever, since its emergence in Wuhan, China in end December 2019, COVID-19 virus spread rapidly with cases being soon reported from Hubei (outside Yuhan) and China (outside Hubei). By March 11, 2020, it was declared as a pandemic by the World Health Organization [9].
As on date, globally, there are 1,698,626 confirmed cases with 102,773 deaths from COVID-19 [10]. According to the Ministry of Health and Family Welfare, Government of India, the scenario in the country as on 17 April 2020, 17:00 GMT+5:30 is 11,616 active cases with 452 deaths. The worst hit states are Maharashtra, Delhi, Tamil Nadu, Kerala, Rajasthan, Telengana, Andhra Pradesh, Uttar Pradesh and Madhya Pradesh [11].
COVID-19, a zoonotic virus. Is transmitted during unprotected close contact from an infected individual through droplets and fomites. Air-borne transmission for COVID 19 has not been reported though it is presumed that aerosol generating procedures as done in healthcare facilities can promote transmission. Fecal shedding with viable virus though has been reported in a few case reports but feco-oral route of transmission has not been reported as on date [1,12].
As COVID-19 is a new pathogen, without any pre-existing immunity in humans, every individual is assumed to be susceptible though certain risk factors are presumed to increase the susceptibility. The morphology of the COVID-19 virus is depicted in Figure 1A and 1B. Mortality increases with age >60 years with highest mortality among aged >80 years and patients with comorbidities like diabetes, cardiovascular diseases, chronic respiratory disease and immunocompromised conditions like malignancy, CKD. Males also reported a higher crude fatality rate than females which may be due to the higher rates of infection among males which may be due to their increased risk of exposure [1].
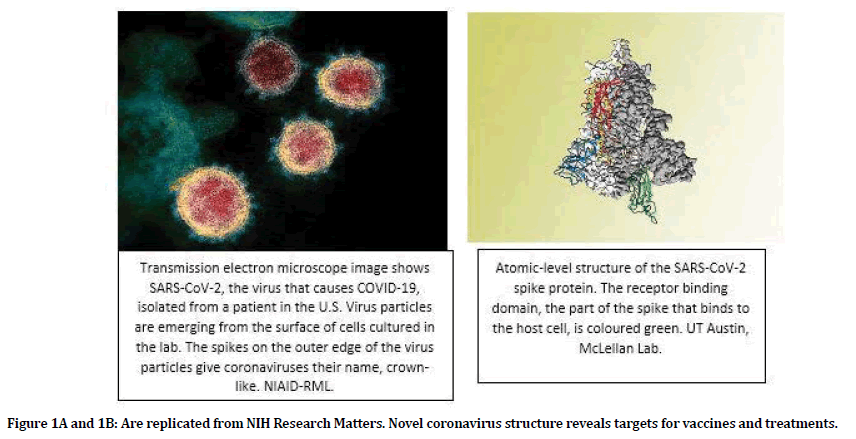
Figure 1A and 1B: Are replicated from NIH Research Matters. Novel coronavirus structure reveals targets for vaccines and treatments.
The clinical presentation of COVID-19 is like SARS, with flu-like symptoms like fever, cough and shortness of breath signified as mild to moderate disease in 80% of the laboratory confirmed cases. Severe and critical disease represented as acute respiratory failure, septic shock with multiorgan dysfunction/failure representing the remaining 14% and 6% patients respectively. However, patients with atypical symptoms like abdominal symptoms have also been noted [1].
The COVID-19 poses tremendous challenge for the healthcare sector globally. Healthcare workers are not only at an increased risk of being infected but also can spread the infection as well.
Anaesthesiologists may encounter and care for patients with COVID-19 in their roles as experts in emergent airway management in intensive care and perioperative anesthesia. Anesthesiologists are at a higher risk than healthcare professionals of any other speciality because they manoeuvre the airway and ventilation. This necessitates that the Anesthesiologist is adjacent to the airway of patients during emergency airway intubation outside the operating room while taking care of critically ill patients in the intensive care settings and providing perioperative care for patients undergoing emergency surgeries [12].
