Research - (2021) Volume 9, Issue 3
Patient Satisfaction and Preference with Dry Shield vs. Rubber Dam Isolation among Pediatric Patients
Sara M Bagher*, Hanaa K Allaf, Layla N Khogeer and Osama Felemban
*Correspondence: Sara M Bagher, Department of Pediatric Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia, Email:
Abstract
Aims: was to conduct a comparative evaluation of the DryShield isolation system (DSI) to the rubber dam isolation (RDI) during premolar fissure sealants (FS) placement as for the chair time, subjective patient discomfort, pain and future preference among 9 to 15-year-old pediatric dental patients. Material and Methods: This split-mouth randomized clinical study included healthy 9 to 15-year-old children with at least one pair of contralateral fully erupted, caries-free permanent premolars indicated for FS. Teeth were randomly allocated to either the control or the test group. In the control group, teeth received FS with RDI while the test group teeth received FS with DSI. Chair time was recorded using a stopwatch. Subjects rated their pain using a answered a validated Arabic interview questionnaire after completing both procedures. Results: Twenty-eight subjects were included. The DSI significantly reduced the chair time with a P-value of <0.001. Subjects reported that they were significantly more annoyed by the noise associated with DSI (2.07 ± 2.11) with P-value of 0.022. Older subjects were less likely to report higher pain scores pain score (OR=0.59, 95% CI, 0.42 – 0.84, P=0.003) compared to younger subjects regardless of gender and the type of isolation system used. No significant differences were found in future preference of DSI or RDI (P=1.00). Discussion and Conclusion: The use of DryShield isolation during fissure sealant application on premolars is associated with a significant reduction in chair time compared to the rubber dam isolation and can be used as an alternative to the rubber dam isolation among pediatric patients.
Keywords
DryShieled, Fissure sealants, Isolation, Rubber dam
Introduction
The most widely used method when performing isolation during dental treatment is rubber dam isolation (RDI), which consists of a rubber sheet, a metal clamp, and a metal frame, all of which provide excellent isolation, retraction, and operator visibility [1]. Although the RDI is an effective isolation tool, it has many drawbacks such as concerns over patient acceptance, the time required for application, cost of equipment and materials, and insufficient training [2].
The DryShield isolation (DSI) system is a newly proposed alternative to RDI. This new system was developed in the United States and is similar to the isolite system isolation (ISI), but it differs in that it does not provide illumination and can be autoclaved [3].The system consists of a bite block and cheek and tongue retractors that connect to the high-volume suction. Therefore, DSI provides the dual function of retraction and suction. In addition, the bite block assists in opening the mouth and stabilizing it. Another advantage of the system is its ability to retract and isolate one side of the oral cavity at the same time, which gives the dentist access to both upper and lower quadrants simultaneously [3].
Fissure sealants (FS) are a preventive, conservative approach. Their use involves the application of sealants into the pits and fissures of teeth, thus changing the teeth’s morphology to a more favorable one that facilitates oral hygiene and prevents debris retention in occlusal pits and fissures [4]. Proper isolation is an essential step in the FS procedure [5], failure to properly isolate the teeth has a negative impact on the treatment outcome and places the patient at risk of swallowing or aspirating materials and instruments [1].
Pediatric patients’ satisfaction, preference and the time required for FS application was compared between ISI and cotton roll isolation (CRI) by Collette et al., 2009 [6] and between ISI and RDI by Alhareky et al., 2013 [3]. Both reported that ISI required significantly less time and was associated with more noise and discomfort when compared to CRI and RDI. Also, more children preferred ISI for their future dental treatment [3,6]. It was also reported that the retention rate of FSs place with ISI is similar to the FSs placed under CRI [7].
Our aim in this study was to conduct a comparative evaluation of the DryShield isolation system to the rubber dam isolation during premolar fissure sealants placement as for the chair time, subjective patient discomfort, pain and future preference among 9 to 15-yearold pediatric dental patients.
Materials and Methods
This split-mouth prospective controlled randomized clinical trial was conducted at Kig Abdulaziz University (KAAU) in the Pediatric Dentistry Department between January and March 2020. The study protocol was approved by the Research Ethics Committee in Kig Abdulaziz University (123-9-19).
The inclusion criteria were: 1) healthy 9 to 15 years old cooperative children requiring nonurgent dental treatment and 2) children with at least two contralateral fully erupted, cariesfree permanent premolars with normal enamel. Children with partially erupted or previously restored premolars were excluded.
