Research - (2021) Volume 9, Issue 11
Network Analysis of Posttraumatic Growth and Posttraumatic Stress Symptomatology in Covid-19 Infected Peruvian Adults
Cristian Ramos-Vera1,2* and Antonio Serpa Barrientos1,2,3
*Correspondence: Cristian Ramos-Vera, Peru, Email:
Abstract
The aim was to estimate the network analysis between indicators of stress and posttraumatic growth in Peruvian adults infected with COVID-19. A total of 456 Peruvian adults were studied, and two self-report health measures were applied in Spanish: Impact of event scale-6 (IES-6) and Posttraumatic Growth Inventory- Short Form (PTGI-SF). The research was quantitative and correlational in nature, evaluated by means of a Gaussian graphical model of partial correlations and the stability of network relationships were verified by Bootstraping. The most central negative posttraumatic symptoms were between intrusive thoughts and avoidance of intrusive thoughts by COVID-19 (E3 and E5). In the PTGI-SF domain, measures of higher centrality were reported for appreciation for life and religious faith (C2 and C9). The reagent associated with life appreciation (C2) plays the role of intermediary between the connecting pathways of the other core elements in the activation of the network system. The highest relationship was found between the hyper vigilance reagents and concentration problems by COVID-19 (E2 and E6). There were four positive relationships and five negative associations between stress symptoms and posttraumatic growth, the largest effect sizes included the core symptom of avoidance of intrusive thoughts with appreciation for life directly and inverse or negative relationship with spiritual growth.
Keywords
Post-traumatic growth, Post-traumatic stress, COVID-19, Network analysis, Mental health
Introduction
During these pandemic times there is an increased tendency for negative impact on mental health. In particular, many individuals exhibit depressive symptoms, related to stress and anxiety in response to viral outbreaks and measures of social isolation [1]. Direct and indirect exposure to COVID-19 has generated feelings of threat linked to increased symptomatologic comorbidity of psychological distress, anxiety, and fear [2,3].
Because of the nature of pandemic threat, models of posttraumatic stress disorder (PTSD) or posttraumatic symptoms (PS) seem relevant in the current pandemic context. The World Health Organization (WHO) refers to PTSD as a disorder that develops "after exposure to an extremely threatening or horrific event or series of events." Which considers that the exposure to the COVID-19 pandemic and its associated consequences refer to a valid potentially traumatic event described by the International Classification of Diseases [4]. Given the persistence of the event since the early 2020s as a latent threat, coupled with the effects of virus mitigation measures have confirmed SP in COVID-19 infected adults [5,6].
However, some individuals exposed to adversity report positive changes as a result of their experiences. Such changes are characterized by a greater appreciation of life, the perception of new opportunities, a greater sense of personal strength, improved relationships with people, and increased religiosity or spirituality. This positive transformation is known as posttraumatic growth (PG) [7,8].
The processes underlying the development of PG emerge in the same way as the negative effects. These are largely represented in existing models of psychological growth, most notably the transformational model of Tedeschi & Calhoun [7]. This model proposes cognitions related to such events and their coping responses, as well as social support, which are essential in PG outcomes. Adverse events are generally experienced as traumatic if they are seismic enough to shatter world assumptions and preexisting schemas. A period of rumination usually follows, in which attempts are made to reconcile worldviews with new information related to the trauma to accommodate existing knowledge. This does not imply that PG occurs in the absence of negative affect, as people exposed to adversity generally report concurrent negative symptoms, such as SPs. These negative symptoms appear to be part of the emotional struggle in which PG may occur [9].
The PS included in this study refers to 3 groups according to the American Psychiatric Association validated by Thoresen et al. [10]: Intrusion, avoidance, and hyperactivity. Intrusion symptoms reflect a reexperiencing of the traumatic event (e.g., intrusive memories, flashbacks, nightmares). Avoidance symptoms are manifested by avoidance of stimuli associated with the event (e.g., avoidance of thoughts or feelings and reminders related to the trauma). And, hyperarousal symptoms reflect increased reactivity to stimuli (e.g., Irritability).
