Review - (2023) Volume 11, Issue 2
Narrative Review Article: Prophylactic and Therapeutic Role of Different Routes of Vitamin C and Zinc against SARS CoV2 Virus
Sushma Selvanathan1 and Pramita A Muntode2
Abstract
The repercussion of SARS CoV2 virus pandemic has been detrimental on economic, social and medical grounds. To combat the disease, policies like maintaining social distance, self-quarantine- voluntarily or by compulsion at home have reduced the rate of spread of disease. The various drugs used in management of these patients are still under study regarding their effectiveness and side effects. Also, the vaccines that are licensed for use in various countries their safety and efficacy in long run is still unknown. With the understanding that the immune mediators and oxidative stressors play a pivot role in pathogenesis of SARS CoV2 virus, a breach in immunity can therefore predispose to severe infections. Majority of population in India suffers from various forms of micronutrient deficiencies. Combating the disease requires strengthening the basic nutritional status of the country. A balanced diet and nutrition are crucial for an optimum immunological response. In this narrative review, mainly focuses on the micronutrient vitamin C and zinc and their role in immune system. With vitamin C and zinc supplements used as an age old remedy for viral respiratory illness like common cold and pneumonia, studies have now focused on their use against SARS CoV 2 virus. This review also focuses on the impact of their deficiencies in COVID-19 patients and their prophylactic and therapeutic use in their various routes of administration against SARS CoV-2 virus are taken into account, which give a holistic approach towards this review.
Keywords
COVID 19, SARS CoV2 virus, Ascorbic acid, Ionophores, Cytokine storm
Introduction
From the first case detected of SARS CoV-2 on 30th January 2020, India is currently in the midst of the second wave; with the number of cases more than double that of the first wave. The consequence of COVID 19 has been detrimental on economical, medical and social grounds. SARS CoV2 viruses a lipid bi-layered single stranded RNA virus from severe acute respiratory syndrome Coronavirus family. A rapid transmission from one person to another is by aerosol route (droplets) [1]. SARSCoV- 2 symptoms can vary from latent asymptomatic to fulminant form, including cough, pyrexia, and shortness of breath. Severe acute respiratory failure, acute cardiac problems, systemic inflammatory response syndrome, multiple organ dysfunction syndromes, septic shock, and death are all possible outcomes in more severe cases [2,3].
Oxidative stress and inflammatory processes have a big influence on the immune system [4]. Coronavirus leads to increased synthesis and secretion of Interleukin-1, Interleukin-4, Interleukin-10, monocyte chemoattractant protein 1 (MCP-1), interferon gamma and Interferon gamma induced protein-10 [5]. In addition, human bronchial epithelial cells produce multiple NF-Bmediated cytokines which is triggered by SARS CoV infection, including Interleukin-6 and Interleukin-8 [6]. Patient in intensive care unit with severe infection shows cytokine storm which leads to excessive inflammatory reaction and can be life threatening [7].
The emergence of this new infectious disease has been moving at a breakneck pace. To combat the disease, strict governmental regulations have been enacted, including interpersonal distancing policies in public places and policies motivating or even compelling people to be home quarantined. Based on our present knowledge on pathogenesis, many vaccines and currently used drugs are under trial with no promising results. Individuals are usually at a loss considering the variation in food patterns and need to maintain optimum nutrient status in order to stay healthy, especially during this selfcontainment. Therefore, a strong, functional immune system is essential for prevention of infection, and an adequate and balanced diet is a vital platform for an effective immunological response [8].
Along with balanced diet, patients receiving various drug regimens, have vitamin C and zinc tablets as a constant. The age old use of vitamin C and zinc for common cold as anti-oxidant and immune modulators have emerged as basic treatment for COVID-19 patients. With the lack of understanding on how the prophylactic action of vitamin C and zinc in common cold and COVID-19 infection differs, this narrative review helps as understand the immune basis of vitamin C and zinc against COVID-19.