Anesthesiologists have been infected with this deadly virus but the exact figures are unknown. Moreover, with all the emergency patients who need surgery being considered as suspects of COVID-19 under the present circumstances, there is an urgent need for development of safe medical practices and infection prevention protocol for the perioperative management of patients with COVID-19.
Specific guidelines for Anesthesiologists for handling suspected/confirmed COVID 19 cases have been published by World Federation of Anesthesiologists (WFSA) and American Society of Anesthesiologists (ASA).
In resource limited settings like India, where the government hospitals and the large private healthcare providers are struggling to provide adequate PPE, with many anesthesiologists working in small hospitals, it is all the more important to customise the guidelines according to the available infrastructure keeping the basic rationale of the precautions intact.
Thus, considering the huge population of India, inadequacy of healthcare providers and more so, Personal Protective Equipment (PPEs), our topic assembling all the standard guidelines along with its practical application in the Indian Scenario is all the more relevant in the current situation.
The need of systematic training on hospital infection control can be beneficial. With restrictions in close contact and with the diverse nature of settings in which anesthesiologists work in this part of the country, trainings imparted through the Digital Platform can be a good and effective way. The training module should include how to implement standard prevention protocol and apply correct isolation and protective measures in order to safely provide care to the patients but also specific prevention practices for them. Regular interactions and counselling sessions with minimal person to person contact utilising the digital platform can help boost the morale and ensure better compliance to the protective measures circumventing the hurdles through discussions and support from peer groups.
According to WHO recommendations, fit tested N95 (P2) respirators, eye protection, gown, gloves and caps are a must for aerosol generating procedures like intubation, extubation, fibreoptic bronchoscopy, bag and mask ventilation, CPR, oral and nasal suction, high flow nasal cannulation and non-invasive ventilation which are significant for anesthesiologists [13].
Aerosol-generating procedures (AGP) demand employing airborne precautions as these tend to generate minute droplets <5 microns in size which can travel further (>1 metre) and stay suspended in air longer duration compared to larger droplets [14].
It is recommended that aerosol generating procedures should be done in Airborne Infection Isolation Room (AIIR). Powered Air Purifying Respirators (PAPR) have a higher protective factor compared with N95 respirators, but there is no definitive evidence that PAPRs reduce the likelihood of viral transmission [15].
Regional anesthesia should be the preferred choice. However, even for regional anesthesia, the patient should wear a mask preferably N95, avoidance of high flow nasal cannula, use of pencil point needles for spinal anesthesia and needless to mention hand hygiene before and after the procedure are the standard recommendations. Use droplet and contact level precautions at the minimum, bearing in mind, the possibility of conversion to general anesthesia if regional anesthesia fails [16,17].
However, the procedures that demand general anesthesia are really challenging. Modifications are aerosol generation and optimisation of respiratory condition of COVID-19 suspected patients and all guidelines aim toward the same [18].
Pre-anesthetic assessment
Pre-anesthetic assessment should be done as per standard anesthesia guidelines using appropriate PPE and hand hygiene performed after the same. The importance is on airway assessment and respiratory system. Chest X-ray should be done to rule out respiratory complications of COVID-19.
Before intubation
The following should be practised:
Integrity of N95 should be tested, only the persons associated with intubation should be inside the operating room. In the absence of PARPs, the C-arm covers may be used. Insertion of bacterial/viral filter to the expiratory limb of the breathing circuit apart from heat and moisture exchanger is recommended [19].
All airway gadgets need to be keep ready for smooth intubation.
Pre-oxygenation for 5 minutes with minimal gas flow at <6 litres/min to reduce aerosol generation is recommended.
No more than three persons, the intubating anesthesiologists, one person assisting the anesthesiologists during intubation and another for administering medications should be in close vicinity of the patient.
Induction of Anesthesia
Following are the practice recommendations during Induction with an aim to minimise aerosol generation and smooth intubation:
Avoidance of hemodynamic alteration. In high risk patients, vasopressor agents should be ready beforehand for administration to avoid any precipitous fall in blood pressure after administering anesthesia drugs
Slow pre-medication with Intravenous Fentanyl to avoid cough.
