Case Report - (2019) Volume 7, Issue 5
Modified Coronally Advanced Flap with Platelet Rich Fibrin as a Scaffold for Periodontal Regeneration in Gingival Recession: A Case Report
*Correspondence: Kumar Chandan Srivastava, Department of Anaesthesiology, Preventive Dental Sciences, College of Dentistry, Jouf University, Saudi Arabia, Email:
Abstract
Irrespective of age, gingival recession is a common periodontal problem witnessed worldwide. Varied factors like malocclusion and improper tooth brushing technique can predispose gingival recession. Root exposure has deleterious outcomes like dentinal hypersensitivity, root caries and unaesthetic appearance. Numerous surgical interventions are advocated for its treatment, with the fundamental aim of periodontal regeneration. Modified coronally advanced flap with platelet rich fibrin is preferred over the available treatment modalities. It outscores other approaches, as platelet rich fibrin is an autologous fibrin gel harbouring growth factors which facilitate healing in the treated site with bone and soft tissue regeneration. The current report portrays a case of Miller’s Class I gingival recession which was successfully treated with platelet rich fibrin along with coronally advanced flap.
Keywords
Gingival recession, Platelet rich fibrin, Root coverage, Coronally advanced flap, Periodontal regeneration
Introduction
Gingival recession can be a considered as a gateway to multiple defects in periodontium. In case, if left untreated, leads to root exposure with impaired aesthetic, root sensitivity, bone resorption and eventually tooth loss [1]. Although in surgical periodontics we aspire to achieve a near total regeneration of the lost tooth supporting structures, it always remained an elusive goal.
Numerous root coverage procedures have been advocated in the past in order to restore aesthetics and function. Sub epithelial connective tissue graft with coronally advanced flap (CAF) is considered as a gold standard approach. However, pain and discomfort associated with the donor site always remained a great concern [2]. In addition, questionable longterm stability of CAF alone has been a widely documented. In order to overcome, it is advised to add regenerative materials such as such as guided tissue regeneration material, enamel matrix protein derivatives, alloderm and living tissue engineered human fibroblast derived dermal substitute along with CAF [3]. These additive materials will aid in regenerating the attachment apparatus and ultimately promotes the root coverage. In the recent years Platelet rich fibrin (PRF) has emerged as a healing biomaterial which is autologous in nature and promotes hard and soft tissue healing and regeneration [4]. The aim of the case report is to elucidate the importance of PRF along with CRF in treatment of Millers Class I gingival recession.
Case Report
A 34 years old male patient reported with the teeth sensitivity in his upper right jaw while taking cold beverages. On clinical examination, Miller’s class-I gingival recession was noticed in relation to maxillary right premolars (Figure 1A). With the availability of sufficient width of attached gingiva, surgical planning was directed to the CAF with PRF membrane. Associated risks and benefits of the procedure were explained and a written informed consent was obtained. Primarily, full mouth scaling and root planning was done followed by oral hygiene instructions. Three weeks post phase 1 therapy, surgical procedure was planned.
Surgical procedure
Pre-operative mouth rinse with 0.2% chlorhexidine (Clohex) was given. Operating site was anesthetized with Lignocaine hydrochloride 2% with adrenaline (1:80,000). Primary incisions were made in the mesial and distal directions from cement-enamel junction (CEJ) directing towards mucogingival junction at a 45° angulation with the long axis of 14 and 15 respectively, without interfering with the gingival margin of the neighboring teeth. From these oblique incisions, two vertical incisions were extended beyond the mucogingival junction (Figure 1B). An intra-sulcular incision was made at the buccal aspect of the involved teeth (14 and 15). The full-thickness portion of the flap was limited to 2 to 3 mm beyond the marginal bone crest. The partial-thickness portion extended apically into the vestibule for desired repositioning. The buccal part of the papillae was de-epithelialized to act as a recipient site for the CAF (Figure 1C). The exposed root surface was planned, debrided, and reduced in convexity by means of curettes and burs to obtain a flattened profile.
