Research - (2020) Advances in Dental Surgery
Multiple Sclerosis Associated with Systemic Sclerosis (Scleroderma): Case Report
Aqeel Almutairi1* and Mohamed Al-Jumah2
*Correspondence: Aqeel Almutairi, Department of Neurology, National Neuroscience Institute, King Fahad Medical City, Saudi Arabia, Email:
Abstract
Introduction: Multiple sclerosis is one of the common chronic inflammatory demyelinating disease of the central nervous system (CNS), affecting more than 2 million people worldwide. The pattern of Multiple sclerosis varies from patient to patient and is unpredictable. Multiple sclerosis (MS) has been increasingly reported to be associated with other autoimmune diseases not affecting the central nervous system especially connective tissue disease.
Objective: To report a case of multiple sclerosis coinciding with systemic sclerosis.
Clinical presentation: A 25-year-old female diagnosed with systemic sclerosis and started on methotrexate then after months patient started to complain of diplopia, eye pain and blurring of vision. Patient seen and after detailed clinical evaluation we considered demyelinating disease MRI showed (showing features of demyelinating disease) and lumbar puncture (showing oligoclonal band), a diagnosis of multiple sclerosis (MS) was established. Patient started on Rituximab for treating her systemic sclerosis and multiple sclerosis after discussion done with rheumatologist.
Conclusion: Detailed history and systemic examination followed by laboratory and radiological investigation should be performed whenever there is a suspicion of Multiple sclerosis, especially if it occurs along with other connective tissue diseases.
Keywords
Multiple sclerosis, Autoimmune diseases, Rheumatoid arthritis, Hashimoto’s thyroiditis, Systemic sclerosis
Introduction
Multiple sclerosis is one of the most common chronic inflammatory demyelinating disease of the central nervous system (CNS), affecting more than 2 million people worldwide [1]. The course of Multiple sclerosis is varied form patient to patient and unpredictable. Optic neuritis is one of most common clinical features of multiple sclerosis, may represent the first sign of the disease [2]. Other manifestation of multiples sclerosis may include diplopia, numbness, spinal cord symptoms (bowel, bladder, sexual dysfunction) and sensory loss.
The pathologic feature in MS is the breakdown of the myelin sheath, with relative sparing of axons. Multiples sclerosis (MS) most of the time presented as isolated autoimmune disease but lately multiple sclerosis has been increasingly reported to be associated with other autoimmune diseases not affecting the central nervous system such as rheumatic diseases, including systemic lupus erythematosus (SLE), rheumatoid arthritis, Hashimoto’s thyroiditis, primary Sjogren’s syndrome, and ankylosing spondylitis [3-6]. In this case we present the coexist of systemic sclerosis and multiple sclerosis.
Case Presentation
We present a 25-year-old white female, dentist, who was diagnosed as case of systemic sclerosis (scleroderma) 7 weeks ago based on skin biopsy on methotrexate started to complain from diplopia especially when looking to the right for 2 weeks associated with eye pain and blurring vision. Patient presented to ophthalmology clinic in privet hospital were the diagnosed her with 6th carinal nerve palsy initially then neurology consultation has been requested. Patient seen by Adult neurology where they suspect demyelinating disorder based on her examination and the clinical picture.
On physical examination showed conscious, women, alert and oriented to time, place, and person. Her vital signs were as follows: heart rate, 88 beats per minute; respiratory rate, 20 cycles per minute; blood pressure, 121/61 mmHg; temperature, 36.3°C; and oxygen saturation, 98% on Room Air. Patient looks concerned about her current situation. Language examination is unremarkable. There was intraocular ophthalmoplegia and coordination exam showed mild ataxia. Other cranial nerves examinations were intact. There was no sensory deficit and motor examinations showed normal tone with full power in all 4 limbs with deep tendon reflexes +2 all over. Blood was drawn for a complete blood count, urea and electrolytes, liver function test, coagulation profile, serum glucose level, thyroid function and ESR were all within the normal limit. Also, we sent for ANA, ANCA and RF all were negative. Urine analysis did not show infection or hematuria.
Patient started on methylprednisolone for 7 days by the privet hospital. MRI with contrast and Visual evoked potentials were requested MRI brain with contrast showed Scattered areas of altered signal intensity in the supratentorial as well as infratentorial region including deep parietal area and the brainstem. Faint signal alteration in the canalicular part of the right optic nerves extending up to the optic chiasm on the right most likely related to optic neuritis. These lesions were highly suggestive of demyelinating disease. Visual evoked potentials showed delay P100 latency bilaterally suggestive of involvement of visual pathway. Then patient refer to higher neurology center for further evaluation and management. Her case was evaluated and assessed. Old investigations in the privet hospital were reviewed and Lumper Puncture was advised. The LP was unremarkable for infection diseases and not suggestive of autoimmune disorder the only finding was oligoclonal band in CSF. All differential diagnosis was excluded depending in clinical, investigation and Radiological results. After confirming the diagnosis of multiple sclerosis, we break the news for the patient, and we discuss with her that this might be rare, but it can be occurred.