Slow induction is recommended. Intravenous Etomidate or Intravenous Ketamine should be used in appropriate cases.
Use of Intravenous Succinylcholine at 1.5 mg/Kg or Intravenous Rocuronium at 1.0-1.2 mg/Kg if Sugammadex is available.
Use of Endotracheal Tube (ETT) of appropriate size with provision for subglottic suction port is recommended.
No positive pressure ventilation should be started before inflation of the endotracheal tube cuff.
Rapid or Ultra-rapid sequence intubation by the most experienced anesthesiologist preferably in the first attempt as quick as possible (<15 seconds) in the operation theatre.
Use of video laryngoscope is preferred as it reduces the proximity of the patient’s airway and the anesthesiologists and increases the chances of successful intubation in difficult airways. Difficult intubation cart should always be ready as failed intubation increased the chances of aerosol generation and viral contamination.
The aim should be avoidance of Bag and Mask ventilation as much as possible
Intubation to be confirmed by observing chest movement and ETCO2. Chest auscultation should be avoided as aerosols generated during intubation tend to contaminate the chest region.
In case of difficulty in intubation or failed intubation, Bag and Mask ventilation with two hands technique involving two persons for better seal and less aerosol generation to be practised. Use of oropharyngeal/nasopharyngeal airway should be done and preferably second generation supraglottic device should be applied directly.
Maintenance of anesthesia
Tube and circuit disconnection to be avoided.
Use of closed suctioning system and lung protective ventilators is recommended.
Aim should be to maintain tidal volume at 5-6 litres/Kg, increase respiratory rate and to keep peak airway pressure below 30 mm Hg.
Emergence from anesthesia
Anti-emetics should be used to minimise vomiting.
Smooth emergence and extubation to be ensured.
Post-operative management
Confirmed COVID 19 patients to be kept in an isolation operating theatre for post anesthesia care followed by direct shifting to the isolation unit as planned. Patients with suspected COVID 19 infections can be observed in the recovery area with cohorting in a corner maintaining atleast one metre distance with other patients. Surgical mask to be applied to all patients in the recovery room [20].
High flow O2, Non-Invasive Ventilation (NIV) or nebulisation unless it is lifesaving should be avoided.
Equipment wherever possible should be disposable for confirmed/suspected COVID 19 patients. All other used equipment needs to be disinfected as per laid down guidelines.
High touch surfaces on the anesthesia machine and anesthesia work area need to be cleaned and disinfected with an Environmental Protection Agency (EPA) approved disinfectant as in Table 1.
| Agent | Concentration | Contact Time Period |
|---|---|---|
| Sodium hypochlorite | 1.00% | 1 min |
| Ethanol | 62-71% | 1 min |
| Hydrogen peroxide | 0.50% | 1 min |
| Povidone iodine | 0.23%-7.5% | 1 min |
Table 1: Effective disinfectants against coronavirus [21,22].
Obstetric anesthesia
In addition to the recommendations above, the following are the special safeguards required:
Regional anesthesia unless contraindicated in the choice [23].
Separation of the mother from the newborn temporarily while diagnostic testing of the mother is being performed is recommended to avoid transmission from mother to newborn. In is in view of the transmission after birth via contact with infectious respiratory secretions though currently there is no evidence of vertical transmission taking place [24,25].
Modifications in CPR
Any resuscitation attempt should be considered as aerosol generating [26].
Early intubation in the resuscitation process with an aim to secure and isolate the airway and possible aerosol generation.
Chest compressions to be kept on hold temporarily during intubation to reduce the risk of inhaling infective aerosol by the intubating clinician [27].
Personal protective equipment
The intubating anesthesiologist and the team assisting the anesthesiologist should use the following PPE like hospital scrubs inside and protective coveralls outside; medical protective mask, disposable surgical cap, and goggles/face shield and disposable medical latex gloves and boot covers [12] (Figure 2).
