Research - (2020) Volume 8, Issue 6
Perception of Saudi Dental Surgeons Regarding Hypomineralised Second Primary Molars (HSPM)
Meer Zakirulla1*, Abdulrahman Yahya Almalki2, Maha M Alrashed1, Rashed M Alrashed1, Waleed Hussain Ali alwadei3, Asma Mohammed Alhanif4, Raghad Mohammed Alhanif1 and Sahar Nasser Fageeh1
*Correspondence: Meer Zakirulla, Department of Pediatric Dentistry and Orthodontic Sciences, College of Dentistry, Kingdom of Saudi Arabia, Tel: +966530518766, Email:
Abstract
Background: This study was to investigate the perception of dental surgeons’ knowledge of clinical condition considering its diagnosis, prevalence, severity and clinical management of Hypomineralised Second Primary Molars (HSPM). Materials & Methods: 206 male dental surgeons was participated in this cross-sectional study. Written informed consent was taken before the start of the study from the dentists. A simple random sampling method was employed in this study. Data was collected through a questionnaire. Statistical analysis was done.
Results: In this study, the majority of participants 126 (61%), were agreed that they often notice HSPM teeth in there clinical practice. Regarding the severity of the defect, 98 (48%) of white demarcations were seen by the dental surgeons. The majority of the participants agreed that 58 (28%) said that they more frequently notice this HSPM defect in the second primary molar tooth in comparison to the first permanent molar tooth. Conclusions: HSPM is a condition encountered by Saudi dentists who advocated the need for clinical training regarding HSPM-aetiological and therapeutic fields. There is considerable variation in knowledge and opinions regarding the prevalence, aetiology and the clinical management of HSPM. Continuing education on HSPM is needed to assure that the highest quality of evidence-based care is given to patients with HSPM.
Keywords
HSPM, Dentists, Enamel defect, Knowledge, MIH, Saudi Arabia.
Introduction
Hypomineralized second primary molars (HSPM) describe demarcated qualitative defects of the enamel of systematic origin affecting ≥1-second primary molars [1]. This hypomineralised disease has the same clinical presentation as compared to molar-incisor hypomineralization (MIH), and as well as structural and putative properties. The Prevalence of HSPM is between 4% and 14.5% [1-4]. HSPM is one of the risk indicators for MIH in children and causes caries risk among pediatric patients. Etiology for MIH and HSPM is mainly due to combined factors including environmental, genetic, and epigenetic factors [5]. HSPM in affected teeth are mainly due to disturbances in the process of initial maturation and calcification of enamel [6]. Mineralization of crowns for both permanent first molars and second primary molars are associated during the developmental stage of the prenatal and perinatal period. Due to this, hypomineralisation affects both second primary molars and even I the cusps of permanent second molars and canines [7]. Characteristic features of HSPM includes white to opaque brown stains, posteruptive enamel breakdown, atypical restorations, and caries with sensitivity and pain [8].
Clinical features of hypomineralization in second primary molars (HSPM) usually mistaken for hypoplasia and atypical caries due to its presentation as irregular, white, creamy, and yellow-brown opacities with post-eruptive breakdown. This defect is associated with pain, infection, and tooth loss. Treatment for this disease is very challenging due to young age involvement, anesthesia problem, and less compatibility with adhesive restorative materials. As a consequence, this HSPM leads to anxiety and dental phobia development [9]. In severe cases, similar to Molar incisor hypomineralization (MIH), hypersensitivity of teeth acts a barrier to do effective oral hygiene [10]. Those teeth are prone to increase dental caries with increased demand for extensive treatment under specialists care. This results in increase financial burden on families in the treatment of these teeth. The diagnosis and treatment of HSPM are related to its recognition by dental practitioners. Early diagnosis and referral for specialist care at the right time will help in the appropriate management of children with HSPM affected teeth. Therefore, the aim of this study is to assess the knowledge of dentists in Saudi Arabia about HSPM clinical condition considering its diagnosis, prevalence, severity, and clinical management.