Methodology
A search was made on 1st June, 2021 on online portals PUBMED, GOOGLE SCHOLAR using search terms like: “COVID-19”and “IMMUNE SYSTEM” and “VITAMIN C AND ZINC” and /or “PROPHYLAXIS”. The articles from 2020-2021 were accessed and analyzed.
Discussion
Immune system, Covid-19 and immune response
Our immune system can be classified into two main types: (a) innate immunity (present since birth) which is a faster in action and non-specific and (b) adaptive immunity (formed during growth) which is delayed response and antigen specific. The innate immunity which consist of physical barrier like skin, gastrointestinal system along with complement system and phagocytes respond quickly to pathogen via nonspecific pattern-recognition receptors, inflammatory processes and thereby reduce inflammation and repair the damage done by the pathogen. But, if our body is exposed to same pathogen, innate immunity lacks the efficiency to clear the pathogen faster. On the other hand, adaptive responses which mainly comprise of lymphocytes are targeted towards specific antigen. The Th4 and Th8 lymphocytes kill the cell which contains the antigens directly and the B lymphocytes secrete antibodies specific against the pathogen. By its virtue of generating memory cells, adaptive immunity can respond in quicker and antigen specific manner when recurrence of infection by same pathogen occurs [9].
The immune system can also be considered as coupling of inflammatory response activation and generation of oxidative stress. Oxidative stress occurs when there is an un-equity between oxidative compounds like reactive oxygen species, reactive nitrogen species and antioxidants which could be endogenous like albumin, urea, reduced glutathione, superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx) and exogenous like vitamin E, vitamin C, carotenoids. The oxidative stress results in endothelial injury and inflammation which is evident in COVID- 19 patients [10]. The inflammatory processed through the innate and adaptive immunity acts like an effect viral barrier by preventing viral replication and its spread, reducing inflammation and repair the damage caused by the virus. In this series of events, an undue production of pro-inflammatory cytokines like Interleukin-1β, Interleukin-4, Interleukin-10, interferon gamma (IFN-γ),monocyte chemoattractant protein 1 (MCP-1) and Interferon gamma induced protein -10, along with macrophages and neutrophils can be triggered by tissue injury. This leads to cytokine storm. The condition is termed as secondary hemophagocytic lymphohistiocytosis (sHLH) or macrophage activation syndrome (MAS), which causes further tissue injury [11]. And also most COVID-19 patients, especially those with severe cases, show substantial lymphopenia, which indicates an immune system deficiency. As a result, neutrophils and leukocytes, rather than lymphocytes, appear to strengthen the cytokine storm inSARS CoV2 virus infection. The cytokine storm is coupled with increased mortality due to acute respiratory distress syndrome and respiratory failure. According to certain studies, the CD+4:CD+8 T cell ratio in SARS-CoV-2 infection is comparable to that in the healthy group, and that a rise in this ratio, as well as a drop in CD+8 T cells and B cells, is a poor predictor for post-treatment clinical follow-up.
The immune system is also under physiological control mainly hormonal and metabolic [12,13]. Malnutrition has increased the risk of infection by impairing the immune response and repair processes. Many randomized controlled trials have shown evidence of reduction of viral risk and symptoms with proper balanced diet and nutritional supplement [14]. Therefore, adopting proper diet and nutritional supplements can boost immune system, prevent infection and promote overall health of an individual (Figure 1).