Sample size and sampling technique
The software nQuery version 8.0 was used to calculate the sample size. Based on the results of Alhareky et al., 2014 [3], it was found that a two-group chi-square test with a 5% two-sided significance level will have 80% power to detect a difference between group 1 proportion of 0.31 and group 2 proportion of 0.69 (odds ratio of 4.95) when the sample size is 26 patients with paired contralateral sound premolars in need of FS.
Patients receiving dental treatment in the Pediatric Dentistry Department’s clinics during the study period were screened for inclusion in the study and the parents/guardians of eligible subjects were approached. The researsh aim was explained to those who agreed to participate and an Arabic consent form was signed by the parents/guardians before their children’s participation.
A randomization sequence was generated using a computer-generated program (https://www. randomizer.org/) and was performed before the treatment appointment to randomly assign each tooth in the pair to one of the isolation systems. Another randomization scheme was generated to decide which isolation system (DSI or RDI) would be used first. Subjects who were assigned to have DSI followed by RDI were categorized in Group 1. Subjects who received the isolation in the reverse order were categorized in Group 2. Only one randomly selected pair of eligible premolars was included in each subject. Both treatments were provided at the same visit, and all the FSs were performed by the same dentist with an assistant’s help.
Treatment
All subjects received fissure sealants using RDI and DSI according to the randomization sequence. Neither topical nor local anesthesia was applied prior to the rubber dam (RD) clamp application. The RD clamp was applied on the included premolar and the isolation included 2-3 teeth anterior to it. No bite block was used with the RDI and all subjects in the test group received a Pedo size mouthpiece. In addition, Tell-Show-Do behaviour management technique was used for all subjects during FS application with both RDI and DSI.
After isolation, FS (Conseal-F TM SDI) was applied following the manufacture instructions. The quality of the FS was checked using an explorer and, if there was any deficiency, a top on layer was added to the deficient site or sites. A stopwatch was used to measure the chair time. The time required to assemble the DSI in the test group and to select the appropriate RD clamp in the control group were not included.
Immediately, after the completion of each procedure, the subjects were asked to rate their pain using a Validated Arabic Version of Wong- Baker FACES Pain Rating Scale. They were asked to pick one of the scale’s faces that described how they felt during the procedure.
At the end of the appointment and after completing both procedures, the subjects were asked to answer a validated Arabic interview questionnaire to evaluate their subjective discomfort and future preference regarding the two isolation systems.
The study questionnaire
The questionnaire was developed in the Arabic language based on a combined review of several previously developed English questionnaires [3,6,8].
The interview questionnaire consisted of several questions assessing the patients’ subjective discomfort and future preference between DSI and RDI during dental treatments. The first part included data regarding age, gender, and each patient’s previous experience with dental isolation.
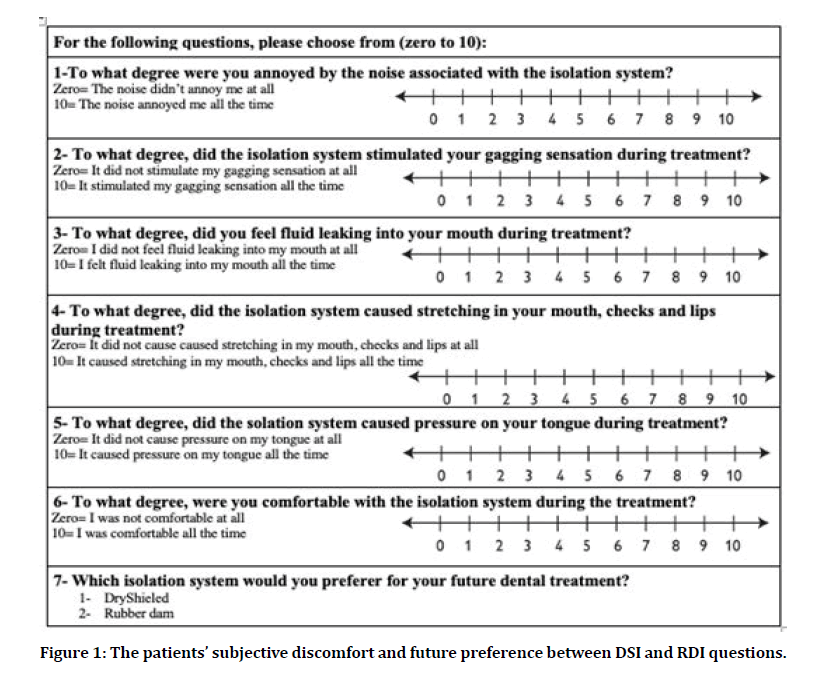
The second part consisted of seven questions on a numerical scale from zero to 10 for the subjects to rate their experiences in relation to noise, gagging sensation, fluid leaking, stretching, pressure, and discomfort associated with the isolation systems. Zero on the numerical scale represented the complete absence of the irritating factors, while 10 represented the presence of the irritating factors at all times during the procedure. Finally, the subjects were asked about their future preference of an isolation system. This section was answered after the completion of both procedures at the end of the dental visit. The patients’ subjective discomfort and future preference between DSI and RDI questions are represented in Figure 1.