Materials and Methods
A cross-sectional study was carried out on the sample size of 246 male dental surgeons in Abha, Saudi Arabia, to know the perception of Saudi Dental Surgeons regarding Hypomineralised Second Primary Molars (HSPM). Written informed consent was obtained from the participants after explaining to them the purpose of the study. The sampling method included in the study is a simple random sampling method. Ethical approval for performing the survey was obtained from the Scientific Research Committee of King Khalid University, College of Dentistry.
The questions were designed and were circulated among dental surgeons practicing in the Abha region of Saudi Arabia. The questionnaire was formulated, which comprised of two parts: The first portion included the questions related to the demographic information of participants, such as age, gender, year of experience, and level of education. The other part of the questionnaire comprised of 12 questions with ‘yes’ and ‘no’ pattern, and the multiple-choice question was prepared, and piloting was done.
A self-administered structured questionnaire originated and tested among a comfort sample of 20 dental surgeons. These were interviewed to get feedback on the entire acceptability of the study when it comes to length and language clearness; in accordance with their feedback, the queries were corrected. Encounter validity was furthermore assessed before the start of research. Both descriptive and analytical statistical dimensions were used to describe the primary variables by SPSS 18 (IBM Corporation, Armonk, NY, USA) software.
Results
A total of 206 dentists responded to the questionnaire. 53% of study subjects were of < 30 years, 38% were of 31-40 years, 6% were of 41-50 years, and 3% were >50 years (Table. 1). 154 (75%) and 52 (25%) were Males and females of the total study samples. Distribution of study samples according to a year of experience and level of education were shown in Table 1. The perception of HSPM among Saudi dental surgeons was shown in Table 2.
| Age | n (206) | % |
|---|---|---|
| <30 years | 109 | 53 |
| 31-40 years | 78 | 38 |
| 41-50 years | 12 | 6 |
| >50 years | 7 | 3 |
| Gender | ||
| Male | 154 | 75 |
| Female | 52 | 25 |
| Year of experience | ||
| < 5 years | 98 | 48 |
| 6-10 Years | 72 | 35 |
| >10 years | 36 | 17 |
| Level of Education | ||
| Bachelor | 174 | 84 |
| Master | 32 | 16 |
| n=Number; %=Percentage | ||
Table 1: Distribution of study sample according to age, gender, year of experience, and level of education.
| Questionnaire | n (206) | % |
| Do you encounter hypomineralizations in second primary molars (HSPM) teeth in your practice? | ||
| Yes | 124 | 60 |
| No | 82 | 40 |
| How often do you notice HSPM teeth in your practice? | ||
| Daily | 27 | 13 |
| Weekly | 126 | 61 |
| Monthly | 20 | 10 |
| Yearly | 33 | 16 |
| Regarding severity of the defect; which of the following do you most frequently notice in your practice? | ||
| White demarcation | 98 | 48 |
| Yellow/brown demarcation | 63 | 31 |
| Post eruptive breakdown | 45 | 21 |
| How frequently do you notice this hypomineralization defect in the second primary molar tooth in comparison to the first permanent molar tooth? | ||
| More frequently | 58 | 28 |
| Less frequently | 128 | 62 |
| Same as first permanent molar | 20 | 10 |
| Are you aware that HSPM is a developmental defect of enamel that differs from dental fluorosis and hypoplasia? | ||
| Yes | 154 | 75 |
| No | 52 | 25 |
| Do you think it would be worthwhile to investigate the prevalence of HSPM in your community? | ||
| Yes | 132 | 64 |
| No | 74 | 36 |
| Do you know if there are clinical criteria to diagnose HSPM? | ||
| Yes | 91 | 44 |
| No | 115 | 56 |
| Do you feel the incidence has increased in the period of your practice? | ||
| Yes | 170 | 83 |
| No | 36 | 17 |
| How do you feel about diagnosing HSPM? | ||
| Confident | 106 | 51 |
| Unconfident | 85 | 41 |
| Very unconfident | 15 | 8 |
| How do you feel about treating HSPM? | ||
| Confident | 142 | 70 |
| Unconfident | 29 | 14 |
| Very unconfident | 35 | 16 |
| n=Number; %=Percentage | ||
Table 2: Perception of HSPM by Saudi Arabian dental surgeons.