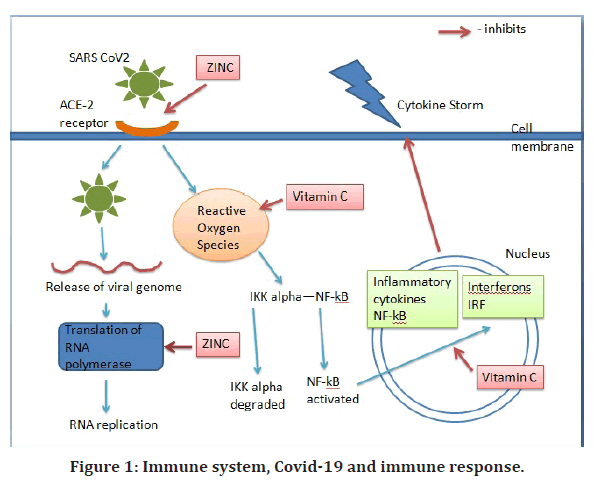
Figure 1. Immune system, Covid-19 and immune response.
Vitamin C, immune response and Covid-19
An age old use of Vitamin C against common cold and other respiratory tract infections have been applied as basis of potential therapeutic use against covid 19 infection [15].
Vitamin C which is a potent exogenous antioxidant, is involved in the redox reaction wherein they reduced free radical in the aqueous layer while get oxidized to dehydro-ascorbic acid [16]. Its immune modulating effect is depicted through various biological synthetic and gene modulatory processes like monooxygenase and dioxygenase enzymes which use vitamin C as their cofactor [17]. In vitro and preclinical studies have demonstrated that vitamin C have a role in lipid synthesis via signaling and biochemical pathways which leads to barrier strengthening function. It is shown to enhance immune response by enhancing chemoattractant of neutrophils, increasing phagocytosis and synthesis of reactive oxygen species. Vitamin C also plays a vital part in wound repair by proliferation and migration of dermal fibroblast via altering gene expression [18]. It has been shown inverse relation between quantity of ascorbic acid intake and the levels of C reactive proteins and tissue plasminogen activator.
Studies have depicted that to maintain normal plasma concentration in healthy subjects, a minimum quantity of 0.1 g/day should be consumed. On the other hand, higher dosages of at least 1 to 3 g/ day have to be consumed by patients in intensive care unit to maintain plasma level [19]. A study has shown that the role of vitamin C in aiding the treatment of sepsis and acute respiratory distress syndrome patients has been insignificant on the account of improving vascular injuries, organ dysfunction and inflammation. But they do show a significant effect on decreasing mortality rates [20]. Deficiency of vitamin C is quite prevalent among patients infected with SARS CoV-2 virus [21]. The immune response that leads to the lung pathology caused by SARS CoV2 virus is the formation of micro thrombi and coagulopathy. SARS-CoV-2 suppresses the production of interferon- 1, but vitamin C increases the expression of these important host defense proteins [22]. Studies have shown that prompt treatment with intravenous vitamin C, deteriorates the above process, by inhibiting the expression of p-selectin on the endothelial surface and thereby inhibiting platelet endothelial cell adhesion [23]. A case series was conducted by Hiedra R et al., evaluating use of vitamin C via intravenous route in COVID-19 patients have shown reduction in the levels of D- dimer in their course of hospital stay [24].
Many clinical trials have been undertaken to examine the advantages of intravenous vitamin C in COVID 19 patients. The pioneer among these trials is ‘Intravenous highdose vitamin C for the treatment of severe COVID-19: study protocol for a multicenter randomized controlled trial. organized in Wuhan, China. In this trial, Liu, et al. treated 56 patients with vitamin C via intravenous route at a dose of 12g/12 h for a week. The intravenous administration of such a large concentration of vitamin C enhanced arterial oxygenation, most likely due to better pulmonary ventilation- perfusion performance, reduced the 28-day mortality rate(P=0.06), and in the same trial, decreased the levels of interleukin-6 (IL-6) (P=0.04) in comparison to the control group by day 7 of infusion [25]. Additional clinical trials have been conducted in various countries (United States, Canada, china), will further investigate whether intravenous vitamin C would provide a cost-effective yet not compromising on the safety of treatment against C. On the other hand, vitamin C has not proven beneficial in decreasing epithelial damage of alveoli in a randomized control study compared to controls, in patients suffering from sepsis and severe acute respiratory distress syndrome [26].