Figure 1: The patients’ subjective discomfort and future preference between DSI and RDI questions.
Assessment of the study questionnaire
To establish the face validity, 20 children from the same age group who were receiving dental treatments at a pediatric dentist at KAAU were invited to read the questions, offer their opinions, and report whether they had any trouble understanding or answering any of the questions. Based on their feedback, a few changes were made.
Later, two expert pediatric consultants at KAAU each assessed the questions. Based on their feedback, the question inquiring about the noise level was revised. Also, the question about the gagging sensation was changed to a positive phrasing instead of a negative phrasing. Furthermore, a note was added to the part of the demographic data that had to be answered by the parents. Finally, multiple grammatical mistakes were corrected.
After addressing all of these changes based on face validity and the experts’ opinions, four pediatric consultants at KAAu individually assessed each question based on its clarity, simplicity, ambiguity, and the relevance to the aim of the study on a four-point scale ranging from 1 to 4 (1 = very important, 2 = important, 3 = moderately important, and 4 = not important). The validity of the questionnaire was evaluated by calculating the Item-Content Validity Index (I-CVI) and the Scale-Content Validity Index (S-CVI). The results showed excellent content validity (I-CVI = 0.89 and S-CVI = 0.96).
Statistical analysis
Demographic variables were summarized as means and standard deviation (SD) or frequencies and compared between the groups by sequence of intervention using Mann Whitney U test, chi-square test, or Fisher exact test. Bivariate analysis was carried out to test the differences between the two isolation systems in terms of time, pain, behavior, subjective discomfort, and future preference. To account for the pairings in the data, the Wilcoxon Signed Rank Test were used for the bivariate analysis. To evaluate if the sequence of the isolation system had an effect on the outcomes, the subjects’ responses of the DSI were subtracted from the RDI and the mean difference in each group was compared using Mann Whiney U test. To estimate the effects of age, gender, and the type of the isolation system on the study’s outcomes, Generalized Estimating Equations were used to account for the clustering in the data (two teeth per subject). All statistical analyses were done using IBM SPSS Statistics for Windows, version 23 (IBM Corp., Amonk, N.Y., USA).
Results
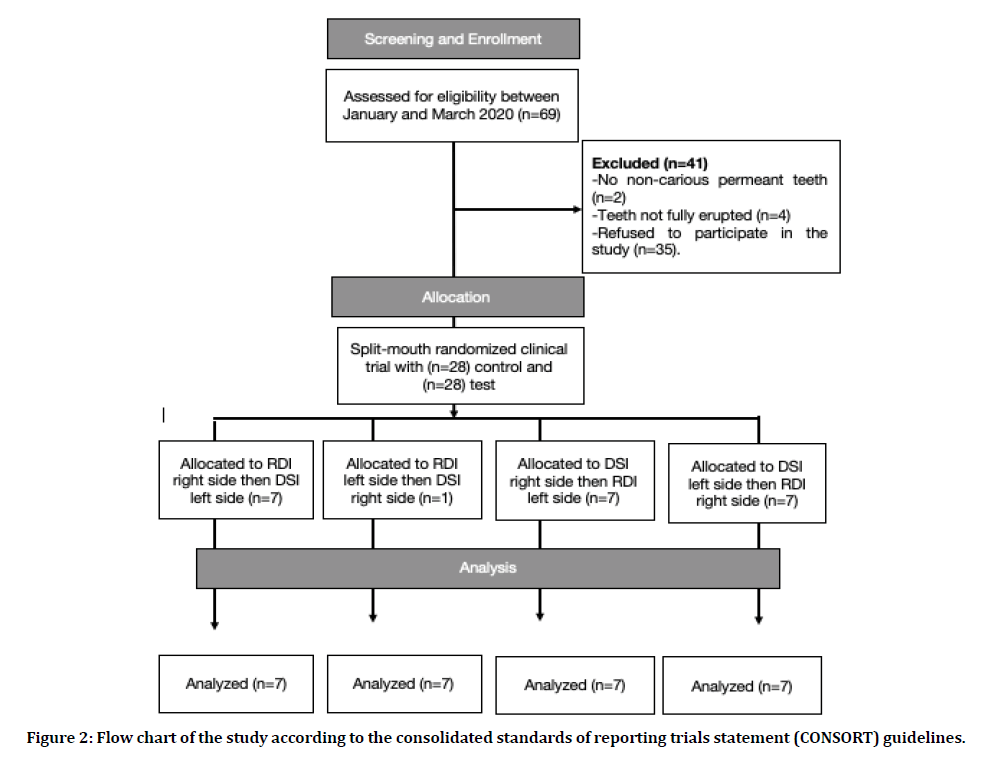
