Review Article - (2022) Volume 10, Issue 10
Paradigm Shift in Sterilization Protocol in Orthodontics Post COVID-19 Pandemic
Trupti Chikankar*, Pallavi Daigavane, Rizwan Gilani, Ranjit Kamble and Gayatri kale
*Correspondence: Dr. Trupti Chikankar, Department of Orthodontics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Demmed to be University) Sawangi (Meghe) Wardha, Maharashtra, India, Email:
Abstract
Sterilization is the process of removing all microorganisms from a product, surface, or medium, whether they are in vegetative or spore form. Every day, the orthodontist, or any clinician for that matter, and his employees are exposed to a wide range of patients with a variety of contagious diseases. Now in the current scenario, coronavirus disease is one of the most dangerous. Coronavirus disease 2019 (COVID-19) is a communicable infection. It is caused by the coronavirus. This causes Severe Acute Respiratory Syndrome (SARS-CoV-2). At the start of 2020, it became a global pandemic, hitting more than 200 nations and territories. The disease is extremely infectious, with asymptomatic carriers, including kids, being recorded as disease carriers. For an orthodontist and his staff, the working distance is in inches. For them, it is not possible to follow this protocol of social distancing in the clinic with their patients. This article discusses several sterilizing procedures while concentrating on the principles for a successful and efficient orthodontic practice.
Keywords
Sterilization, Orthodontics, COVID-19, Infection control, Pandemic
Introduction
Dental treatment includes numerous procedures like RCT (Root Canal Treatment), implants, orthodontic treatments, oral surgery, and many more. Each of these dental procedures entails operational tools and devices coming into touch with the sterile/unstable oral cavity of the patient. The transfer of harmful germs, which can cause infection, is a major danger of all such treatments. Transmission via contaminated medical and surgical devices is possible if equipment is not thoroughly disinfected or sterilized [1,2].
In order to protect both the physician and the patient, disease control is critical and the only tool in avoiding the spread of infectious illness. This is especially important in dentistry since the mouth cavity contains more microbes than just about any other portion of the body. Dental professionals (dentists, dental assistants, and dental hygienists) have the greatest infection risk than any health care worker. Dental professionals are in direct contact with patients and exposure to splatter of patient's saliva, aerosol and fluids are the primary sources of nosocomial infection [3]. It appeared in a research that "orthodontists seemed to have the 2nd highest prevalence of Hepatitis B among other dental professionals [4].
In the current scenario of COVID-19, not only infectious illness transmission is a concern, but the transmission of COVID is also a major concern. As a result, the general public is recommended to minimise contact among individual and keep a safe distance of 1-2 m between persons. Unfortunately, owing to the sensitivity of the orthodontic treatment, this puts the orthodontist and dental attendant at substantial threat of infection. Hence, this recommendation cannot be fully implemented in an orthodontic clinic. It thus becomes mandatory on a part of every dentist/orthodontist to follow the SOP and protocol meticulously post COVID to avoid life threatening situations [5].
Literature Review
The following review will highlight the need in change in the SOP of infection control and cautious methods of sterilization to be followed in an orthodontic clinic.
Sterilization
Sterilization is a process performed to prevent hazardous microorganisms from spreading and causing illness. It is described as any technique that efficiently kills or gets rid of all microorganisms (excluding prions) from a surface, surgical instruments, food, medication, or biological culture medium either in vegetative or spore form [6]. The sterilizing procedure can aid in the prevention of the spread of COVID, not only COVID but also other infectious disease.
Sterilization can be achieved by variety of methods. Ethylene oxide sterilization, chemical vapour sterilization, dry heat sterilization, and steam autoclave sterilization are some of the most popular methods used in orthodontic treatment.
Ethylene oxide sterilization: At room temperature, ethylene oxide is a very penetrating gas. It works by alkylating protein amino, carboxyl, and sulfhydryl groups. It binds to both RNA and DNA. Heat sensitive devices are sterilized using this solution.
The sterilization SOP and protocol
The way an object is used is the most important aspect in deciding whether it has to be sterilized, disinfected or just cleaned.