As a result, preliminary trials and studies suggest that vitamin C levels and vitamin C therapeutic supplementation may influence the clinical spectrum of COVID-19. But majority of these clinical trials investigates the benefits and effects of intravenous infusions of vitamin C in patients admitted in intensive care unit. With randomized control trial with large subjects and high funding such as LOVIT-COVID, the usage of intravenous vitamin C against tissue damage done by SARS CoV-2 virus will provide evidences with greater significance. There are no trials studying the prophylactic usage of vitamin C in intravenous and oral route to healthy individuals or to asymptomatic or mild cases of COVID-19.
Zinc, immune response and Covid-19
Zinc is a basic trace element obtained through balanced diet containing lentils, legumes, nuts, black rice, lamb, chicken, and oyster or through supplementation. They are usually present at low intracellular concentration in plasma with normal dietary recommendation range of 8-11mg/dl [27].
Zinc as a macronutrient is important for the growth and development of cells in both the innate and adaptive immune systems. Studies have shown zinc to play an important role in maintenance of skin and mucosal membrane integrity [28]. In case of adaptive immunity, zinc is important for immune cellular growth and differentiation, helps in signaling release of cytokine and triggers multiplication of CD8+ T-cells [29]. Zinc is important for proliferation of T lymphocytes via intracellular binding of tyrosine kinase to T- cell receptors. Zinc acts as cofactor for several enzymes acting as antioxidants by stabilizing their catalytic site. Zinc also has vital role in DNA and RNA synthesis by acting as cofactor for nearly 750 zinc- finger transcription factor. Zinc, therefore, plays a pivot role in modulating the immune system and its deficiency has been related to various illnesses. Severe form of zinc deficiency has shown to cause decrement in number of lymphocytes and also increase lymphocyte death via apoptosis. Various studies prove the efficacy of zinc along with its salt against various viral infections namely: herpes, cytomegalovirus and respiratory syncytial virus. In an experiment conducted by Lu et al., zinc has shown to inhibit RNA synthesis of SARS CoV in vitro; and this reaction was reversible on adding zinc chelators. As SARS CoV and SARS CoV2 share 95% similarity in RdRp 3 [30], allows hypothesizing Zinc effectivity against SARS CoV2.
The regimen approved to reduce the prevalence of pneumonia in developing countries contains zinc supplements and it’s because zinc deficiency has been found to enhance the susceptibility of pneumonia among elderly. The mortality rate from pneumonia is twice as high in people who have low zinc levels compared to people who have normal zinc levels [31].
Studies have shown that zinc can inhibit the penetration of SARS CoV-2 virus by decreasing the activity of ACE-2 receptor, a type-1 integral membrane protein present on lipid bilayer of epithelial cells of lung [32]. This has been supported by a study which depicts that zinc in exogenous form inhibits the action of angiotensin converting enzyme -2 to assimilate substrates. Cell culture studies shows that zinc has the ability to inhibit SARS-CoV replication transcription complexes along with that of Nidovirus [33]. A pilot study is conducted among COVID 19 positive subjects in Australia, regarding the benefits and side effects of intravenous zinc administration, is yet to be completed.
A study depicted requirement of more corticosteroids (p=0.02) and an increased lengths of hospital stay (p=0.076) inCOVID-19 patients with zinc deficiency (p<0.001).Many in vitro studies have demonstrated a synergy between zinc and chloroquine/ hydro chloroquine with possibly chloroquine acting as ionophore for zinc due to its positive charge [34]. Skalny, et al. showed that pairing up zinc and pyrithione at low concentration potentially stop the SARS CoV-2 virus from multiplying in cell culture [35]. Therefore, zinc as an adjuvant therapy (with a recommended dose of 25mg/12hr) may have a preventative and/or therapeutic efficacy in the treatment of COVID-19. Other important studies are mentioned in Table 1.