Of the 34 subjects who were screened for inclusion in the study, 28 were found to be eligible and agreed to participate. The Flow Chart of the study according to the Consolidated Standards of Reporting Trials Statement (CONSORT) guidelines in presented in Figure 2 [9]. Table 1 summarizes the demographic characteristics of the subjects stratified by the isolation sequence. The mean ± SD age of the subjects was 11.54 ± 1.64 year and more than half (57.1%) of them were males. About half of the subjects (53.6%) had a previous experience with RDI and 10.7% of them had partial isolation with cotton rolls before. About fifth of the subjects (21.4%) did not have previous experience of any isolation system. The majority (82.1%) of the treated teeth were in the lower arch. A comparison of the baseline characteristics showed no significant differences between Group 1 (DSI followed by RDI) and Group 2 (RDI followed by DSI).
Figure 2: Flow chart of the study according to the consolidated standards of reporting trials statement (CONSORT) guidelines.
Table 1: Demographic characteristics of the subjects stratified by the isolation sequence.
| Variables | All subjects n=28 | Group 1 (DSI followed by RDI) | Group 2 (RDI followed by DSI) | P-value |
|---|---|---|---|---|
| n=14 | n=14 | |||
| Age | 11.54 ± 1.64 | 11.50 ± 1.56 | 11.57 ± 1.79 | 0.946† |
| Gender | N (%) | N (%) | N (%) | 0.445‡ |
| Male | 16 (57.1) | 7 (50.0) | 9 (64.3) | |
| Female | 12 (42.9) | 7 (50.0) | 5 (35.7) | |
| Previous Experience | ||||
| Yes, RDI | 15 (53.6) | 8 (57.1) | 7 (50.0) | 0.728‡ |
| Yes, CRI | 3 (10.7) | 2 (14.3) | 1 (7.1) | |
| Yes, RDI and CRI | 3 (10.7) | 1 (7.1) | 2 (14.3) | |
| I do not remember | 1 (3.6) | 1 (7.1) | 0 (0.00) | |
| No | 6 (21.4) | 2 (14.3) | 4 (28.6) | |
| Upper Arch | 5 (17.9) | 3 (21.4) | 2 (14.3) | 1.00‡ |
| Lower Arch | 23 (82.1) | 11 (78.6) | 12 (85.7) | |
†Mann-Whitney U test
‡ Chi-square test or Fisher exact test
DSI: DryShieled isolation
RDI: Rubber dam isolation
CRI: Cotton roll isolation
Table 2 illustrates the differences in time, pain, and subjective discomfort between the isolation systems. The use of DSI significantly reduced the chair time required to finish the dental procedure compared to the RDI with a P-value of <0.001. The mean ± SD chair time required to finish the procedure using the DSI was 3.59 ± 0.72 minutes, while the chair time required using the RDI was 4.20 ± 0.72 minutes. The mean ± SD chair time required by the DSI was 0.91 ± 0.92 minutes less than the time for the RDI. Regarding the Wong Baker Faces Pain Rating Scale, the subjects reported slightly less pain and discomfort when using the DSI (1.21 ± 1.57) compared to RDI (1.71 ± 2.23), but the difference was not statistically significant with P-value of 0.336. Subjects reported that the mean ± SD score of to which extent they were annoyed by the noise associated with the isolation system was significantly higher with DSI (2.07 ± 2.11) than the RDI (0.86 ± 1.60) with P-value of 0.022. The mean scores reported by the subjects also showed that DSI slightly increased their gagging sensation but decreased their feeling of fluid leakage into their mouth, caused slightly more stretching on their lips and cheeks, and more pressure on their tongue, and was less comfortable in comparison to RDI.