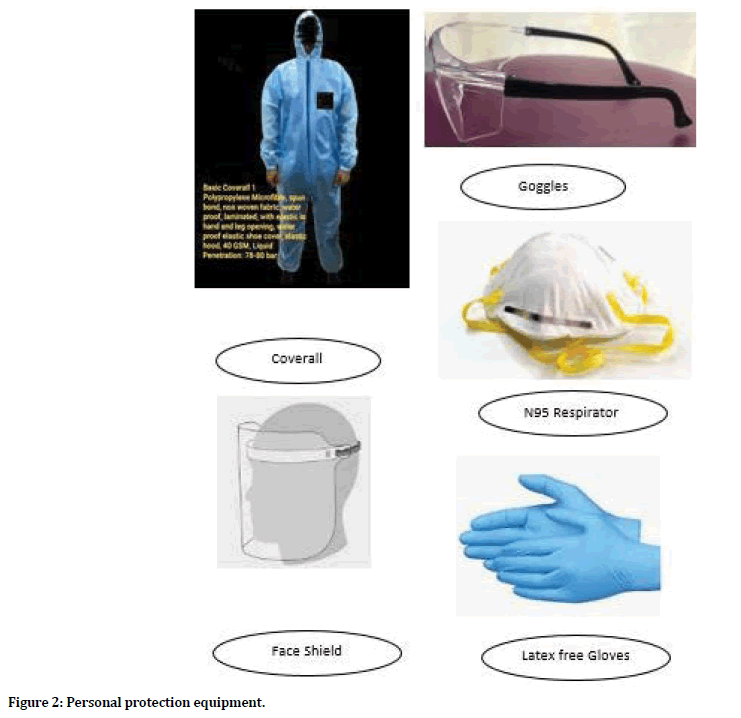
Figure 2. Personal protection equipment.
Donning and doffing of PPE should be as per standard guidelines. Hand hygiene must be performed before and after use of PPE. PPE should be disposed as per biomedical waste management guidelines under supervision of the Infection Control Team.
The following can be done in resource limited settings to optimise supplies of PPE and reuse of single use disposable PPEs.
It is preferable to shift from disposable to reusable devices (i.e., goggles and reusable face shields) during these situations. Safety glasses having side extensions to cover the eyes are preferred. Extended use of Eye protection and reprocessing of the disposable PPE can be done as per CDC recommendations. However, the PPEs should be dedicated for one healthcare provider (HCP); reprocessed as per CDC recommendations whenever visibly soiled or removed. If goggles or face shield becomes loose fitting and obscuring vision even after reprocessing, it should be discarded. The eye protection or face-shield should not be touched while in use, if touched for the purpose of adjustment, hand hygiene should be performed immediately. PPE should be removed after leaving the patient care area [28].
It is preferable to shift gown use towards cloth isolation gowns which are washable and reusable. Use of coveralls are recommended as those provide 360-degree protection for the whole body. Extended use of isolation gowns and reuse of cloth isolation gowns if required to be practised as a part of “Crisis Capacity Strategies” should be strictly in conformance to the CDC recommendations. Prioritization of gowns like surgical gowns for surgical and other sterile procedures should be practised [29].
Strategies for optimising the use of N95 respirators should be formulated by the local administration in conjunction with the Infection Control Team keeping in conformance with the CDC recommendations and taking into considerations current N95 respirator inventory and supply chain and utilisation rate. Surgical N95 respirator which is a NIOSH-approved N95 respirator that has also been cleared by the FDA as a surgical mask is recommended for use of HCPs with chances of both airborne and fluid hazards, such as splashes or sprays. NIOSH approved alternatives to N95 respirators may be used where applicable. When practicing extended use of N95 respirators, the same should be as per the CDC recommendations with the maximum recommended extended use period of 8–12 hours; restricting the use to single shift and no reused after extended use. N95 respirators should be removed and discarded appropriately before meals and restroom breaks [30].
Surveillance of anesthesia providers caring for confirmed or suspected patients
If a healthcare provider who had direct contact with confirmed or suspected patients develop fever, cough or fatigue, he/she must inform the hospital authorities. A healthcare provider meeting the criteria for medical observation should be self-isolated at home [12].