| Title | Authors | Study Type | Objectives | Population | Results |
|---|---|---|---|---|---|
| Pilot trial of high-dose vitamin C in critically ill COVID-19 patients | Jing Zhang et al. [36] | Randomized Control Trial | To check if High-dose vitamin C infusion was effective for severe COVID-19. | Patients with confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections in the ICU. | Patients in the HDIVC group had a steady rise in the PaO2/FiO2 (day 7: 229 vs. 151 mmHg, 95% CI 33 to 122, P=0.01), which was not observed in the control group. |
| Efficacy of high dose vitamin C, melatonin and zinc in Iranian patients with acute respiratory syndrome due to coronavirus infection: a pilot randomized trial. | Darban M et al. [37] | Randomized Control Trial | To investigate the efficacy of vitamin C, melatonin, and zinc in patients with severe Covid-19. | Adults with severe COVID-19 | There were no significant differences between 2 groups (P>0.05). |
| Effect of high-dose intravenous vitamin C on prognosis in patients with SARS-CoV-2 pneumonia. | Kavurgacı Suna et al. [38] | Randomized Control Trial | To examined the effect of high dose intravenous vitamin C. | Adults with severe COVID-19 | No significant change in mortality (p=0.52). |
| The COVID A to Z Randomized Clinical Trial. | Suma Thomas et al. [39] | Randomized Control Trial | To investigate if high dose zinc and vitamin C reduce duration of symptoms in SARS CoV2 patients | PCR confirmed COVID 19 patients above the age of 18 years | No significant difference in the duration of symptoms(p=0.45) |
Table 1: Other important studies.
Conclusion
SARS CoV2 VIRUS has been a huge burden on global public wellbeing and has a set a huge setback on global economies. Due to its high transmission rate, many countries have seen the emergence of third wave. Novel treatment modalities and vaccines are being tested, but management is proving difficult due to the SARS CoV-2 virus's rapid mutation. Therefore, strengthening one's immune system through a well-balanced diet rich in macronutrients and micronutrients plays a significant part in the course of illness. From the discussion, the importance of Vitamin C and zinc as prophylaxis against SARS CoV-2 virus is emphasized. Vitamin- C mainly acts as a potent antioxidant and as a chemoattractant for phagocytes. Zinc, on the other hand, has shown to inhibit replication of virus through its proteolytic action against ACE-2. Inability to monitor zinc levels as they act as a cofactor for various molecules may set as a drawback for its usage. The clinical trials considered in this article, investigates the benefits and side effects of vitamin C via intravenous infusions in patients admitted in intensive care unit. Further studies should look for the prophylactic benefits of vitamin C in intravenous and oral route to healthy individuals or to asymptomatic or mild cases of COVID-19. Studies should also be undertaken regarding proper dosage of these micronutrients in COVID- 19 patients and their interaction with other drugs used in COVID-19 patients.
References
- Fu L, Wang B, Yuan T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J Infect 2020; 80:656-665.
Indexed at, Google Scholar, Cross Ref - Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 2020; 109:102433.
Indexed at, Google Scholar, Cross Ref - Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020; 395:1054-1062.
Indexed at, Google Scholar, Cross Ref - Lauridsen C. From oxidative stress to inflammation: Redox balance and immune system. Poult Sci 2019; 98:4240-4246.
Indexed at, Google Scholar, Cross Ref - Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497-506.
Indexed at, Google Scholar, Cross Ref - Yoshikawa T, Hill T, Li K, et al. Severe acute respiratory syndrome (SARS) coronavirus-induced lung epithelial cytokines exacerbate SARS pathogenesis by modulating intrinsic functions of monocyte-derived macrophages and dendritic cells. J Virol 2009; 83:3039-3048.