The processing period of adverse events is generally reflected in increased stressful PS, marked by intrusive thoughts and flashbacks of the event [11]. Findings suggest that PTSD cognitions show linear and curvilinear positive relationships with PG [12,13]. Specifically, lower self-report of PS refers to lower perceived distress from the adverse event and, in turn, lower experience of PG. Moderate levels of PTSD symptomatology refer that the person's world has been challenged in some way, yet may be involved in the cognitive processing necessary for the PG to occur. Higher levels of negative SP tend to overwhelm the individual's coping resources being more likely to succumb to negative effects of PTSD, with minimal experience of PG [11].
Thus, although seemingly incompatible, the components of PG and PTSD often overlap. Concurrence of both has been reported in a variety of traumatic events [12,13]. Indeed, many individuals have experienced growth simultaneously with considerable levels of TEPT symptoms during the COVID-19 pandemic [14,15]. Research on the relationship between PTSD-PG measures has been focused on identifying general relationships between both constructs in specific traumatic events. However, there is little research on how these variables are maintained among them, therefore, it is necessary to know the global dynamics of positive and negative PS in order to know the protective characteristics of psychological well-being and those of greater vulnerability to traumatic impact by COVID-19.
After a brief review of the scientific literature, no Latin American network study was found to date that includes COVID-19 infection as a traumatic event, and it is necessary to explore how the higher risk symptoms of PTSD and the elements of PG are maintained and mutually reinforcing. Therefore, we aimed to evaluate the correlation networks of the items of these variables.
Methods
Participants
Quantitative study of exploratory, correlational, crosssectional type, developed in the Metropolitan city of Lima, Peru, composed of 456 Peruvian adults from the city of Lima (59.53% women; M age: 25.40, SD=2.08), due to restrictive government measures of distancing and social mobility, the application of online survey methodology was considered. Participants were recruited using a snowball sampling technique through social networks such as Whats App groups, Facebook and Google groups and were encouraged to invite their family and friends to participate in the survey. It was developed and administered using Google forms, likewise, informed consent was included for all participants included in the study. The data were collected during the last two months of 2020 targeting an audience over 18 years of age. Sampling requirements were met given the a priori power analysis with the consideration of anticipating a median effect size of 0.10 considered to be a moderate effect on partial network relationships [16], with a power level set at 0.95 and a significant alpha of 0.05. The minimum required size needed to detect a significant effect was 328 participants for the proposed model of psychological networks [17].
Instruments
The following instruments were considered in the Spanish versions: Impact of event scale-6 (IES-6) composed of six symptoms of increased risk for posttraumatic stress disorder [10] with Likert responses from 1 to 4, and Posttraumatic Growth Inventory- Short Form (PTGI-SF) composed of 10 items [18] for the measurement of PG with a Likert scaling of six-choice response. The alpha and omega reliability of the instruments were estimated, with values greater than 0.85. A demographic data questionnaire was also considered. The first question of the questionnaire consisted of reporting whether they had a positive diagnosis by COVID-19 and its consideration as a traumatic event; the other questions covered sociodemographic variables such as age, sex, place of residence and mental health status.
Statistical analysis
The R package qgrap and the LASSO graph (recommended fit parameter of γ=.50) were used to graphically represent the patterns of connections representing the partial correlations in the network system; the LASSO estimator allows spurious relationships to be eliminated [19,20]. The items (nodes) are interconnected by lines or edges representing the partial correlations that tend to be located in the network according to the sum of connections with other nodes [21]. Red edges represent negative relationships and blue edges represent positive relationships. The expected influence index was included since it is the most stable measure for determining the importance of components in positive and negative correlations [22] reported in network antecedents by Yuan et al. [23] and Peters et al. [24]. More central elements refer greater network connections and favor direct and indirect relationships of the other components in the dynamic system structure. The robustness of the accuracy of the edge weights was evaluated using the Bootstrapping method based on 5000 samples to calculate 95% Confidence Intervals (CI) from a nonparametric approach [19].