The majority of participants, 126 (61%) were agreed that they often notice HSPM teeth in there clinical practice. Regarding the severity of the defect, 98 (48%) of white demarcations were seen by the dental surgeons. The majority of the participants agreed that 58 (28%) said that they more frequently notice this HSPM defect in the second primary molar tooth in comparison to the first permanent molar tooth. 132 (64%) participants believed that its worthwhile to investigate the prevalence of HSPM in there community. 115(56%) agreed that they do not know the clinical criteria to diagnose HSPM. According to 170 (83%) of participants felt that the incidence of HSPM is increased in their clinical practice. The majority of the participants agreed that the causative etiology of HSPM was genetics (32%), next was environmental contaminants (19%) (Figure 1). Various materials used to treat HSPM tooth and their concern regarding treatment options by dental surgeons given in Figure 2.
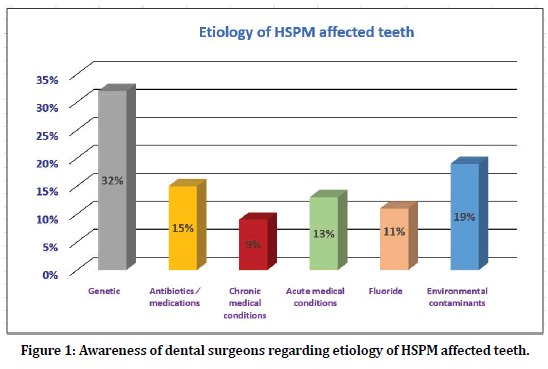
Figure 1. Awareness of dental surgeons regarding etiology of HSPM affected teeth.
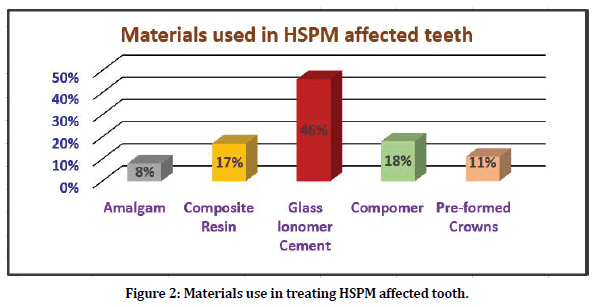
Figure 2. Materials use in treating HSPM affected tooth.
Discussion
The epidemiology of dental care caries and periodontal diseases has been widely studied in Saudi Arabia. Nevertheless, the literature on MIH and HSPM will be sparse, though it is acknowledged as a distinct medical entity in Saudi Arabia. That is probably the first research investigating the perception of Saudi dentists concerning this condition. There might have been variations in criteria for the study of these teeth. This emphasizes the necessity to perform a study of this situation with calibrated examiners. Furthermore, because of varied presentations dependant on the degree of involvement, age group of the patient during diagnosis, and amount of damage, it becomes quite difficult to categorize HSPM. The prevalence of HSPM varies between various countries, which range from 2.9% to 21.8% [1-3]. In the principal dentition, molars will be the teeth most frequently suffering from caries, and 2nd molars are more usually affected than 1st molars. A confident correlation between enamel hypoplasia and caries in the principal dentition was within some investigations [11]. Because of the early lack of second main molars with a number of factors like post-eruptive breakdown caused by long time publicity in the mouth and earlier extractions, it outcomes in under-scoring of the prevalence of the lesion [11].