Indexed at, Google Scholar, Cross Ref - Fu Y, Cheng Y, Wu Y. Understanding SARS-CoV-2-mediated inflammatory responses: From mechanisms to potential therapeutic tools. Virol Sin 2020; 35:266-271.
Indexed at, Google Scholar, Cross Ref - Iddir M, Brito A, Dingeo G, et al. Strengthening the immune system and reducing inflammation and oxidative stress through diet and nutrition: considerations during the COVID-19 crisis. Nutrients 2020; 12:1562.
Indexed at, Google Scholar, Cross Ref - Murphy K, Weaver C. Janeway's immunobiology. Garland science 2016.
Indexed at, Google Scholar, Cross Ref - Bouayed J, Bohn T. Exogenous antioxidants double-edged swords in cellular redox state: health beneficial effects at physiologic doses versus deleterious effects at high doses. Oxid Med Cell Longev 2010; 3:228-237.
Indexed at, Google Scholar - McGonagle D, Sharif K, O'Regan A, et al. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev 2020; 19:102537.
Indexed at, Google Scholar, Cross Ref - Ganeshan K, Chawla A. Metabolic regulation of immune responses. Annu Rev Immunol 2014; 32:609.
Indexed at, Google Scholar, Cross Ref - Wick G, Hu Y, Schwarz S, et al. Immunoendocrine communication via the hypothalamo-pituitary-adrenal axis in autoimmune diseases. Endocr Rev 1993; 14:539-563.
Indexed at, Google Scholar, Cross Ref - Park JE, Barbul A. Understanding the role of immune regulation in wound healing. Am J Surg 2004; 187:11-16.
Indexed at, Google Scholar, Cross Ref - Cerullo G, Negro M, Parimbelli M, et al. The long history of vitamin C: From prevention of the common cold to potential aid in the treatment of COVID-19. Front Immunol 2020; 2636.
Indexed at, Google Scholar, Cross Ref - Wannamethee SG, Lowe GD, Rumley A, et al. Associations of vitamin C status, fruit and vegetable intakes, and markers of inflammation and hemostasis. Am J Clin Nutr 2006; 83:567-574.
Indexed at, Google Scholar, Cross Ref - Englard S, Seifter S. The biochemical functions of ascorbic acid. Annu Rev Nutr 1986; 6:365-406.
Indexed at, Google Scholar, Cross Ref - Mohammed BM, Fisher BJ, Kraskauskas D, et al. Vitamin C promotes wound healing through novel pleiotropic mechanisms. Int Wound J 2016; 13:572-584.
Indexed at, Google Scholar, Cross Ref - Hemil, Chalker E. Vitamin C can shorten the length of stay in the ICU: A meta-analysis. Nutrients 2019; 11:708.
Indexed at, Google Scholar, Cross Ref - Te Velthuis AJ, van den Worm SH, Sims AC, et al. Zn2+ inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture. PLoS Pathog 2010; 6:e1001176.
Indexed at, Google Scholar, Cross Ref - Chiscano-Cam,Ruiz-Rodriguez JC, Ruiz-Sanmartin A, et al. Vitamin C levels in patients with SARS-CoV-2-associated acute respiratory distress syndrome. Crit Care 2020; 24:1-3.
Indexed at, Google Scholar, Cross Ref - Holford P, Carr AC, Jovic TH, et al. Vitamin C: An adjunctive therapy for respiratory infection, sepsis and COVID-19. Nutrients 2020; 12:3760.
Indexed at, Google Scholar, Cross Ref - Tyml K. Vitamin C and microvascular dysfunction in systemic inflammation. Antioxidants 2017; 6:49.
Indexed at, Google Scholar, Cross Ref - Hiedra R, Lo KB, Elbashabsheh M, et al. The use of IV vitamin C for patients with COVID-19: A case series. Expert Rev Anti Infect Ther 2020; 18:1259-1261.