Results
Table 1 collects the descriptive statistics of the participants' responses for the measures used. These data indicate higher reporting of IES-6 items E5 and E3, and PTGI-SF items C9 and C2, which in turn reported the highest measures of expected network influence.
| IES-6 | ME | EI |
|---|---|---|
| E1. | 2.98 | 0.78 |
| E2. | 2.93 | 1.26 |
| E3. | 3.04 | 0.72 |
| E4. | 2.15 | 0.75 |
| E5. | 3.18 | 1.33 |
| E6. | 2.89 | 0.79 |
| PTGI-SF | ME | IE |
| C1. | 3.74 | 0.85 |
| C2. | 3.98 | 1.18 |
| C3. | 3.82 | 0.91 |
| C4. | 2.68 | 0.81 |
| C5. | 3.54 | 0.43 |
| C6. | 3.8 | 0.69 |
| C7. | 3.29 | 0.95 |
| C8. | 2.86 | 0.67 |
| C9. | 4.47 | 1.26 |
| C10. | 3.05 | 0.99 |
| Note: ME=mean, EI=expected influence index | ||
Table 1: Mean of the items and measures of expected influence.
The results of Figure 1 show higher network connections (correlations) in the PC domain in items C7 and C8 (partial r=0.31), C2 and C9 (partial r=0.29), C5 and C6 (partial r=0.28), which refers to a higher interactive prevalence between such network elements and presents item C9 linked to personal mental strength as one of the most central in the network (1.26), item C2 reports a higher number of connections.
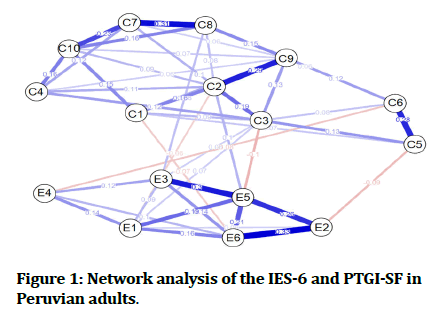
Figure 1: Network analysis of the IES-6 and PTGI-SF in Peruvian adults.
Likewise, high measures of association are highlighted in the IES-6 symptoms: E2 and E6 (partial r=0.33), E3 and E5 (partial r=0.30), E2 and E5 (partial r=0.26), item E5 referred to the avoidance of intrusive thoughts by COVID-19 reports greater network centrality (1.33). In turn, this item stands out in the interdomain connections (IES6-PTGI) with a greater association with the C2 and C3 items.
Standing out with more interdomain relationships (3) was the spiritual growth item (C3). Other reported connections were between items C2 and E1, C5 and E2, C6 and E4 whose correlation effect sizes are between -0.09 and 0.08 values.
The precision of the edge weights is shown in Figure 2, where the red line indicates the sample edge weight (with increasing order from highest negative to highest positive ratio) and the gray bars are the 95% CIs using the bootstrapping method. There is evidence of positive and negative estimated edges, which mostly did not overlap with other edges, which refers to an accurate estimation.
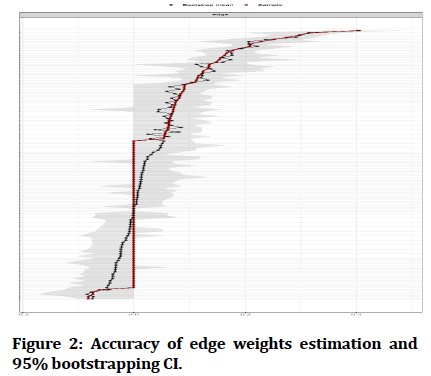
Figure 2: Accuracy of edge weights estimation and 95% bootstrapping CI.
Discussion
Network results seek to provide further information on how PTSD and PG symptom measures are reinforced during COVID-19, since in addition to higher reported levels of stress symptomatology, high values of PG are also evident during the pandemic event [14,15,25], and such studies report relationships between both concepts during COVID-19. Therefore, it is important to evaluate the simultaneous relationships between the components of such psychological measures using network analysis, to our knowledge this is the first study to include this dynamic method given the stressful event of COVID-19 infection. Although mostly network studies have focused on assessing negative PS linked to PTSD as referred by a previous systematic network study [26], while studies with this dynamic methodology including the measure of PG are scarce [23,24,27].