According to the Spaulding method, orthodontic instruments are classified into three types:
• Critical instruments are those that enter soft tissue (mucosa or skin) or bone in the mouth [7]. After each usage, these tools must be sterilized or disposed of such as Bands and band removers, orthodontic miniimplant placement kit, band forming pliers, ligature directors, etc. [8].
• Semi-critical instruments are those which interact with mucous membranes or intact skin but are not designed to penetrate oral soft tissues or bone, e.g., mainly orthodontic tools, retractors, mouth mirrors etc. Although these items provide a significantly lesser risk of disease transmission, they should nevertheless be sterilised after each use as the majority of semicritical equipment in dentistry are heat tolerant.
• Least critical instruments that don’t touch mucous membrane Such as arch forming and V-bend forming pliers, bracket positioning gauges, Distal-end and ligature cutter, torquing keys, etc. should be disinfected.
A new form of coronavirus emerged in Wuhan in December 2019 and quickly spread throughout China.
Later, verified instances were recorded in various parts of the world [9]. The majority of those who became infected with the virus developed mild to moderate respiratory disease and recovered without the need for additional treatment. Some, though, fell very sick and required medical assistance. To minimise COVID spread, dental practitioners should grasp how COVID transmission occurs, how to encounter patients with COVID disease, and what additional precautions must be performed during practise [10]. The COVID has changed all the perceptions of following the SOP for sterilization all over the world. There by CDC and WHO advised meticulously change in the sterilization protocol post COVID.
Infection rates are greater in the hospital working environment than in the general population. Working environments have a greater prevalence of invasive operations, patients are exposed to the outside environment for extended periods of time and there is a danger of disease transmission.
• Patient to operator
• Operator to Patient
• Patient to Environment
• Environment to patient
There are several high risk places in an orthodontic working place that can lead to infection transmission. The following are some of the high risk areas:
• OPD area
• Biomedical area
• Spittoons
• Impression storage area
• Cast storage areas
• Instruments and material table
In these high risk areas, the following general principles must be followed:
• Standard precautions: All staff members should use standard precautions while dealing with patients
• Hand washing: The importance of this in healthcare settings cannot be overstated. It is necessary to use Sterilium hand massages between patients and before invasive operations.
• Aprons and gloves: When necessary, the operator wears aprons and gloves. Gloves must be mandatory for examination (examination gloves) and invasive treatments (sterile gloves).
• Mask: A mask is used mandatorily while treating patients who may be exposed to airborne diseases.
• Goggles: Goggles are worn when there is a chance of a splash while scaling, bonding and use of aerosol generating instruments or when dealing with UV light.
All these are called as barrier control.
Barrier control protection is provided against a wide spectrum of possible infections that come across during patient treatment. Physical barriers such as face masks, safety glasses, head caps, disposable gloves and hospital gowns are used throughout treatment operations to prevent infection exposure.
Protective eye wear: According to study by Sun, et al. that there might be a slight chance of transfer of virus through eye as a droplet or aerosol into the body [11]. During work, the operator is advised to wear safety glasses. As sharp tools, hand pieces, arch wires and other items are constantly passed over the patients' faces, it is recommended that patients wear protective eyewear as well. It is no longer suggested that a patient's spectacles be removed during the procedure for the sake of comfort.
Masks: Masks can serve at least two purposes in the control of transmission of the virus in the general public [12]. For starters, masks can have an effect on turmoil gas cloud cover and emission of breathing microbe [13].
According to research, masks can either prevent the quick turbulence jets produced by sneezing or spitting or divert the jets in significantly lesser hazardous ways to limit airborne illness [14]. Second, virus particles (aerosols or droplets) can be filtered by the mask layer [15]. The operator is protected from microbe-laden aerosolized droplets by wearing a face mask. The proposed mask should filter out 95% of droplets with a diameter of 3.0 to 3.2 microns. The mask should cover the complete face's perimeter. It is advised to switch masks between patients.
Points to consider before using a mask:
• While evaluating any patient, a mask must be worn.
• While utilising hand pieces, air/water syringes, or scalars, by the assistance.
