Research - (2021) Volume 9, Issue 1
Oral Rehabilitation with Telescopic Overdenture-A Case Report
Sanjana Devi*, Deepak Nallaswamy and Revathi Duraisamy
*Correspondence: Sanjana Devi, Department of Prosthodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Science, Saveetha University Tamilnadu, India, Email:
Abstract
Any procedure that can delay or eliminate potential future problems come under preventive prosthodontics. In scenarios with few remaining natural teeth, prosthodontists are posed with a dilemma for the treatment options. In such cases, treatment with overdentures has been proven to be advantageous. This gives the patient a lot of advantages like better stability, proprioception, support among a few. A telescopic overdenture is a removable prosthesis that has a primary coping on the teeth and a secondary coping in the denture. The primary copings are full-coverage parallel-milled copings that are cemented to the prepared teeth. The secondary coping fits over the primary coping. It works by the application of interfacial surface tension and friction fit mechanism of retention using double copings. They are, however, indicated only for patients with multiple abutments distributed bilaterally along the dental arch. This clinical report describes the prosthetic rehabilitation of a patient with only a few remaining teeth in the mandible, and all the teeth were on one side of the arch.
Keywords
Telescopic denture, Telescopic overdenture, Attachment, Overlay prosthesis
Introduction
Any procedure that can delay or eliminate potential future problems come under preventive prosthodontics. Retention of teeth offers a variety of advantages like proprioception, better stability, support, and retention. Alveolar bone is also preserved [1,2]. When only a few teeth are remaining in the arch, we can go for either a fixed or removable prosthetic option. However, bridges and implants are not always an option for several patients. Reasons can vary from socioeconomic conditions, anatomic conditions, systemic conditions, or the patient’s attitude toward dental implants. In such cases a removable prosthesis would be ideal [3-5]. But patients are not always satisfied with removable dentures due to excessive tissue coverage, lack of retention, etc. A telescopic overdenture can overcome these problems [6,7].
A telescopic overdenture is a removable prosthesis that has a primary coping on the teeth and a secondary coping in the denture. The primary copings are full-coverage parallel-milled copings that are cemented to the prepared teeth. The secondary coping fits over the primary coping. It works by the application of interfacial surface tension and friction fit mechanism of retention using double copings. This increases retention and stability. It is otherwise known as overlay denture, overlay prosthesis and superimposed prosthesis [8-11].
They work by transferring the forces along the long axis of the abutment teeth and prevent dislodgement of the denture. It can also be used in patients with reduced and residual dentition as it gives an opportunity to reduce destructive rotational and horizontal occlusal forces by directing them more axially [12,13].
A major advantage of telescopic overdentures is that it can be used in periodontally compromised patients as well, as it disperses the forces and prevents pathological migration of teeth. They are, however, indicated only for patients with multiple abutments distributed bilaterally along the dental arch [14,15].
Previously our department has published extensive research on various aspects of prosthetic dentistry [16-26] this vast research experience has inspired us to research about this topic. Considering the above factors discussed, this clinical report describes the prosthetic rehabilitation of a patient with only a few remaining teeth in the mandible, and all the teeth were on one side of the arch.
Case Report
A 62-year-old patient reported to the Department of Prosthodontics with a chief complaint of multiple missing teeth and a desire to improve chewing and esthetics. History revealed the patient was a smoker for the past 21 years. Extraoral examination revealed a convex profe and a normal temporomandibular joint. On intraoral examination there was missing 15, 16, 17, 23, 27, 31, 32, 33, 34, 35, 36, 37, 41, 42, 46, 47 and non-vital 12, 13, 14, 21, 24, 25, 26.
Patient underwent periodontal therapy - scaling, root planning and flap surgery to save the remaining teeth. This was followed by root canal treatment of 12, 13, 14, 21, 24, 25, 26. Diagnostic casts were prepared after taking alginate impressions. Temporary denture base and wax occlusal rim was fabricated on the mandibular diagnostic cast. The occlusal rim was used to determine the vertical dimension of occlusion, prior to tooth preparation. Casts were mounted on a semi-adjustable articulator and were analyzed.
Various prosthetic options, including implant therapy, were given to the patient. The patient was interested in saving the remaining teeth and did not give a positive response for implants. Patient also had a removable partial denture previously and was not satisfied with it.
After consideration of all factors a treatment plan of fixed prosthesis irt 11, 12, 13, 14, 21, 22, 23, 24, 25, 26, with an attachment removable partial denture irt 15, 16, primary metal copings irt 43, 44, 45, 48 with a lower complete telescopic overdenture was planned (Figure 1).
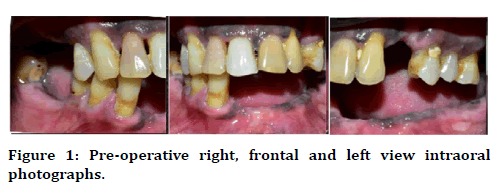
Figure 1. Pre-operative right, frontal and left view intraoral photographs.