The present study reported a higher expected influence index in item E5. This core component reinforces the other interactions in the network, i.e., the intrusive thought avoidance measure by COVID-19 together with the hypervigilance measure reinforcing the activation of the other PS by COVID-19 of IES-6 and anchoring the relationships with the PG domain in the network structure. Such a finding is in agreement with the positive and negative PS network study by Peters et al. [24] in a sample of Chinese earthquake-affected adults, who reported a higher centrality on the thought avoidance measure. Thus, also the authors indicated the relevance of two other symptoms linked to PTSD that were not included in the current study such as physiological cue reactivity and reckless behavior. While the PG measures presented low centrality values, such variations may be due to the different traumatic event and that the event in question happened more than a decade ago (2008).
The research by Yuan et al. [23] in a sample of Chinese university students affected by a natural disaster (grade 3 typhoon), highlighted the higher centrality of PG measures compared to PTSD symptoms in the network, especially reported higher centrality in the components of global vital appraisal. In our study, the core items of appreciation for each day and greater appreciation for others were not considered, with the most important positive PS being appreciation for life (C2) and personal strength (C9) in the face of COVID-19 infection. Another central component was the symptom of hypervigilance (E2), which was also evidenced in the study of Yuan et al. [23], who also reported high centrality indices in the negative PS related to difficulty concentrating (E6). Both negative PS are of higher covariance of the IES-6 domain in the present network and present relationships with the central reagent (E5) of higher effect size.
The most central measure of the network is positively related to the element of appreciation for life (C2) and negatively related to spiritual growth (C3). This suggests that avoidance of intrusive thoughts directly reduces spiritual growth in the face of the COVID-19 infection event, since further spiritual growth requires acceptance of such negative thoughts [23]. However, in the short term this symptom avoidance favors the reduction of stressful impact, and reinforces a greater appreciation of life and personal priorities such as family and better use of time in pleasurable activities, which is more closely related to the core element of PG (C9).
It is possible to identify a network pathway of interest consisting of five variables that include the highest relationships of both network domains (E5-E3-C8-C7- C2), whose feedback from such indicators provides additional information on how PTSD and PG measures are positively reinforced [12,13]. This dynamic pathway refers that avoidance of intrusive thoughts may generate a paradoxical effect of increased level of rumination or repetitive obsessive thoughts that relate to religious faith [28]. People who have had these experiences may perceive negative or adverse situations as transformative given that religious faith reinforces the creation of deep meaning of the event, which enables the development of new positive coping skills related to greater adjustment and positive reappraisal [7,9].
The PG process is composed of negative and positive cognitions based on the traumatic event (COVID-19), this refers to a new belief system where people can identify themselves as vulnerable, but stronger, i.e., they simultaneously feel less immune to life's adversities, but with the strength to face it, which strengthens the coping capacity for the emergence of psychological growth [29,30]. The interpretation of network models favors the systemic representation of such a manifestation since it allows a system where positive and negative PS coexist.
The negative relationships of life appreciation symptoms with stressful symptoms (C1 and E6; C2 and E5) provide information on the most essential components linked to psychological growth, and the findings of Yuan et al. [23] also point out that life appreciation is essential in the reduction of PTSD symptoms. Such a measure of PG should be promoted along with other associated variables such as meaning, hope, and life satisfaction that evidence the reduction of the effect of negative PS by COVID-19 [31-33]. The network results also suggest reduced avoidance of intrusive thoughts that in the long term produce more severe symptoms of psychological distress and chronic stress. This is of further interest given that other previous network findings reflect greater associations between avoidant symptoms of PTSD [23,24].
The network results obtained show interactions not only at the level of items in the same domain but also between domains of two clinical variables of a traumatic nature in the current pandemic context. Network models are applicable beyond psychological measures, for example, they have been applied to other areas of health sciences and in groups with various chronic conditions [34-38]. It is possible to explore new clinical hypotheses such as the comprehensive and simultaneous assessment of various health conditions comorbid with the COVID-19 pandemic [39,40], which is not possible with bivariate analyses. It is also useful for analyzing the systemic relationship of various protective and risk factors to physical and mental health [41-43].