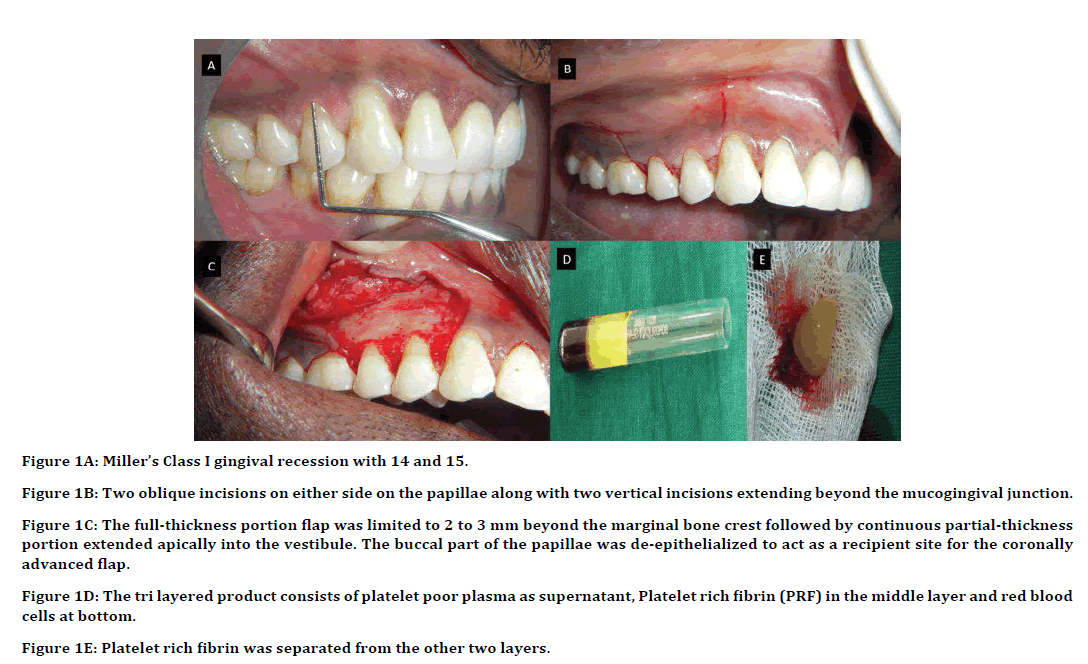
Figure 1A: Miller’s Class I gingival recession with 14 and 15.
Figure 1B: Two oblique incisions on either side on the papillae along with two vertical incisions extending beyond the mucogingival junction.
Figure 1C: The full-thickness portion flap was limited to 2 to 3 mm beyond the marginal bone crest followed by continuous partial-thickness
portion extended apically into the vestibule. The buccal part of the papillae was de-epithelialized to act as a recipient site for the coronally
advanced flap.
Figure 1D: The tri layered product consists of platelet poor plasma as supernatant, Platelet rich fibrin (PRF) in the middle layer and red blood
cells at bottom.
Figure 1E: Platelet rich fibrin was separated from the other two layers.
Preparation and application of PRF membrane
A 10 ml of venous blood sample was drawn from the patient’s arm and immediately, it was centrifuged at 3000 rpm for 10 minutes without anticoagulant. The tri layered product consists of platelet poor plasma as supernatant, PRF in the middle layer and red blood cells at bottom (Figure 1D). PRF clot was separated from the other two layers (Figure 1E). Autologous fibrin membrane was obtained by driving out the serum from the fibrin clot. PRF membrane was placed over the exposed root surface at cemento enamel junction (Figure 2A). The buccal flap was coronally positioned to cover the PRF membrane (Figure 2B) and retained with nonabsorbable 4-0 braided silk sutures (Ethicon) without tension, by means of a sling suture (Figure 2C). Periodontal dressing was applied (Coe-Pak, GC) (Figure 2D).