Table 2: Comparison of pain and subjective discomfort between the DryShield and the rubber dam isolation system.
| DSI | RDI | P-value | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Time | 3.59 ± 0.72 | 4.50 ± 0.72 | <0.001* |
| Wong Baker Faces Pain Rating Scale | 1.21 ± 1.57 | 1.71 ± 2.23 | 0.336 |
| On a scale from 0 to 10: where 0 is the least and 10 is the most, to what degree did you feel: | |||
| Annoyed by the noise associated with the isolation system | 2.07 ± 2.11 | 0.86 ± 1.60 | 0.022* |
| Wanted to throw up because of the isolation system | 1.04 ± 2.52 | 0.43 ± 1.60 | 0.206 |
| Isolation system stretching lips and cheeks | 3.68 ± 3.19 | 3.50 ± 3.90 | 0.627 |
| Isolation system causing pressure on the tongue | 3.29 ± 3.54 | 2.57 ± 3.36 | 0.494 |
| Water leaking into mouth while using the isolation system | 0.93 ± 1.72 | 1.32 ± 2.40 | 0.341 |
| Isolation system being uncomfortable | 2.86 ± 3.08 | 2.54 ± 3.04 | 0.683 |
* Statistically significant at P=0.05 level using Wilcoxin Signed Rank test.
DSI: DryShieled isolation
RDI: Rubber dam isolation
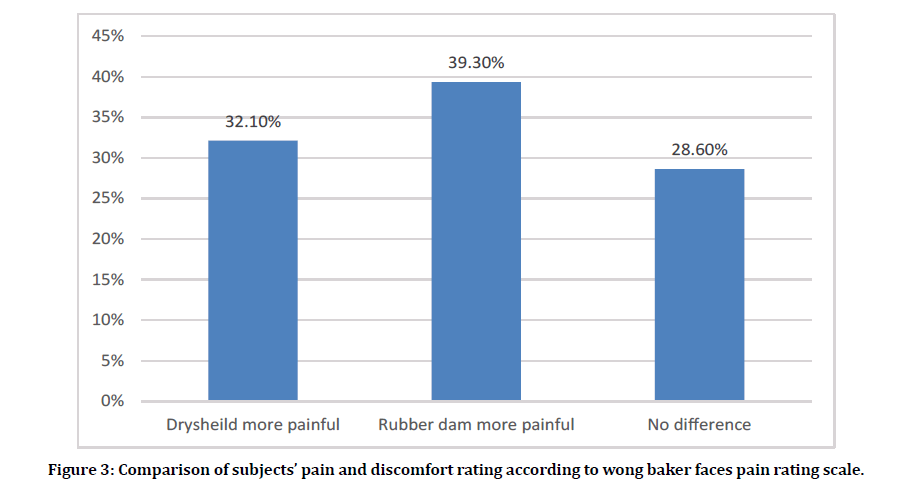
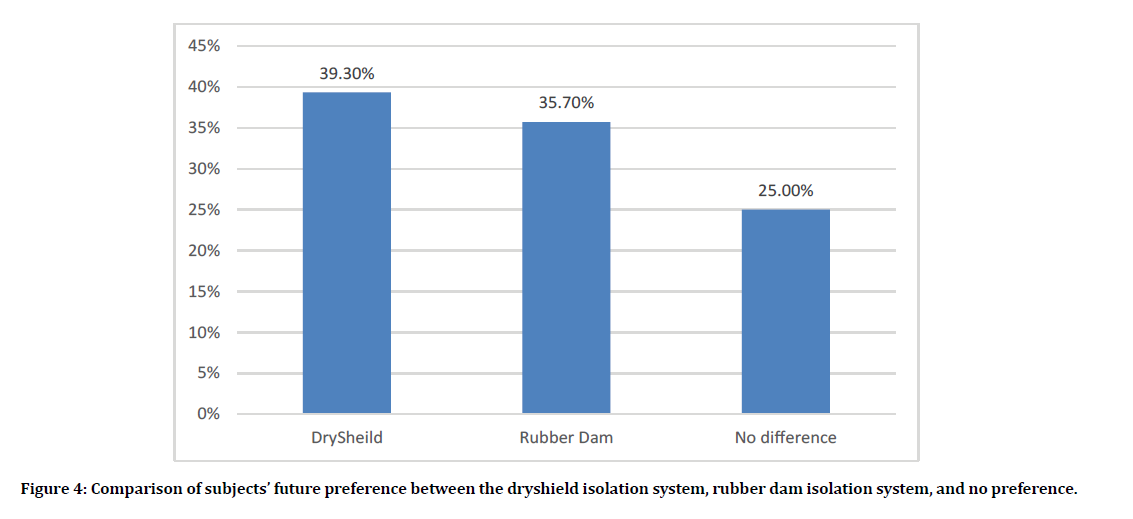
According the Wong Baker Faces Pain Rating scale scores, eleven (39.3%) subjects rated RDI as more painful than DSI as opposed to 9 (32.1%) subjects who rated DSI was more painful than RD. The remaining 8 (28.6%) subjects reported no difference in Wong Baker Faces Pain Rating Scale between DSI and RDI (Figure 3). When asked which of the two isolation systems do you prefer in the future, 11 subjects (39.3%) preferred DSI, 10 subjects (25.7%) preferred the RDI, and 7 subjects (25.0%) were indifferent (P=1.00). Subjects’ future preference of the isolation systems is demonstrated in Figure 4. The effect of the isolation sequence on the study outcomes were explored and the results are shown in Table 3. Neither pain, time, nor subjective discomfort were significantly affected by the isolation sequence.
Figure 3: Comparison of subjects’ pain and discomfort rating according to wong baker faces pain rating scale.
Figure 4: Comparison of subjects’ future preference between the dryshield isolation system, rubber dam isolation system, and no preference.
Table 3: Comparison of the mean differences of DryShieled isolation system and Rubber dam isolation between the groups.
| Variables | Group 1 (DSI followed by RDI) | Group 2 (RDI followed by DSI) | P-value† |