• Instruments that have been infected should be washed.
• When either the patient or the operator has a respiratory condition.
• For each patient, a fresh mask is utilised.
• During treatment or when removing the mask, do not contact the mask's body with your exposed hands.
Head coverings: Head coverings act as an important barrier.
Steps in infection control in a clinic
Patient screening: Screening of patient which includes medical history of the patient can help to assist factors that can help in diagnosis of systemic or oral disorders. Most patients fail to provide the necessary information. Every person is treated as though he/she has contracted an infection. Universal precautions are a crucial basic application of preventing infection. Restriction of blood and fluids reduces clinical guesswork about a patient's infection condition significantly.
Personal protection: Continuous contact with body fluids (saliva and blood) during procedures may expose operator’s immune system to a wide spectrum of pathogenic agents. Immunological and barrier protection are essential in this situation. One must monitor that:
• Scrubs are cleaned every day.
• Short nails recommended. It is to minimise rips in gloves. It also helps to reduce the likelihood of patient discomfort due to long nails. Watches and accessories of hand are prohibited.
• Hands are cleansed prior to the patient wearing gloves, and they are also washed when the gloves are removed. If the treatment took more than 15-20 minutes, it is advised that you wash your hands. Hand sanitizer is advised for normal OPD patients in between patients.
• Gloves are changed after each patient and are replaced if they become damaged or noticeably filthy while working on a single patient.
• Before therapy, the patient should rinse his or her mouth with an antibacterial mouthwash.
• In the lab, protective eyewear is used.
• Splashes from the lathe or other by products are avoided as much as possible either on flooring or the table.
Washing and care of hands is advised in the following way
• Before putting on gloves wash and care for your hands to eradicate transitory bacteria and diminish residual micro flora.
• Remove any microorganisms that may have invaded the gloves via microscopic defects or rips, as well as any remaining micro-flora growth that may have occurred.
• When doing typical orthodontic operations, hand cleaning takes roughly 40-45 seconds. Disposable paper towels are used to dry hands, followed by the application of disposable gloves.
Clinical attire is required. When operating rotating instruments, a scrub/uniform is worn. Lab coats and aprons are used with caution. Personnel don’t dress clinic clothes to and from work. When evaluating patients or working in the laboratory, aprons must be worn. These processes invariably introduce germs into the fabric of the apron.
The surveillance of infection control protocols must be a mandatory step in the infection control policy.
High-risk areas are an important area of targeted surveillance activities:
• Infection control workers and clinicians work closely with the Infection Control Department to monitor record and analyse infections in high-risk regions.
• Active surveillance is required for:
• Infections acquired in the hospital
• Needle stick injuries
• Environmental surveillance
Monitoring the efficacy of housekeeping services is one type of surveillance activity. Register must be maintained in the working/registration counter for daily monitoring and the personnel must be assigned to monitor on a daily basis.
Methods for cleaning blood spills and body substances during the procedures. It is recommended to:
• Use a 1% sodium hypochlorite solution to clean up spillage.
• Use a disinfectant cleaning solution to wipe up spills of fluids (blood, body fluids and other potentially contagious fluids) as soon as possible.
• Immediately cover the area with any absorbent material, such as gauze piece, old newspaper or tissue paper.
• To clean up small spills, use a towel soaked in a 1% sodium hypochlorite solution while wearing utility or examination gloves. Then clean with a disinfectant solution.
• For major spills, pour the area with a 1% sodium hypochlorite solution while wearing gloves. After sweeping up the solution, clean as usual with water detergent solution.
Note: After pouring the chlorine solution, wait a few minutes, ideally 15 minutes. Following disinfection, the floor must be thoroughly cleaned with soap and water.