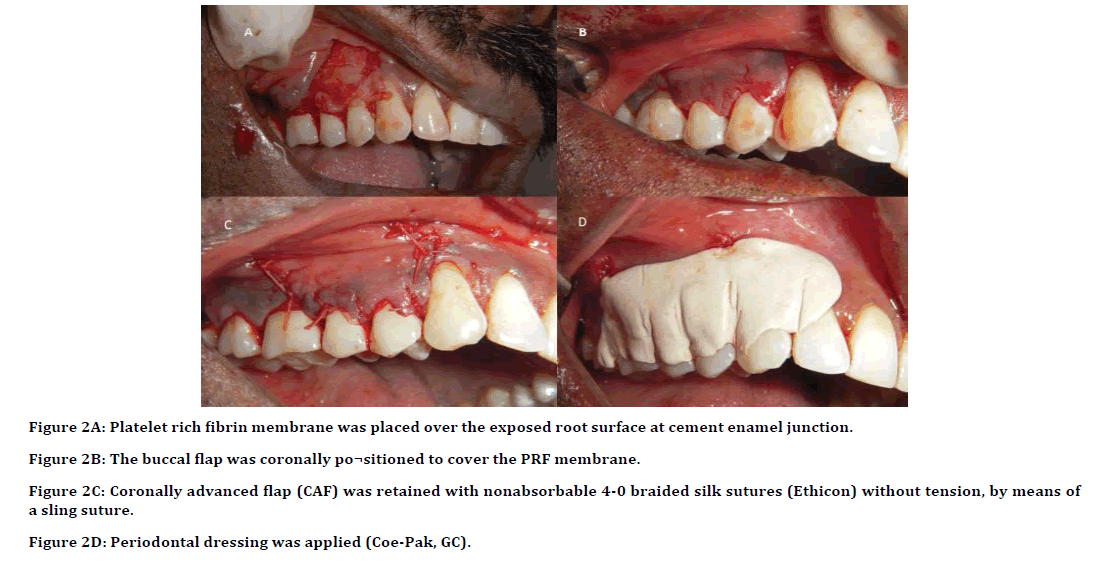
Figure 2A: Platelet rich fibrin membrane was placed over the exposed root surface at cement enamel junction.
Figure 2B: The buccal flap was coronally po¬sitioned to cover the PRF membrane.
Figure 2C: Coronally advanced flap (CAF) was retained with nonabsorbable 4-0 braided silk sutures (Ethicon) without tension, by means of
a sling suture.
Figure 2D: Periodontal dressing was applied (Coe-Pak, GC).
Post-operative care
Post-surgery prescription included a course of amoxicillin 500 mg thrice daily and ibuprofen 400 mg thrice daily for about 5 days. Surgical post-operative instructions were given and advised to visit clinic post 2 weeks for suture removal. On follow up (15 days and 6 months), a complete root coverage was appreciated. (Figure 3A and Figure 3B).
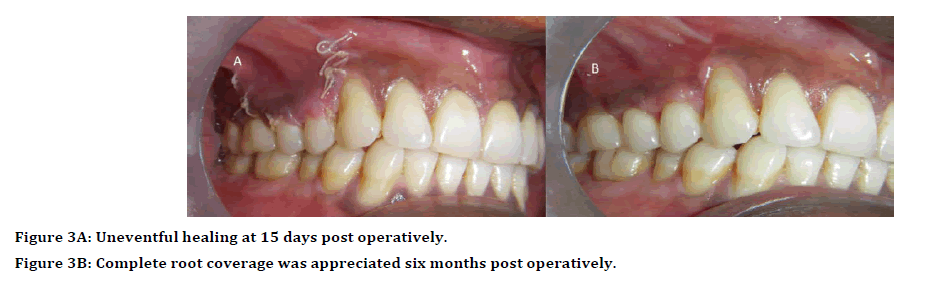
Figure 3A: Uneventful healing at 15 days post operatively.
Figure 3B: Complete root coverage was appreciated six months post operatively.
Discussion
With the increasing awareness, root coverage has become an important treatment modality to achieve aesthetics as well as regeneration of the lost periodontal structure which is the primary goal of periodontal plastic surgery [5].