The most typical clinical manifestation encountered by the participants inside our study was white demarcated defects (48%), another lesion was yellow/brown demarcation (31%). A correlation between hardness ideals, mineral density, and the color of the hypomineralized enamel offers been proven, with yellow/ brownish opacities becoming softer than whitened [12]. This results in earlier breakdown and associated signs and symptoms, evoking the affected patients to get treatment. Yellow/dark brown opacities are often distinguishable from fluorosis and whitened spot lesions because of caries in comparison with other scientific manifestations of HSPM, resulting in earlier differentiation. The HSPM situation is a risk element for molar-incisor hypomineralization (MIH), sharing an identical clinical presentation, structural qualities, and putative etiology [6]. Dentists' responses reflect the hypothesis that the etiology may be multifactorial, with a diversity of responses. In our study, 32% of dentists attributed the etiology to genetic factors, and the second cause was 19% for environmental contaminants. Although the etiology of MIH and HSPM is currently unknown, a combination of environmental factors from the prenatal and early life period and genetic and epigenetic factors is thought to contribute [13]. Observational studies have linked HSPM with a range of early-life environmental factors, including maternal alcohol intake during pregnancy, low birth weight, and early childhood illness [6, 14]. Early childhood illness was reported to have the strongest association with MIH [15].
In the current study, 46% of dentist choice for restoration for HSPM teeth was Glass-ionomer cement, and next was composite restorative materials. This may be because they treat younger children and use it as filling material in atraumatic restorative treatments or for interim restorations. There are studies using GIC (81%) more than RMGIC (44.3%), which is justified by the greater fluoride release [16]. Inside our study, over fifty percent of the dental surgeons (51%) agreed they are confident in diagnosing HSPM in children. Kids with HSPM have a severe danger for caries and bad oral hygiene [17]. Early recognition of HSPM will initiate preventive steps for preventing caries and bad oral hygiene. If this precautionary gauge isn't employes, that may bring about social, financial distress caused by pain, mental, and multiple dental care clinic visits [18]. Early recognition of HSPM in kids provides preventive therapy for post-eruptive breakdown with advantageous public teeth's health actions for the analysis population.
Conclusion
HSPM is a condition encountered by Saudi dentists who advocated the need for clinical training regarding HSPM-aetiological and therapeutic fields. There is considerable variation in knowledge and opinions regarding the prevalence, aetiology and the clinical management of HSPM. Continuing education on HSPM is needed to assure that the highest quality of evidence-based care is given to patients with HSPM.
Hypomineralised second primary Molars (HSPM) will be an acknowledged dental care issue by oral surgeons inside Saudi Arabia. White-colored demarcated opacities had been the almost all documented medical demonstration, and the glass ionomer cement has been the nearly all favored dental care materials for repairing HSPM tooth. Many dentists and oral professionals would make use of preformed metallic crowns for severely affected molars. Dentist documented acceptable amounts of self-confidence in HSPM analysis, which necessitates performing continuing dental education programs to offer high-quality dental care treatment for kids with HSPM and to expose in-depth information on HSPM, its etiology, and its therapy into the oral program at the undergraduate degree.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Elfrink ME, Schuller AA, Weerheijm KL, et al. Hypomineralized second primary molars: Prevalence data in Dutch 5-year-olds. Caries Res 2008; 42:282–285.
- Mittal N, Sharma B. Hypomineralised second primary molars: prevalence, defect characteristics and possible association with molar incisor hypomineralisation in Indian children. Eur Arch Paediatr Dent 2015; 16:441–447.
- Temilola OD, Folayan MO, Oyedele T. The prevalence and pattern of deciduous molar hypomineralization and molar-incisor hypomineralization in children from a suburban population in Nigeria. BMC Oral Health 2015; 15:73.
- Owen M, Ghanim A, Elsby D, et al. Hypomineralised second primary molars: prevalence, defect characteristics and relationship with dental caries in Melbourne preschool children. Aust Dent J 2018; 63:72–80.
- Teixeira RJPB, Andrade NS, Queiroz LCC, et al. Exploring the association between genetic and environmental factors and molar incisor hypomineralization: Evidence from a twin study. Int J Paediatr Dent 2018; 28:198–206.
- Elfrink ME, cate JM, Jaddoe VWV, et al. Deciduous molar hypomineralization and molar incisor hypomineralization. J Dent Res 2012; 91:551-555.