|---|---|---|---|
| Mean difference ± SD (RDI – DSI) | |||
| Time | 0.64 ± 0.96 | 1.18 ± 0.81 | 0.164 |
| Wong Baker Faces Pain Rating Scale | 0.43 ± 2.95 | 0.57 ± 1.83 | 0.541 |
| On a scale from 0 to 10: where 0 is the least and 10 is the most, to what degree did you feel: | |||
| Annoyed by the noise associated with the isolation system | -1.07 ± 2.84 | -1.36 ± 2.50 | 0.769 |
| Wanted to throw up because of the isolation system | -0.43 ± 3.06 | -0.79 ± 2.67 | 1.00 |
| Isolation system stretching lips and cheeks | -0.50 ± 2.90 | 0.08 ± 3.99 | 1 |
| Isolation system causing pressure on the tongue | -0.64 ± 4.50 | -0.79 ± 4.34 | 0.839 |
| Water leaking into mouth while using the isolation system | 0.21 ± 1.63 | 0.57 ± 2.41 | 0.734 |
| Isolation system being uncomfortable | -1.71 ± 4.68 | 1.07 ± 3.27 | 0.246 |
†Mann-Whitney U test
Table 4: Results of the Generalized Estimating Equations (GEE) model to estimate the effects of the Isolation system on time, pain, and subjective discomfort while controlling for age and gender.
| Variables | Age b (95% CI) | Gender (male vs females) b (95% CI) | Group (DSI vs RDI) b (95% CI) |
|---|---|---|---|
| P-value | P-value | P-value | |
| Time | -0.05 (-0.15 – 0.06) | 0.14 (-0.26 – 0.54) | -0.91 (-1.24--0.58) |
| P=0.393 | P=0.481 | P<0.001* | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| P-value | P-value | P-value | |
| Wong Baker Faces Pain Rating Scale | 0.59 (0.42 – 0.84) | 1.34 (0.46–3.92) | 0.69 (0.26–1.87) |
| P=0.003* | P=0.590 | P=0.467 | |
| Annoyed by the noise associated with the isolation system | 1.23 (0.85 – 1.78) | 0.98 (0.38–2.52) | 4.04 (1.45–11.23) |
| P=0.267 | P=0.971 | P=0.007* | |
| Wanted to throw up because of the isolation system | 0.99 (0.61 – 1.59) | 1.47 (0.22–9.61) | 3.45 (0.71–16.89) |
| P=0.950 | P=0.689 | P=0.126 | |
| Isolation system stretching lips and cheeks | 0.74 (0.50 – 1.09) | 0.94 (0.31–2.86) | 1.18 (0.60–2.32) |
| P=0.130 | P=0.907 | P=0.624 | |
| Isolation system causing pressure on the tongue | 0.76 (0.51 – 1.12) | 1.07 (0.37–3.11) | 1.43 (0.62–3.30) |
| P=0.166 | P=0.902 | P=0.403 | |
| Water leaking into mouth while using the isolation system | 0.94 (0.58 – 1.53) | 0.46 (0.11–1.97) | 0.84 (0.37–1.94) |
| P=0.791 | P=0.296 | P=0.684 | |
| Isolation system being uncomfortable | 0.98 (0.70 – 1.37) | 1.01 (0.39–2.5) | 1.30 (0.55–3.11) |
| P=0.883 | P=0.987 | P=0.553 |
* Statistically significant at P=0.05 level.