Given the traumatic impact of the pandemic, it is required to evaluate network models that report the interconnections of PS with other clinical variables of major interest such as COVID-19 preventive health behavior [2], burnout [14], eating disorders [6,44], depression and anxiety [45], sleep disorders [46], Internet gaming disorder symptoms [47], in addition to obsession, threat, and fear symptomatology by COVID-19 [39,40,48] to implement a transdiagnostic approach to mental health assessment and treatment in the face of psychological responses consequent to the potentially traumatic event of the current pandemic [49]. While other network results are of great interest to this journal as they include measures associated with oral health [50-53] that require further diffusion in diverse cultural contexts beyond Latin America.
In the present study, participants did not present diverse traumatic events, therefore, future studies should consider correlation network models in participants with varied stressful events and other populations with diverse sociodemographic characteristics, also longitudinal data should be included to estimate directed networks that are more accurate in assessing causality patterns in the items evaluated. It should be considered that this is a cross-sectional study, and does not allow inferring whether a given node causes or is caused by another node to which it is connected, due to the use of undirected networks. It is important to replicate these network findings in other Latin American groups to generalize the results obtained.
Another limitation is that the cross-sectional edges represent both within- and between-subject effects that cannot be disentangled, i.e., it is not possible for such results to be interpreted at the individual level. Experimental and prospective designs are needed that favor a more rigorous evaluation of the underlying assumptions in causal systems models in psychological research that consider diverse measures of analysis and diagnosis.
In conclusion, this study is the first to apply network analysis to examine patterns of relationships between positive and negative posttraumatic indicators considering the COVID-19 virus infection event. The most central measures in this network are C9, C2, E2 and E5. The reagent associated with life appreciation (C2) plays a fundamental intermediary role in the interconnection of the other core elements. The intrusive thought avoidance symptom by COVID-19 (E5) reported the highest relationships between the positive and negative PS domains.
References
- Hawryluck L, Gold WL, Robinson S, et al. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis 2004; 10:1206-1212.
- Olapegba PO, Chovwen CO, Ayandele O, et al. Fear of COVID-19 and preventive health behavior: mediating role of post-traumatic stress symptomology and psychological distress. Int J Ment Health Addict 2021; 1-12.
- Ayandele O, Ramos-Vera CA, Iorfa SK, et al. Exploring the complex pathways between the fear of COVID-19 and preventive health behavior among Nigerians: Mediation and moderation analyses. Am J Trop Med Hyg 2021; 105:701-707.
- https://www.who.int/standards/classifications/classification-of-diseases
- Xiao S, Luo D, Xiao Y. Survivors of COVID-19 are at high risk of posttraumatic stress disorder. Glob Health Res Policy 2020; 5:29.
- Ramos-Vera CA. Red de síntomas psicopatológicos de la conducta alimentaria, depresión, ansiedad y estrés postraumático en adultos peruanos en cuarentena por COVID-19. Rev Cuba Enferm 2020; 36:e4200.
- Tedeschi RG, Calhoun LG. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychol Inquiry 2004; 15:1-18.
- Ramos-Vera C. Crecimiento postraumático durante la pandemia de COVID-19. Curr Opin Nurs Res 2021; 1:1-3.
- Lancaster SL, Klein KR, Nadia C, et al. An integrated model of posttraumatic stress and growth. J Trauma Dissociation 2015; 16:399-418.
- Thoresen S, Tambs K, Hussain A, et al. Brief measure of posttraumatic stress reactions: Impact of Event Scale-6. Soc Psychiatry Psychiatr Epidemiol 2010; 45:405-412.
- Joseph S, Murphy D, Regel S. An affective-cognitive processing model of post-traumatic growth. Clin Psychol Psychother 2012; 19:316-325.
- Liu AN, Wang LL, Li HP, et al. Correlation between posttraumatic growth and posttraumatic stress disorder symptoms based on pearson correlation coefficient: A meta-analysis. J Nerv Ment Dis 2017; 205:380-389.
- Shakespeare-Finch J, Lurie-Beck J. A meta-analytic clarification of the relationship between posttraumatic growth and symptoms of posttraumatic distress disorder. J Anxiety Disord 2014; 28:223-229.