The dental practise is completely dependent on technical use of instruments without which no procedure can be done in a dental clinic. It is important to have thorough knowledge regarding the sterilization sand disinfection of dental armamentarium (Table 1).
| S. no | Instrument | Suggested protocol for sterilization and disinfection |
|---|---|---|
| 1 | Operatory Chair, Chair switches, Light handles, Equipment trolley handles, Three-way syringes IOPA viewer, Dental Chair lights, buttons, instrument holder, Clinician chair | Wipe with sterile cotton/tissue paper using the following recommended preparations 1. A solution prepared by adding (15 ml) Dettol Multipurpose Hygiene Liquid (4% Benzalkonium Chloride) to 1 L water. 2. 2 % gluteraldeyde solution 3. When the surface is visibly contaminated with blood use spirit preferably. Sanitization of chair-once daily before starting with the first patient. |
| 2 | Drawer handles, pens, other surfaces touched with gloved hands | Cleaning and dusting |
| 3 | Patient drapes | 1. Cloth material: Wash and autoclave 2. Plastic material: Clean, rinse with dettol 2 % gluteraldeyde solution. Either discard/reuse |
| 4 | Patient viewing mirrors | Wipe with spirit using sterile cotton. |
| 5 | Countertops, Washbasin and taps in cabinets | Clean with detergent. When the surface is visibly contaminated with blood use spirit/H2O2. |
| 6 | Patient tumbler | Wash with detergent solution. |
| 7 | Hand Towel | Wash with detergent, rinse with Dettol (preferably use paper napkins/tissue paper) |
| 8 | Spittoons | Scrub and wash with detergent after every patient. If any blood stains are there, use H2O2/sodium hypochlorite and later wash with detergent. |
| 9 | Suction tips | Reusable steel suction tips: washed with detergent and autoclaved Disposable: Change for every patient, discard in Red dustbin. |
| 10 | Ultrasonic scaler unit | Tips are cleaned and autoclaved after every use the unit and cables are cleaned using bacillol/H2O2 spray |
| 11 | Handpiece-Airrotor, Contrangle and Straight headpieces of micromotor | Cleaning followed by Autoclave |
| 12 | Light cure unit Spot welders | Bacillol |
Table 1: Instruments and recommended sterilization protocol.
Sterilization-capable items: Gauze, cotton, linen, needles, syringes, auto clavable hand parts, gloves, imprint trays and so on.
Cold sterilisation is recommended as follows: Sterilization is accomplished by immersing the articles to be sterilised in chemicals. Chemical sterilising methods include absolute alcohol (2%), gluteraldeyde (2%), (Cidex), formaldehyde, bacillol, bio shield Ethylene Trioxide (ETO) and others.
Disinfection: Dental chair, tables and working surfaces also other operatory materials, surfaces and orthodontic equipment’s that cannot be consistently sterile, should be disinfected [16].
Cleaning surfaces after each patient and applying disinfectant chemical substance are both part of the disinfection process. Alcohol, synthetic phenols, gluteraldeyde and other substances are among them.
Cleaning of all water pipelines for few minutes (3-5) that has been inactive for a while. Run high-speed headpieces for at least half minute after each patient to release water and air to clean out any patient material that may have entered during the treatment. Water pipes may be disinfected on a regular basis by running a disinfectant solution through them while the unit is turned off.
Cleaning the waterline of the dental unit: At the end of the day, it is advisable to vacuum around one litre of 1%sodium hypochlorite via the suction line and leave it overnight. The next day, before commencing the task, give it a good rinse with water and put it to use.
The following review will discuss about the protocol and sop of sterilization along with sterilization of orthodontic armamentarium.
Orthodontic pliers: Stainless steel pliers of high grade may be sterilised using chemical vapour, steam, dry heat and ethylene oxide gas. “Steam autoclave” is not recommended for low-quality pliers because it might harm the material. Ethylene oxide sterilisation is the only viable procedure for pliers with plastic components [17].
Orthodontic wires: A study by Smith, et al. suggests effects of clinical usage and various disinfection and sterilization techniques on 3 types of nickel-titanium arch wire, as well as one type of titanium arch wire and one type of stainless steel arch wire. Disinfection was used alone or in combination with sterilization/disinfection processes such as steam autoclave, dry heat or cold solution sterilisation [18].
Ligatures: Metal and elastomeric ligatures have the potential to be agents of infectious disease transmission. Cross-contamination in the orthodontic clinic is a big problem since cold sterilisation might degrade the elastomeric material. Mulick advocated for single-use elastomeric material dispensing to avoid interaction of canes or sticks with infected hands [19].