Conclusion
The chance of acquiring COVID-19 infection is higher among the anesthesiologists due to the nature of their practice. However, modifications in airway management and anesthesia practise are required to minimise aerosol generation. Regional anaesthesia should be the preferred choice wherever possible. Planned perioperative care can minimise disease transmission. Crisis capacity Strategies as per CDC recommendations to ensure smooth supply and use of Personal Protective Equipment in resource limited settings is necessary.
References
- https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
- Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382:727-733.
- Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020; 395:565-5740.
- Zhao S, Lin Q, Ran J, et al. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: A data-driven analysis in the early phase of the outbreak. Int J Infect Dis 2020; 92:214-217.
- https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200130-sitrep-10-ncov.pdf?sfvrsn=d0b2e480_2
- Christian MD, Poutanen SM, Loutfy MR, et al. Severe acute respiratory syndrome. Clin Infect Dis. 2004; 38:1420–1427.
- https://currents.plos.org/outbreaks/index.html%3Fp=40801.html
- Warriner DR. Three little words. BMJ. 2009; 338:b521–b521.
- https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- https://www.theguardian.com/world/2020/apr/10/coronavirus-world-map-countries-most-cases-and-deaths
- https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
- Chen X, Liu Y, Gong Y, et al. Chinese society of anesthesiology, Chinese association of anesthesiologists; perioperative management of patients infected with the novel coronavirus: Recommendation from the joint task force of the Chinese society of anesthesiology and the Chinese association of anesthesiologists. Anesthesiology 2020; Special Section: Covid-19: 1-10.
- https://ww.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control
- https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020; 67:568-576.
- Zhong Qi, Liu YY, Luo Q, et al. Spinal anaesthesia for patients with coronavirus disease 2019 and possible transmission rates in anaesthetists: retrospective, single-centre, observational cohort study. Br J Anaesthesia 2020; 1-6.
- Brown NW, Parsons APR, Kam PCA. Anaesthetic considerations in a parturient with varicella presenting for Caesarean section. Anaesthesia 2003; 58:1092-1095.
- https://www.wfsahq.org/components/com_virtual_library/media/1c4ec5c64b9aaacf7c47f76a61fb6edc-atow-422-01.pdf
- Wilkes AR. Heat and moisture exchangers and breathing system filters: Their use in anaesthesia and intensive care. Part 1-History, principles and efficiency. Anaesthesia. 2011; 66:31-39.
- Tan TK. How severe acute respiratory syndrome (SARS) affected the department of anaesthesia at Singapore general hospital. Anaesthesia Intensive Care 2004; 32:394-400.
- Kampf G, Todt D, Pfaender S, et al. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hospital Infection 2020; 104:246-251.
- https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2
- https://icmanaesthesiacovid-19.org/management-of-pregnant-women-with-known-or-suspected-covid-19
- Xia H, Zhao S, Wu Z, et al. Emergency caesarean delivery in a patient with confirmed coronavirus disease 2019 under spinal anaesthesia. Br J Anaesthesia 2020; e216-e218.
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/inpatient-obstetric-healthcare-guidance.html
- Tran K, Cimon K, Severn M, et al. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLOS ONE 2012; 7:e35797.
- Peng PWH, Ho PL, Hota SS. Outbreak of a new coronavirus: What anaesthetists should know. Br J Anaesthesia 2020; 124:497-501.
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/eye-protection.html
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/isolation-gowns.html
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html
Author Info
Manasij Mitra1*, Maitraye Basu2 and Sudipta Chandra3
1Department of Anesthesiology, MGM Medical College and LSK Hospital, Purab Palli, Kishanganj, Bihar, India2Department of Biochemistry, MGM Medical College and LSK Hospital, Purab Palli, Kishanganj, Bihar, India
3Department of Otorhinolaryngology and Head and Neck Surgery, Belle Vue Clinic, Dr. UN. Brahmachari Street, Kolkata, West Bengal, India
Citation: Manasij Mitra, Maitraye Basu, Sudipta Chandra, Perioperative Management of Suspected/Confirmed cases of COVID-19 in the Indian Scenario, J Res Med Dent Sci, 2020, 8(3):94-100.
Received: 13-Apr-2020 Accepted: 30-Apr-2020