Various root coverage treatment modalities are available to treat Class I and Class II Miller’s gingival recession. Considering the drawback of CAF alone as being unstable in long term. In our present case report CAF along with PRF is used. PRF being as an autologous fibrin matrix, enriched in growth factors and cytokines has made it a scaffold for tissue regeneration [6].
As it is autologous in nature no rejection is seen within the body as compared to platelet rich plasma where bovine thrombin is used and leads to hypersensitivity. PRF has natural fibrin network which protect growth factor from proteolysis and its 3D organization favours cytokine entrapment and cellular migration [7].
The importance of PRF during the healing phase lies in the fact that the alpha granules of platelet are rich in various growth factors such as PDGF, VEGF and IGF-1 and cytokines and they are released constantly for 7 days in a successive manner which is utmost important for cell proliferation, collagen synthesis and osteoid formation. Among which PGDF in PRF helps in healing and tissue regeneration by chemotactic and mitogenic properties that modulate cellular function [8].
In the present case report, 100% root coverage is achieved at the time of surgery and its results were stable even after 6 months. This is in conjunction with other studies done by Thamaraiselvan et al. and Dohan et al. and which has shown predictable outcome results with CAF and PRF [3,7]. Although there are studies done by, Verma et al. Castro et al. and Moraschini et al. which has shown no added benefits of PRF for periodontal regeneration [6,9,10]. In the present study there is increase in the gingival thickness as compared to base line which are in accordance with other studies done by Dohan et al. [7] PRF being inexpensive, autologous regenerative material has shown predictable outcome for root coverage procedure.
Conclusion
The present case report shows the added benefits of PRF as a healing regenerative material combined with CAF, which can be successfully used for the root coverage procedure.
References
- Zucchelli G, Testori T, De Sanctis M. Clinical and anatomical factors limiting treatment outcomes of gingival recession: A new method to predetermine the line of root coverage. J Periodontol 2006; 77:714–21.
- Srinivas BV, Rupa N, Halini Kumari KV, et al. Root coverage using subepithelial connective tissue graft with platelet-rich plasma in the treatment of gingival recession: A clinical study. J Pharm Bioallied Sci 2015; 7:530–538.
- Thamaraiselvan M, Elavarasu S, Thangakumaran S, et al. Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recession. J Indian Soc Periodontol 2015; 19:66–71.
- Choukroun J, Diss A, Simonpieri A, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101:56-60.
- Sanz M, Simion M, Working Group 3 of the European Workshop on Periodontology. Surgical techniques on periodontal plastic surgery and soft tissue regeneration: Consensus report of Group 3 of the 10th european workshop on periodontology. J Clin Periodontol 2014; 41:92-97.
- Verma UP, Yadav RK, Dixit M, et al. Platelet-rich fibrin: A paradigm in periodontal therapy–A systematic review. J Int Soc Prev Community Dent 2017; 7:227-233.
- Dohan DM, Del Corso M, Diss A, et al. Three-dimensional architecture and cell composition of a Choukroun’s platelet-rich fibrin clot and membrane. J Periodontol 2010; 81:546–55.
- Dohan DM, Choukroun J, Diss A, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101:45-50.
- Castro AB, Meschi N, Temmerman A, et al. Regenerative potential of leucocyte and platelet rich fibrin. Part A: Intra-bony defects, furcation defects and periodontal plastic surgery: A systematic review and meta-analysis. J Clin Periodontol 2017; 44:67-82.
- Moraschini V, Barboza ED. Use of platelet‐rich fibrin membrane in the treatment of gingival recession: A systematic review and meta‐analysis. J Periodontol 2016; 87:281-290.
Author Info
Department of Anaesthesiology, Preventive Dental Sciences, College of Dentistry, Jouf University, Saudi ArabiaCitation: Kumar Chandan Srivastava, Modified Coronally Advanced Flap with Platelet Rich Fibrin as a Scaffold for Periodontal Regeneration in Gingival Recession: A Case Report, J Res Med Dent Sci, 2019, 7(5):25-28.
Received: 22-Aug-2019 Accepted: 11-Sep-2019