- Chen R, Sun C, Chen JJ, et al. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 Pandemic. Int J Ment Health Nurs 2021; 30:102-116.
- Hamam AA, Milo S, Mor I, et al. Peritraumatic reactions during the COVID-19 pandemic: The contribution of posttraumatic growth attributed to prior trauma. J Psychiatr Res 2021; 132:23-31.
- https://f1000research.com/articles/10-19/v2
- Ramos-Vera CA. Beyond sample size estimation in clinical univariate analysis. An online calculator for structural equation modeling and network analysis on latent and observable variables. Nutr Hosp 2021.
- García FE, Wlodarczyk A. Psychometric properties of the posttraumatic growth inventory–short form among Chilean adults. J Loss Trauma 2016; 21:303-314.
- Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol Methods 2018; 23:617-634.
- Ramos-Vera C. Statistical relationship networks in psychiatric research: The case of delirium in the context of COVID-19. Rev Colomb Psiquiatr 2021; 50:158-159.
- Ramos-Vera C, Serpa A. Network analysis in psychiatric research. Actas Esp Psiquiatr 2021; 49:123-124.
- Bringmann LF, Elmer T, Epskamp S, et al. What do centrality measures measure in psychological networks? J Abnorm Psychol 2019; 128:892-903.
- Yuan G, Park CL, Birkeland SR, et al. A network analysis of the associations between posttraumatic stress symptoms and posttraumatic growth among disaster-exposed chinese young adults. J Trauma Stress 2021; 34:786-798.
- Peters J, Bellet BW, Jones PJ, et al. Posttraumatic stress or posttraumatic growth? Using network analysis to explore the relationships between coping styles and trauma outcomes. J Anxiety Disord 2021; 78:102359.
- Zhen R, Zhou X. Latent patterns of posttraumatic stress symptoms, depression, and posttraumatic growth among adolescents during the COVID-19 Pandemic. J Trauma Stress 2021.
- Birkeland MS, Greene T, Spiller TR. The network approach to posttraumatic stress disorder: A systematic review. Eur J Psychotraumatol 2020; 11: 1700614.
- Ramos-Vera C, Ramírez Y, Rojas E, et al. Evidencias psicométricas mediante SEM y análisis de red del Inventario de Crecimiento Postraumático en adolescentes peruanos. Psi Cond 2020; 29.
- Himle JA, Chatters LM, Taylor RJ, et al. The relationship between obsessive-compulsive disorder and religious faith: Clinical characteristics and implications for treatment. Psychol Religion Spirit 2011; 3:241-258.
- Jayawickreme E, Infurna FJ, Alajak K, et al. Post-traumatic as growth as positive personality change: Challenges, opportunities, and recommendations. J Pers 2021; 89:145-65.
- Olson K, Shanafelt T, Southwick S. Pandemic-driven posttraumatic growth for organizations and individuals. JAMA 2020; 324:1829-30.
- Robles-Bello MA, Sánchez-Teruel D, Valencia Naranjo N. Variables protecting mental health in the Spanish population affected by the COVID-19 pandemic. Curr Psychol 2020; 1-12.
- Trzebinski J, Cabanski M, Czarnecka JZ. Reaction to the COVID-19 pandemic: The influence of meaning in life, life satisfaction, and assumptions on world orderliness and positivity. J Loss Trauma 2020; 25:544-557.
- Prieto-Ursúa M, Jódar R. Finding meaning in hell. The role of meaning, religiosity and spirituality in posttraumatic growth during the coronavirus crisis in Spain. Front Psychol 2020; 11: e567836.
- Henneghan A, Wright ML, Bourne G, et al. A cross-sectional exploration of cytokine-symptom networks in breast cancer survivors using network analysis. Can J Nurs Res 2020; 844562120927535.
- de Rooij BH, Oerlemans S, van Deun K, et al. Symptom clusters in 1330 survivors of 7 cancer types from the PROFILES registry: A network analysis. Cancer 2021.
- Zhu Z, Hu Y, Xing W, et al. Identifying symptom clusters among people living with HIV on antiretroviral therapy in China: A network analysis. J Pain Symptom Manage 2019; 57:617-626.