Orthodontic bands: They are cleaned with ultrasonic cleanser and then with disinfectant solution as suggested by manufacturer after testing them on patient. Then they are placed back in the box.
Orthodontic brackets: These brackets can lose its clinical efficacy if are reused, hence reuse is not advisable. Also there is threat of infection spread. A research was conducted by Speera, et al. to assess the effect of 0.01%chlorohexidine disinfection solution on bond strength of ceramic and metal brackets and concluded that chlorohexidine has no significant influence on ceramic and metal bracket adhesion ability. As a result, chlorohexidine is the disinfection of choice for ceramic and metal brackets [20].
Rubber products and saliva ejectors: They should be discarded after each usage. Rubber materials are inefficient for ethylene oxide sterilisation. They might be harmed by moist or dry heat sterilisation.
Hand pieces: Hand pieces can be sterilised using steam, dry heat, chemical vapour or ethylene oxide.
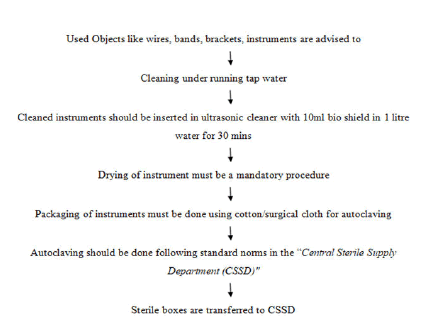
As the pliers used in orthodontics are expensive but still, it must be mandatory for every orthodontist to have 3 sets of each instrument. In orthodontics Stainless Steel material is advised to recycle. Procedure for recycling of used instrument as follow:
Disinfection of instruments: Tying pliers, torqueing keys, ligature tier and distal end cutter, elastomeric rings, arch forming pliers, boons gauge and other less important tools are cleaned and disinfected. Removable appliances are disinfected in separate 2% gluteraldeyde containers during the appointment to limit the quantity of bacteria at the source.
Practices in the dental laboratory: Before being sent to the laboratory imprints bite records, and devices implanted in patients' mouths are properly cleansed with H2O2 spray to remove debris, saliva and blood. Then disinfect it by immersing in appropriate disinfection agent like sodium hypochlorite.
Casts/impressions
The following procedure is recommended for disinfecting impression:
• Immersion in a chemical disinfectant, such as sodium hypochloride, for 30 minutes. Furthermore, despite the fact that it is ineffective against HIV and HBV, glutaraldehyde is commonly used.
• 2% gluteraldeyde–spraying of a disinfectant on the impression.
Alginate impression disinfection procedure
• Under running water, rinse the impression thoroughly and shake it to remove excess of water.
• To achieve optimum disinfection, immerse the impression in a 1:10 solution of sodium hypochlorite for few seconds.
• Removing the imprint and carefully rinsing it under running tap water.
Infectious germs may be present in dental casts made from impressions, or wax bite records from patients may cause contamination to dental castings. During mixing, disinfectant like gluteraldeyde can be added to clean these dental castings.
Statutory provisions regarding the management and disposal of Bio-Medical Waste (BMW)
Biomedical waste is waste formed during animal or human research procedures such as diagnosis, treatment, or vaccination, or in the testing or manufacturing of biological products in health camps [21]. BMW generated in dental office include cotton, plastic, glass, amalgam waste, X ray processing solutions, mercury, lead foils, chemicals, disinfectants, dental casts and impressions, latex, waste sharps like dental materials, human tissues, blades, discarded/expired medicines, extracted tooth and surgical needles. All these materials pose high risk as they are blood and saliva contaminated which carry disease spreading microorganisms [22]. If not handled properly, this can be damaging to the environment and individuals who come into touch with the materials. To avoid negative impacts on health and the environment, correct segregation protocols must be followed.
Principles of waste management
• Develop a waste management strategy based on an assessment of the present situation and aimed at reducing trash generation.
• Separate clinical (infectious) trash from nonclinical waste and store them in separate containers.
• Dedicated garbage trolleys are used to transport rubbish.