- Schmalfuss A, Stenhagen KR, Tveit AB, et al. Canines are affected in 16-year-olds with molar-incisor hypomineralisation (MIH): An epidemiological study based on the Tromsø study: Fit Futures. Eur Arch Paediatr Dent 2016; 17:107-113.
- Weerheijm KL, Jälevik B, Alaluusua S. Molar-incisor hypomineralisation. Caries Res 2001; 35:390–391.
- Jalevik B, Klinberg GA. Dental treatment, dental fear and behavioural management problems in children with severe hypomineralisation of their first permanent molars. Int J Paediatr Dent 2002; 12:24-32.
- Zakirulla M, Essa A Khormi, Hamed M Bakri, et al. Prevalence of Molar Incisor Hypomineralisation (MIH) in 7-10-year-old school children in southern Saudi Arabia: A cross-sectional study. Annals Tropical Medicine Public Health 2018; 2:192-207.
- Negre-Barber A, Montiel JM, Catala MB, et al. Hypomineralized second primary molars as predictor of molar incisor hypomineralization. Sci Rep 2016; 6:31929.
- Suckling GW, Nelson DG, Patel MJ. Macroscopic and scanning electron microscopic appearance and hardness values of developmental defects in human permanent tooth enamel. Adv Dent Res 1989; 3:219-233.
- Teixeira RJPB, Andrade NS, Queiroz LCC, et al. Exploring the association between genetic and environmental factors and molar incisor hypomineralization: Evidence from a twin study. Int J Paediatr Dent 2018; 28:198–206.
- Ghanim AM, Morgan MV, Marino RJ, et al. Risk factors of hypomineralised second primary molars in a group of Iraqi school children. Eur Arch Paediatr Dent 2012; 13:111–118.
- Silva MJ, Scurrah KJ, Craig JM, et al. Etiology of molar incisor hypomineralization-A systematic review. Community Dent Oral Epidemiol 2016; 44:342–353.
- Crombie FA, Manton DJ, Weerheijm KL, et al. Molar incisor hypomineralization: A survey of members of the Australian and New Zealand society of paediatric dentistry. Aust Dent J 2008; 53:160–166.
- Oyedele TA, Folayan MO, Oziegbe EO. Hypomineralised second primary molars: Prevalence, pattern and associated co morbidities in 8- to 10-year-old children in Ile-Ife, Nigeria. BMC Oral Health 2016; 16:65.
- Moure-Leite FR, Ramos-Jorge J, Ramos-Jorge ML, et al. Impact of dental pain on daily living of five-year-old Brazilian preschool children: Prevalence and associated factors. Eur Arch Paediatr Dent 2011; 12:293–297.
Author Info
Meer Zakirulla1*, Abdulrahman Yahya Almalki2, Maha M Alrashed1, Rashed M Alrashed1, Waleed Hussain Ali alwadei3, Asma Mohammed Alhanif4, Raghad Mohammed Alhanif1 and Sahar Nasser Fageeh1
1Department of Pediatric Dentistry and Orthodontic Sciences, College of Dentistry, Abha, Kingdom of Saudi Arabia2Department of Preventive Dental Sciences, Division of Pediatric Dentistry, Teaching Assistant at College of Dentistry, Jazan University, Jazan, Kingdom of Saudi Arabia
3General Dentist, Ministry of Health, Abha, Kingdom of Saudi Arabia
4General Dentist, Private clinic, Abha, Kingdom of Saudi Arabia
Citation: Meer Zakirulla, Abdulrahman Yahya Almalki, Maha M Alrashed, Rashed M Alrashed, Waleed Hussain Ali alwadei, Asma Mohammed Alhanif, Raghad Mohammed Alhanif, Sahar Nasser Fageeh, Perception of Saudi Dental Surgeons regarding Hypomineralised Second Primary Molars (HSPM), J Res Med Dent Sci, 2020, 8 (6): 71-76.
Received: 28-Jul-2020 Accepted: 11-Sep-2020