Discussion with other neuroimmunology consultants done regarding the suitable management plan. Furthermore, we involved rheumatologist in the case, and we all agreed that patient should stope methotrexate and should be started on Rituximab every 6 months. Patient was informed about the management plan and she agreed. 6 months later patient seen in the clinic and she was fine clinically. MRI brain with contrast follow up did not showed any progression in the disease’s activity. Patient tolerated rituximab first dosage. Follow up investigations was unremarkable. Due to low mood patient was seen in mental health clinic and was started on escitalopram. After 1 year of being started on Rituximab patient evaluated again in the clinic and was tolerated the management well with not history of relapse (Figure 1).
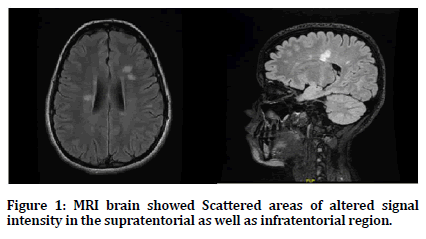
Figure 1. MRI brain showed Scattered areas of altered signal intensity in the supratentorial as well as infratentorial region.
Discussion
In this case, we are reporting a case of female with rare coexist between multiple sclerosis and systemic sclerosis reported. The diagnosis of MS in patient with systemic sclerosis is challenging. The neurological features of systemic sclerosis are unusual. Although rare but cases of multiple sclerosis and other autoimmune disease has been reported. Of connective tissue disorder SLE was often associated with multiple sclerosis [7]. Trostle et al [8] reported 4 cases that found to have MS and systemic sclerosis on 1986 but we did not find any other case reports between MS and systemic sclerosis since that time. Henderson et al [9] did a study to find occurrence of autoimmune disease in patient with MS and their family that they found individuals with MS have a genetic predisposition to autoimmunity in general.
An associated between MS and systemic sclerosis was not surprising, 2 disorder within autoimmune origin. Furthermore, the association of MS and systemic sclerosis is remarkably interesting and deserves further investigation. The pathophysiologic link of these diseases remains unknown. T cells seem to play a major role in both diseases. Thus, T cells and TNF-alpha drive the in Xammatorycascade that will activates metalloproteinases and other degradative enzymes responsible for the demyelination in MS [10]. This case report highlights the importance of considering multiple sclerosis with other autoimmune disease especially if patient had symptoms or sign which can be suggestive for other autoimmune disease. Furthermore, our report highlights the interesting coexist between MS and SSc that may be due to an overlapping pathogenetic mechanism for both processes.
Conclusion
We highly recommend the importance of detailed history with involving all rheumatological diseases in consideration together with systemic examination followed by laboratory and radiological investigation whenever there is a suspicion of MS especially with other connective tissue disease and autoimmune disease.
Conflict Of Interest Statement
None declared.
References
- GBD 2015 Neurological disorders collaborator group. Global, regional, and national burden of neurological disorders during 1990-2015: A systematic analysis for the global burden of disease study 2015. Lancet Neurol 2017; 16:877-897.
- Chen L, Gordon LK. Ocular manifestations of multiple sclerosis. Curr Opin Ophthalmol 2005; 16:315–320.
- Fulford KWM, Catterall RD, Delhanty JJ, et al. A collagen disorder of the nervous system presenting as multiple sclerosis. Brain 91972; 5:373-386.
- Khan MA, Kushner I. Ankylosing spondylitis and multiple sclerosis: A possible association. Arthritis Rheum 1979; 22:784786.
- Baker HWG, Balla JI, Burger HG, et al. Multiple sclerosis, and autoimmune diseases. Aust NZJ Med 1972; 3:256260.
- Alexander EL, Provost TT, Stevens MB, et al. Neurologic complications of primary Sjogren’s syndrome. Medicine 1982; 61:247-257.
- Fulford KWM, Catterall RD, Delhanty JJ, et al. A collagen disorder of the nervous system presenting as multiple sclerosis. Brain 1972; 95:373-386.
- Trostle DC, Helfrich D, Medsger TA. Systemic sclerosis (scleroderma) and multiple sclerosis. Arthritis and rheumatism. J Am College Rheumatol 1986; 29:124-127.
- Henderson Robert D, Bain Christopher J, Pender Michael P. The occurrence of autoimmune diseases in patients with multiple sclerosis and their families. J Clin Neurosci 2000; 7:434-437.
- Ram M, Sherer Y, Shoenfeld Y. Matrix metallopro-teinase-9 and autoimmune diseases. J Clin Immunol 2006; 26:299-307.
Author Info
Aqeel Almutairi1* and Mohamed Al-Jumah2
1Department of Neurology, National Neuroscience Institute, King Fahad Medical City, Riyadh, Saudi Arabia2KAIMRC, King Saud Ben Abdul-Aziz University for Health Sciences, NGHA and MS center, Prince Mohammed Ben Abdul-Aziz Hospital,, MOH, Riyadh, Saudi Arabia
Citation: Aqeel Almutairi, Mohamed Al-Jumah, Multiple Sclerosis Associated with Systemic Sclerosis (Scleroderma) : Case Report, J Res Med Dent Sci, 2020, 8 (7): 1-3.
Received: 21-Oct-2020 Accepted: 12-Nov-2020