Tooth preparation was done in the maxillary and mandibular arch. After preparation of the abutments, impression was made using polyvinyl siloxane elastomeric impression material (putty and light body) by double step technique. Primary copings were fabricated on the master cast obtained and the fit of the copings were evaluated in the patient’s mouth, after which they were cemented on the abutments with glass ionomer cement. At the same time, metal trial for the maxillary arch was done and maxillomandibular relationship was assessed using occlusal rims.
Bisque trial for upper arch along with a Kennedys class 2 RPD irt 16, 17 was done along with wax trial of lower telescopic complete denture. Occlusion along with protrusive and laterotrusive movements were assessed. The RPD and complete denture were processed with heat cure acrylic while the ceramic was glazed. A follow up of 1 year revealed no prosthetic complication and complete patient satisfaction (Figures 2-4).
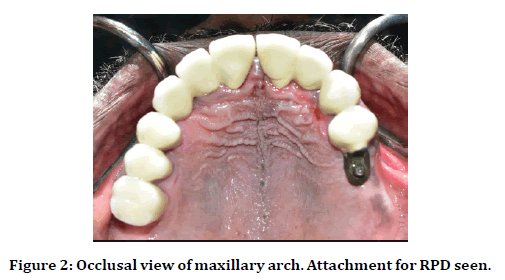
Figure 2. Occlusal view of maxillary arch. Attachment for RPD seen.
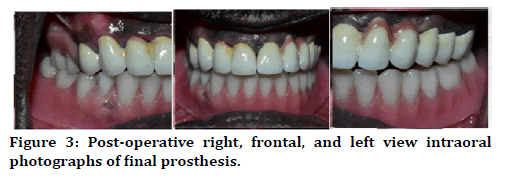
Figure 3. Post-operative right, frontal, and left view intraoral photographs of final prosthesis.
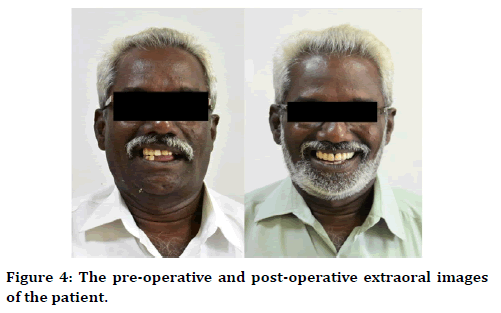
Figure 4. The pre-operative and post-operative extraoral images of the patient.
Discussion
In this case, considering the age of the patient and his habits, implant supported prosthesis was ruled out as a treatment option for the patient. A telescopic denture was chosen as a favorable treatment option for mandible, even though it is usually indicated for patients with multiple abutments distributed bilaterally along the dental arch. This overcame many of the problems posed by conventional complete dentures like progressive bone loss, less retention and stability, loss of periodontal proprioception and low masticatory efficiency. It also helped in better distribution of forces [27,28].
It is a known fact that the residual alveolar ridge undergoes rapid loss in all dimensions [29]. The residual ridge resorption (RRR) is said to be rapid, progressive, irreversible, and inevitable. It has been well observed and documented in the literature [29-32]. However, it was also observed that bone is maintained around standing teeth and implants [33,34]. Therefore, retaining teeth as overdenture abutments slows down the rate of alveolar resorption [35]. A study by Crum et al. concluded that patients treated with complete maxillary dentures and mandibular overdentures demonstrated less vertical alveolar bone reduction than patients with complete maxillary and mandibular conventional dentures [36].
Prosthetic rehabilitation with over dentures constitutes essentially a preventive prosthodontics concept, as it endeavors to preserve the few remaining teeth and the supporting structures [37]. The teeth which are generally too weak to support a fixed partial denture and are considered unsuitable abutments to support a removable partial denture can often at times be usefully conserved and suitably modified to act as abutments for over dentures for a useful span of time [38]. Proprioception, through the periodontal fibres, also gives the patient a sense of discrimination to touch and pressure, which is less with conventional complete dentures [39,40].
A telescopic overdenture is a removable prosthesis that has a primary coping on the teeth and a secondary coping in the denture. The primary copings are full-coverage parallel-milled copings that are cemented to the prepared teeth. The secondary coping fits over the primary coping. It works by the application of interfacial surface tension and friction fit mechanism of retention using double copings. The smaller the degree of the taper, the greater the frictional retention of the retainer. The average wall taper is a 6-degree angle. A longitudinal study conducted by Bhagat et al. stated that conical crown-retained partial dentures have a lower failure rate compared to those retained with clasps or precision attachments [41]. Stability is enhanced by the vertical component of the retained teeth. The copings are milled to exact configurations of taper angles of the walls with each other to create a common path of insertion for outer telescopic crowns of a retrievable superstructure [42-44].