- Zhu Z, Wen H, Yang Z, et al. Evolving symptom networks in relation to HIV-positive duration among people living with HIV: A network analysis. Int J Infect Dis 2021; 108:503-509.
- Rha SY, Lee J. Stable symptom clusters and evolving symptom networks in relation to chemotherapy cycles. J Pain Symptom Manage. 2021; 61:544-554.
- Ramos-Vera C. Network relationships of the stigma-discrimination complex and fear of COVID-19 during the second pandemic wave in Peruvian adults. Rev Colomb Psiquiatr 2021.
- Ramos-Vera C. The dynamic network relationships of obsession and death from COVID-19 anxiety among Peruvian university students during the second quarantine. Rev Colomb Psiquiatr 2021; 50:160-163.
- Taylor S, Paluszek MM, Rachor GS, et al. Substance use and abuse, COVID-19-related distress, and disregard for social distancing: A network analysis. Addict Behav 2021; 114:e106754.
- Shim EJ, Ha H, Suh YS, et al. Network analyses of associations between cancer-related physical and psychological symptoms and quality of life in gastric cancer patients. Psychooncol 2021; 30:946-953.
- Penzel N, Antonucci LA, Betz LT, et al. Association between age of cannabis initiation and gray matter covariance networks in recent onset psychosis. Neuropsychopharmacol 2021; 46:1484-1493.
- Liebman RE, Becker KR, Smith KE, et al. Network analysis of posttraumatic stress and eating disorder symptoms in a community sample of adults exposed to childhood abuse. J Trauma Stress 2021; 34:665-674.
- Price M, Legrand AC, Brier ZMF, et al. The symptoms at the center: Examining the comorbidity of posttraumatic stress disorder, generalized anxiety disorder, and depression with network analysis. J Psychiatr Res 2019; 109:52-58.
- Wang S, Sit HF, Garabiles MR, et al. A network analysis investigation of the comorbidity between sleep dysfunction and PTSD symptomatology among Filipino domestic workers in Macao (SAR) China. J Psychiatr Res 2021; 140:337-345.
- Yuan GF, Shi W, Elhai JD, et al. Gaming to cope: Applying network analysis to understand the relationship between posttraumatic stress symptoms and internet gaming disorder symptoms among disaster-exposed Chinese young adults. Addict Behav 2021; 124: e107096.
- Ramos-Vera C. Estructura de red del impacto y la percepción de amenaza de la COVID-19. Rev cuba enferm. 2020; 36: e4136.
- Williamson RE, Hoeboer CM, Primasari I, et al. Symptom networks of COVID-19-related versus other potentially traumatic events in a global sample. J Anxiety Disord 2021; 84:102476.
- Baek JJH, Soares GH, da Rosa GC, et al. Network analysis and psychometric properties of the Brazilian version of the eHealth Literacy Scale in a dental clinic setting. Int J Med Inform 2021; 153: e104532.
- Soares GH, Santiago PH, Biazevic MGH, et al. Dynamics in oral health-related factors of Indigenous Australian children: A network analysis of a randomized controlled trial. Community Dent Oral Epidemiol 2021.
- Soares GH, Santiago PHR, Biazevic MGH, et al. Do network centrality measures predict dental outcomes of Indigenous children over time? Int J Paediatr Dent 2021; 31:634-646.
- Soares GH, Santiago PHR, Michel-Crosato E, et al. The utility of network analysis in the context of Indigenous Australian oral health literacy. PLoS One 2020; 15:e0233972.
Author Info
Cristian Ramos-Vera1,2* and Antonio Serpa Barrientos1,2,3
1Universidad Cesar Vallejo, Lima, Peru2Sociedad Peruana de Psicometría, Lima, Peru
3Universidad Nacional Mayor de San Marcos, Lima, Peru
Citation: Cristian Ramos-Vera, Antonio Serpa Barrientos, Network Analysis of Posttraumatic Growth and Posttraumatic Stress Symptomatology in Covid-19 Infected Peruvian Adults, J Res Med Dent Sci, 2021, 9(11): 61-67
Received: 28-Sep-2021 Accepted: 22-Oct-2021