Table 4 illustrates the effects of the isolation system used on the time, subjective discomfort, and pain accounting for the clustering in the data while controlling for age and gender. The procedure done with the DSI system required significantly less time (β= -0.91, 95% CI, -1.24 - -0.58, P<0.001) compared to the procedures performed using RDI controlling for age and gender. Older subjects were less likely to report higher pain scores pain score (OR=0.59, 95% CI, 0.42 – 0.84, P=0.003) compared to younger subjects regardless of gender and the type of isolation system used. Also, the subjects were 4.04 times more annoyed by the sound associated with the DSI when compared to the RDI (95% CI, 1.45 – 11.23, P=0.007) controlling for age and gender.
Discussion
The DSI is a newly developed system that is similar to the ISI. The main differences are that the DSI is auto clavable and does not provide illumination [3]. To our knowledge, there are only two published studies aimed at assesses patients’ satisfaction and future preference for the ISI when compared to the CRI [6] and the RDI [6]..However, no published study has aimed at assessing patients’ satisfaction and preference with the DSI.
Our study showed three clinically significant outcomes. First, the chair time required to perform FS on a permanent premolar was significantly less with the DSI in comparison to the RDI by an average of 0.91 minute. Second, children were significantly more annoyed by the noise associated with the DSI. Finally, older children complained more about the pressure on their tongue and reported higher pain scores compared to younger children regardless of the type of isolation system used.
In our study, the DSI reduced the chair time needed for FS application when compared to RDI, which agrees with previously published studies [3,6]. in which ISI required significantly less chair time when compared to other isolation systems. In our study, the mean chair time required was reduced from 4.20 minutes for the RDI to 3.59 minutes for the DSI with an average difference of 0.91 minutes. Alhereky et al., 2014 reported that the chair time was reduced from 19.36 minutes with RDI to 10 minutes with ISI with an average difference of 10 minutes [3].These differences can be attributed to the previously mentioned study in which the FSs were applied on permanent first molars, whereas for our study they were applied on premolars that were smaller and easier to reach by the operator. Also, they included the chair time required for the application of topical anesthesia before RD clamp application in the control group and the time required to assemble the ISI in the test group. In contrast, in our study, neither topical nor local anesthesia was applied in the control group premolars prior to RD clamp application and the time required to assemble the DSI in the test group was not included.
Noise is considered a stress-triggering factor that involves fear and anxiety, especially among children [10]. Our study and previously published studies [3,6] reported that children were significantly more annoyed by the noise associated with DSI and ISI compared to other isolation systems.
During the insertion of the DSI, the patient was instructed to open his/her mouth wide and the tongue retractor portion of the DSI was inserted in the tongue vestibule, and the check retractor was inserted into the buccal vestibule. This explains why children in our study reported slightly more stretching of their lips and cheeks and more pressure on their tongue with the DSI compared to the RDI, which agrees with the study reported by Alhereky et al., 2014 [3].
Measuring pain is a difficult and complex process [11]. In our study, the pain was measured by utilizing a subjective tool that might provide inaccurate or false results [12], especially among pediatric patients. Therefore, studies in which pain is measured by both subjective and objective measures are recommended to obtain a more reliable outcome.
Almost equal numbers of children preferred DSI or RDI as their dental treatment and few felt there was a difference between both systems. Perhaps this is because although less chair time was needed for the DSI, but its noise had a major influence on children’s discomfort and future preference. Which emphasizes the importance of following the manufacturers’ recommended guidelines for the proper selection, insertion, and adjustment of the DSI mouthpieces to minimize the stretching and pressure caused by using the isolation system [3].