• Keep garbage in designated places with limited access.
• Gather sharps and place them in sharps containers. Containers for sharps should be constructed of plastic and have a closable cover. A biohazard sign should be placed in the storage rooms.
• Make sure that the carts or trolleys used for transporting segregated garbage collection aren't being utilised for anything else and that they're being cleaned on a regular basis.
• Determine a waste storage place prior to treatment or transportation to the final disposal area.
Waste created in a hospital must be separated and kept in distinct containers according to the colour coding shown in the Table 2 below.
| Type of bag | Type of waste |
|---|---|
| Yellow bag | Cotton, gauze, cap, mask, alginate, plaster casts |
| Red bag | Gloves, modules, e-chain, separators |
| Blue bag | TAD’s |
| White bag | Wires, ligatures, brackets, band material |
| Gray bag | General wastes like GIC papers, mixing pad |
Table 2: Waste created in a hospital must be separated and kept in distinct containers according to the colour coding.
Material disposal
• Black container: Impression material and dental casts (Discarded/Used) should be immersed in a 1% Sodium hypochlorite solution bucket for 24 hours and then discarded, head cap, and shoe covers.
• Red container: Gloves, button and other attachment, elastic ligatures, de-bonded brackets, elastics, wax bite registration, mouth mask, ligatures.
• Yellow container: Infected cotton.
• Sharp container containing 1% sodium hypochlorite: Removable Appliances with wire component (Used/broken items are no longer used by the patient.), needles after being burnt, wires, orthodontic mini implants, steel ligatures
• Storage: The BMW cannot be kept at the hospital for more than 48 hours. Doing the BMW on a regular basis is good.
If it is to be held for final disposition, it must be done so carefully, ensuring that:
• The storage space is in an isolated, distant area.
• The space is properly fenced and locked.
• To prevent spillage and infection dissemination by vectors, the BMW should be contained in rigid or semi-rigid, leak-proof containers (flies).
• The sign of a “Hazardous BMW” must be widely displayed, as well as a warning message in the local language.
Mercury hygiene and waste mercury disposal must be given special consideration.
Discussion
The COVID-19 outbreak has had a significant impact on all dental health practitioners and orthodontists. Following this pandemic, it is very important that orthodontics and along with the co-worker should follow strict infection control measures and sterilization protocol to avoid cross contamination among patients and for their safety too. The infection control measure should include wearing of eye wear, facemasks, face shield, PPE and try to use disposable instruments wherever possible. A typical clinical screening approach should include efficient telescreens and triaging. Any patient suspected of having COVID-19 should be sent right away to the COVID-19 screening unit. Sterilization protocol include sterilization and disinfection of all instruments, also cleaning surfaces after each patient and applying disinfectant chemical substance are both part of the disinfection process. Alcohol, synthetic phenols, gluteraldeyde, and other substances are among them. Gloves are changed after each patient and are replaced if they become damaged or noticeably filthy while working on a single patient. Sterilization is accomplished by immersing the articles to be sterilised in chemicals. Chemical sterilising methods include absolute alcohol (2%), gluteraldeyde (2%) (Cidex), formaldehyde, bacillol, bio shield Ethylene Trioxide (ETO), and others.
Conclusion
Sterilization should be routinely monitored as part of professional job. The implementation of sterilising procedures in the care of all patients reduces exposure of working area to microbiological infections significantly. Here, as mentioned in article, it must be made mandatory protocol to prevent exposure of COVID-19 to the operator or the patient. It is the responsibility of every orthodontist and clinician to conduct his practise in such a way that no one is harmed. By following the SOPs, one can reduce, if not eliminate, the likelihood of COVID-19 spread in their workplace.
References
- Epstein L, Hunter JC, Arwady MA, et al. New Delhi Metallo-β-Lactamase–Producing Carbapenem-Resistant Escherichia coli Associated With Exposure to Duodenoscopes. JAMA 2014; 312:1447–1455.
- Wendorf KA, Kay M, Baliga C, et al. Endoscopic retrograde cholangiopancreatography-associated AmpC Escherichia coli outbreak. Infect Control Hosp Epidemiol 2015; 36:634–642.