Indexed at, Google Scholar, Cross Ref - Liu F, Zhu Y, Zhang J, et al. Intravenous high-dose vitamin C for the treatment of severe COVID-19: Study protocol for a multicentre randomised controlled trial. BMJ Open 2020; 10:e039519.
Indexed at, Google Scholar, Cross Ref - Patel O, Chinni V El, Khoury J, et al. A pilot double blind safety and feasibility randomized controlled trial of high dose intravenous zinc in hospitalized COVID 19 patients. J Med Virol 2021; 93:3261-3267.
Indexed at, Google Scholar, Cross Ref - Razzaque MS. COVID-19 pandemic: can maintaining optimal zinc balance enhance host resistance? Tohoku J Exp Med 2020; 251:175-181.
Indexed at, Google Scholar, Cross Ref - Maggini S, Pierre A, Calder PC. Immune function and micronutrient requirements change over the life course. Nutrients 2018; 10:1531.
Indexed at, Google Scholar, Cross Ref - Wintergerst ES, Maggini S, Hornig DH. c. Ann Nutr Metab 2007; 51:301-23.
Indexed at, Google Scholar, Cross Ref - Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020; 395:565-74.
Indexed at, Google Scholar, Cross Ref - Barnett JB, Hamer DH, Meydani SN. Low zinc status: A new risk factor for pneumonia in the elderly? Nutr Rev 2010; 68:30-37.
Indexed at, Google Scholar, Cross Ref - McPherson SW, Keunen JE, Bird AC, et al. Investigate oral zinc as a prophylactic treatment for those at risk for COVID-19. Am J Ophthalmol 2020; 216:5-6.
Indexed at, Google Scholar, Cross Ref - Truwit JD, Hite RD, Morris PE, et al. Effect of vitamin C infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: The CITRIS-ALI randomized clinical trial. JAMA 2019; 322:1261-70.
Indexed at, Google Scholar, Cross Ref - Jothimani D, Kailasam E, Danielraj S, et al. COVID-19: Poor outcomes in patients with zinc deficiency. Int J Infect Dis 2020; 100:343-349.
Indexed at, Google Scholar, Cross Ref - Skalny AV, Rink L, Ajsuvakova OP, et al. Zinc and respiratory tract infections: Perspectives for COVID ??19. Int J Mol Med 2020; 46:17-26.
Indexed at, Google Scholar, Cross Ref - Zhang J, Rao X, Li Y, et al. Pilot trial of high-dose vitamin C in critically ill COVID-19 patients. Ann Intensive Care 2021; 11:1-2.
Indexed at, Google Scholar, Cross Ref - Rawat D, Roy A, Maitra S, et al. Vitamin C and COVID-19 treatment: A systematic review and meta-analysis of randomized controlled trials. Diabetes Metab Syndr 2021; 15:102324.
Indexed at, Google Scholar, Cross Ref - Suna K, Melahat U, Murat Y, et al. Effect of high-dose intravenous vitamin C on prognosis in patients with SARS-CoV-2 pneumonia. Med Clin 2022; 158:356-360.
Indexed at, Google Scholar, Cross Ref - Thomas S, Patel D, Bittel B, et al. Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: The COVID A to Z randomized clinical trial. JAMA Netw Open 2021; 4:e210369.
Indexed at, Google Scholar, Cross Ref
Author Info
Sushma Selvanathan1 and Pramita A Muntode2
1Department of Medicine, Jawaharlal Nehru Medical College, India2Department of Community Medicine, Datta Meghe Institute of Medical Sciences, India
Received: 03-Jan-2023, Manuscript No. jrmds-22-76447; Accepted: 05-Jan-2023, Pre QC No. jrmds-22-76447; Editor assigned: 05-Jan-2023, Pre QC No. jrmds-22-76447; Reviewed: 20-Jan-2023, QC No. jrmds-22-76447; Revised: 27-Jan-2023, Manuscript No. jrmds-22-76447; Published: 03-Feb-2023