The prevalence children with sound first permanent molars was reported to be low among of 9-12-year-old children in Jeddah, Saudi Arabia. It was found that the prevalence was the highest (33%) among nine-year-old children and the lowest (17%) among 12-yearold children [13]. In addition, during regular screening for children attending KAAU pediatric dentistry department, most of the examined 9-15-year-old children were usually high-risk and their first permanent molars were either carious or already restored and the application of FS on newly and full erupted premolars is an essential part of dental preventive programs for this group of children [14]. Therefore, our study aimed to compare he DSI isolation system to the RDI during premolar fissure sealant placement.
All of the included subjects were cooperative and most of them had a previous experience with the dental isolation system. But the influence of their behavior and previous experiences on their preference was not investigated. Therefore, further studies involving children with different behaviors and previous experiences with dental isolation system are recommended.
In our study, both treatments were provided during the same appointment by the same operator to enhance or make it easier for the participants to compare both isolation systems and to indicate their future personal preference. Also, McNemar and Wilcoxin Signed Rank and GEE tests were used to estimate the effects of the isolation system on different variables while controlling for age and gender.
More randomized clinical trials with a larger sample size and different behaviors, as well as longer follow-up periods to evaluate the success rate of different treatment modalities, are required to compare each patient’s satisfaction and future preferences with DSI.
Conclusion
Based on the study’s results, the following conclusions can be made:
1. The use of Dry Shield isolation during fissure sealant application on premolars is associated with a significant reduction in chair time compared to the rubber dam isolation.
2. Dry Shieled isolation can be used as an alternative to the rubber dam isolation among pediatric patients.
References
- Reid JS, Callis PD, Patterson CJW. Rubber dam in clinical Practice. London; Chicago: Quintessence 1990.
- Hill EE, Rubel BS. Do dental educators need to improve their approach to teaching rubber dam use?. J Dent Educ 2008; 72:1177-1181.
- Alhareky MS, Mermelstein D, Finkelman M, et al. Efficiency and patient satisfaction with the isolite system versus rubber dam for sealant placement in pediatric patients. Pediatr Dent 2014; 36:400-404.
- Simonsen RJ. Pit and fissure sealant: Review of the literature. Pediatr Dent 2002; 24:393-414.
- Deery C. Caries detection and diagnosis, sealants and management of the possibly carious fissure. Br Dent J 2013; 214:551-557.
- Collette J, Wilson S, Sullivan D. A study of the Isolite system during sealant placement: Efficacy and patient acceptance. Pediatr Dent 2010; 32:146-150.
- Lyman T, Viswanathan K, McWhorter A. Isolite vs cotton roll isolation in the placement of dental sealants. Pediatr Dent 2013; 35:E95-9.
- Maslamani M, Mitra AK. Factors associated with patients’ satisfaction of rubber dam use during root canal treatment. Indian J Dent Res 2018; 29:144-149.
- Schulz KF, Altman DG, Moher D. Consort 2010 statement: Updated guidelines for reporting parallel group randomised trials. Ital J Public Health 2010; 7:325-332.
- Belcheva A, Shindova M. Subjective acceptance of pediatric patients during cavity preparation with Er:YAG laser and conventional rotary instruments. J IMAB Annu Proceeding 2014; 20:631
- Zarbock SF. Pediatric pain assessment. Home Care Provid 2000; 5:181-184.
- Merkel S. Pain control. Pain assessment in infants and young children: The finger span scale. Am J Nurs 2002; 102:55-56.
- Al-Samadani KH, Ahmad MS. Prevalence of first permanent molar caries in and its relationship to the dental knowledge of 9-12-year old from Jeddah, Kingdom of Saudi Arabia. ISRN Dent 2012; 2012:391068.
- Nowak AJ, Christensen JR, Mabry TR, et al. Pediatric dentistry: Infancy through Adolescence. 6th Edn: Philadelphia, PA: Elsevier 2019.
Author Info
Sara M Bagher*, Hanaa K Allaf, Layla N Khogeer and Osama Felemban
Department of Pediatric Dentistry, King Abdulaziz University, Jeddah, Saudi ArabiaCitation: Sara M Bagher, Hanaa K Allaf, Layla N Khogeer, Osama Felemban, Patient Satisfaction and Preference with Dry Shield vs. Rubber Dam Isolation among Pediatric Patients, J Res Med Dent Sci, 2021, 9 (3):82-90.
Received: 14-Feb-2021 Accepted: 08-Mar-2021 Published: 15-Mar-2021