Retrievability is the major advantage of telescopic overdenture, that is not available with a fixed prosthesis. It is a more versatile alternative for these patients because the prosthesis can be repaired without reconstruction of the entire superstructure. Patients should be given instructions regarding denture maintenance since distortion of an outer telescopic crown can reduce the retention of the prosthesis. They also promote oral hygiene and periodontal health because the abutments are more accessible for oral hygiene [45].
However, as it is an overdenture, its success depends on the continued retention of the underlying abutments. From the practitioner’s end, it becomes obligatory to periodically monitor their health and institute necessary steps to prolong their useful span. Periodical recall and review is of utmost importance [46].
Conclusion
Although the cost and number of appointments are higher with the overdenture treatment when compared with conventional complete dentures, it is justified as telescopic overdentures are a superior health service. Even with the increased use of implant supported overdentures, tooth supported telescopic overdentures can be an alternative treatment plan.
Acknowledgment
I would like to thank Saveetha dental college for providing me with the opportunity, knowledge, and guidance to complete this case. I would also like to thank my guide for guiding me through the entire process.
Conflict of Interest
There are no conflicts of interest.
References
- Soratur SH. Retention and stability. Essentials Prosthodont 2006; 24.
- Dl S, Sarandha DL. Retention, stability and support in complete denture treatment. Textbook of Complete Denture Prosthodontics 2007; 58–58.
- Akagawa Y, Rachi Y, Matsumoto T, et al. Attitudes of removable denture patients toward dental implants. J Prosthetic Dent 1988; 60:362-364.
- Bassi F, Mantecchini G, Carossa S, et al. Oral conditions and aptitude to receive implants in patients with removable partial dentures: A cross‐sectional study. Part I. Oral conditions. J Oral Rehab 1996; 23:50-54.
- Carr AB, Brown DT. Considerations for the use of dental implants with removable partial dentures. McCracken’s Removable Partial Prosthodont 2010; 338-45.
- Park C, Jun DJ, Park SW, et al. Use of polyaryletherketone (PAEK) based polymer for implant-supported telescopic overdenture: A case report. J Adv Prosthodont 2017; 9:74-76.
- Shruthi CS, Poojya R, Swati Ram A. Telescopic overdenture: A case report. Int J Biomed Sci 2017; 13:43.
- Abraham PA, Koka P, Murugesan K, Vasanthakumar M. Telescopic overdenture supported by a combination of tooth and an implant: A clinical report. J Indian Prosthodont Society 2010; 10:230-233.
- Dede DÖ, Cenk Durmuşlar M, Şahın O, et al. Telescopic overdenture and implant supported fixed partial denture: A pragmatic treatment approach. Case Reports Dent 2015; 2015:392397.
- Fernandes FL, Chaware SH. Telescopic overdenture–An overlooked treatment modality for partially edentulous patients: A case report. J Contemporary Dent 2018; 8:148-152.
- Laksono H. Telescopic overdenture as an aesthetic treatment for partially dentate patients–A case report. Indonesian J Dent Med 2018; 1:27-30.
- Tan AS, Walmsley AD. Mandibular implant-retained overdenture with magnets: A case report. Dental Update 2004; 31:104-108.
- Budihargono O, Hendrijantini N, Immediate complete overdenture for esthetic consideration of the upper edentulous ridge-A case report. Proceedings of the 7th International Meeting and the 4th Joint Scientific Meeting in Dentistry 2017.
- Kaira LS, Mishra R. Telescopic denture a treatment modalitity of preventive prosthodontics. Int J Oral Health Sci 2013; 3:121.
- Yarborough A, Cooper L, Duqum I, et al. Evidence regarding the treatment of denture stomatitis. J Prosthodont 2016; 25:288-301.
- Begum R, Ariga P, Jain AR. Evaluation of corrosive behavior of four nickel–Chromium alloys in artificial saliva by cyclic polarization test: An in vitro study. World J Dent 2017; 8:477–482.
- Ganapathy DM, Kannan A, Venugopalan S. Effect of coated surfaces influencing screw loosening in implants: A systematic review and meta-analysis. World J Dent 2017; 8:496–502.
- Jain AR. Clinical and functional outcomes of implant prostheses in fibula free flaps. World J Dent 2017; 8:171–176.
- Jain AR. Prevalence of partial edentulousness and treatment needs in rural population of south India. World J Dent 2017; 8:213–217.
- Ranganathan H, Ganapathy DM, Jain AR. Cervical and incisal marginal discrepancy in ceramic laminate veneering materials: A SEM analysis. Contemporary Clin Dent 2017; 8:272–278.