- Ge Z, Yang L, Xia J, et al. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J Zhejiang Univ Sci B 2020; 21:361–368.
- Turkistani KA. Precautions and recommendations for orthodontic settings during the COVID-19 outbreak: A review. Am J Orthod Dentofacial Orthop 2020; 158:175–181.
- Matthews IP, Gibson C, Samuel AH. Sterilisation of implantable devices. Clin Mater 1994; 15:191–215.
- Indian Dental Association. Sterilization and Disinfection.
- National Center for the Chronic Disease prevention and Health Promotion. Sterilization and Disinfection of Patient-Care Items and Devices. Division of Oral Health, 2021; 1-26.
- Kalra S, Tripathi DT, Rai DP. Infection Control in Orthodontics. J Orthod Endod 2015; 1:12.
- Wan XY, Luo W, Dong Z, et al. Current practice and potential strategy in diagnosing COVID-19. Eur Rev Med Pharmacol Sci 2020; 24:4548-4553.
- Pangilinan P, Manzano P, Arnold J, et al. Orthodontics in the COVID-19 Era: The Way Forward Part 1 Office Environmental and Infection Control. J Clin Orthod 2020.
- Morag. Eye protection equipment for preventing transmission of COVID-19 in primary care National Elf Service. The Dental EIF, 2020.
- Singh KR, Kamble SD, Kalbande SM, et al. A Review on COVID-19 Face Mask Detection using CNN. J Pharma Res Int 2021; 39–45.
- Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions: Potential implications for reducing transmission of COVID-19. JAMA 2020; 323:1837-1838.
- Tang JW, Liebner TJ, Craven BA, et al. A schlieren optical study of the human cough with and without wearing masks for aerosol infection control. J R Soc Interface 2009; 6:727–736.
- van der Sande M, Teunis P, Sabel R. Professional and Home-Made Face Masks Reduce Exposure to Respiratory Infections among the General Population. PLoS One 2008; 3:2618.
- Motwani N, Ikhar A, Chandak M,et al. Disinfection Measures during COVID-19 for Dental Operatories. Open Dent J 2021; 15.
- Centers for Disease Control and Prevention (CDC). Infection Prevention and Control in Dental. Department of Health & Human Services, 2019;
- Smith GA, Fraunhofer JA von, Casey GR. The effect of clinical use and sterilization on selected orthodontic arch wires. Am J Orthod Dent fac Orthoped 1992; 102:153–159.
- Mulick JF. Upgrading sterilization in the orthodontic practice. Am J Orthod 1986; 89:346–351.
- Speer C, Zimny D, Hopfenmueller W,et al. Bond Strength of Disinfected Metal and Ceramic Brackets: An In Vitro Study. Angle Orthod 2005; 75:836–842.
- Datta P, Mohi G, Chander J. Biomedical waste management in India: Critical appraisal. J Lab Physicians 2018; 10:006–0014.
- Benakatti V, Kanathila H. Biomedical waste management in dental office-a review. World J Adv Healthcare Res 2018; 2:177-181.
Author Info
Trupti Chikankar*, Pallavi Daigavane, Rizwan Gilani, Ranjit Kamble and Gayatri kale
Department of Orthodontics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Demmed to be University) Sawangi (Meghe) Wardha, Maharashtra, IndiaCitation: Trupti Chikankar, Pallavi Daigavane, Rizwan Gilani, Ranjit Kamble, Gayatri kale, Paradigm Shift in Sterilization Protocol in Orthodontics Post COVID-19 Pandemic, J Res Med Dent Sci, 2022, 10 (10): 155-161.
Received: 02-Aug-2022, Manuscript No. JRMDS-22-49462; , Pre QC No. JRMDS-22-49462(PQ); Editor assigned: 04-Aug-2022, Pre QC No. JRMDS-22-49462(PQ); Reviewed: 18-Aug-2022, QC No. JRMDS-22-49462; Revised: 03-Oct-2022, Manuscript No. JRMDS-22-49462(R); Published: 13-Oct-2022