- Jain AR, Nallaswamy D, Ariga P, et al. Determination of correlation of width of maxillary anterior teeth using extraoral and intraoral factors in Indian population: A systematic review. World J Dent 2018; 9:68-75.
- Gupta P, Ariga P, Deogade SC. Effect of monopoly-coating agent on the surface roughness of a tissue conditioner subjected to cleansing and disinfection: A contact profilometric study. Contemporary Clin Dent 2018; 9:S122–S126.
- Anbu RT, Suresh V, Gounder R, et al. Comparison of the efficacy of three different bone regeneration materials: An animal study. Eur J Dent 2019; 13:22.
- Ashok V, Ganapathy D. A geometrical method to classify face forms. J Oral Bio Craniofac Res 2019; 9:232–235.
- Duraisamy R, Krishnan CS, Ramasubramanian H, et al. Compatibility of nonoriginal abutments with implants: Evaluation of microgap at the implant–abutment interface, with original and nonoriginal abutments. Implant Dent 2019; 28:289-295.
- Varghese SS, Ramesh A, Veeraiyan DN. Blended module-Based teaching in biostatistics and research methodology: A retrospective study with postgraduate dental students. J Dent Educ 2019; 83:445–450.
- Verma M, Mutneja P, Gupta R, et al. Telescopic overdenture for oral rehabilitation of partially edentulous patient. Indian J Dent Res 2019; 30:468–471.
- Ardiansyah M, Dharmautama M. Preventive maintenance prosthodontics telescopic overdenture: A literature review, J Dent Sci 2016; 175.
- Reich KM, Huber CD, Lippnig WR, et al. Atrophy of the residual alveolar ridge following tooth loss in an historical population. Oral Diseases 2011; 17:33-44.
- https://onlinelibrary.wiley.com/doi/full/10.1111/jcpe.546_12915?af=R
- Wical KE, Swoope CC. Studies of residual ridge resorption. Part II. The relationship of dietary calcium and phosphorus to residual ridge resorption. J Prosthet Dent 1974; 32:13-22.
- Al-Noori A, Said G. The effect of soft lining materials on mandibular residual ridge resorption for edentulous patient. Al-Rafidain Dent J 2012; 13:66–71.
- Li Z, Müller R, Ruffoni D. Bone remodeling and mechanobiology around implants: Insights from small animal imaging. J Orthop Res 2018; 36:584-593.
- Harrel SK. Videoscope-Assisted minimally invasive surgery (VMIS) for bone regeneration around teeth and implants: A literature review and technique update. Dent J 2018; 6:30.
- Verma M, Mutneja P, Gupta R, et al. Telescopic overdenture for oral rehabilitation of partially edentulous patient. Indian J Dent Res 2019; 30:468.
- Crum RJ, Rooney Jr GE. Alveolar bone loss in overdentures: a 5-year study. J Prost Dent 1978; 40:610-613.
- Morrow RM, Feldmann EE, Rudd KD, et al. Tooth-supported complete dentures: an approach to preventive prosthodontics. J Prosthetic Dent 1969; 21:513-522.
- Bolouri A. Removable partial denture design for a few remaining natural teeth. J Prosthet Dent 1978; 39:346-348.
- Hakkoum MA, Wazir G. Telescopic denture. Open Dent J 2018; 12:246–254.
- Yee A, Chui Ling G. Aesthetic and occlusal rehabilitation using a telescopic denture. Cureus 2020; 12:e7402.
- Bhagat TV, Walke AN. Telescopic partial dentures-concealed technology. J Int Oral Health 2015; 7:143–147.
- Shimodaira O. A longitudinal observation of a unilateral konus telescopic denture patient. Nihon Hotetsu Shika Gakkai Zasshi 2013; 846–847.
- Suzuki F. A case used dental implant for long-term stabilization of cone crown telescopic denture. Nihon Hotetsu Shika Gakkai Zasshi 2003; 375–376.
- Stančić, I, Jelenković A. Retention of telescopic denture in elderly patients with maximum partially edentulous arch. Gerodontology 2008; 162–167.
- Hamzah MU, Sayed AM, Nassef TM. Computer assisted validation of using newly introduced thermoplastic material in fabrication of a telescopic denture. Int J Computer Applications 2018; 975:8887.
- Modalavalasa HK, Shankar YR, Kumar PS, et al. A novel overdenture telescopic prosthesis. J Orofac Res 2015; 2015:56-60.
Author Info
Sanjana Devi*, Deepak Nallaswamy and Revathi Duraisamy
Department of Prosthodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Science, Saveetha University Tamilnadu, IndiaCitation: Thaer A Mukhlif, Raghad A Al-Hashimi, The Effect of Adding Poloxamer Surfactant on the Penetration Depth of NaOCl and NaOH into Dentinal Tubules, J Res Med Dent Sci, 2021, 9 (1): 210-214.
Received: 23-Sep-2020 Accepted: 23-Dec-2020
