Research - (2020) Volume 8, Issue 1
Marginal Microleakage of Composite Resin Materials Comprising Different Photo Initiators with Surface Sealants and Bonding Agent Application after Thermomechanical Aging
Magrur Kazak*, Rabianur Yurdan, Nazmiye Donmez and Safiye Selin Koymen
*Correspondence: Magrur Kazak, Department of Restorative Dentistry, School of Dental Medicine, Bahcesehir University, Istanbul, Turkey, Email:
Abstract
Aim: To evaluate both gingival and occlusal microleakage of Class II cavities restored with radical amplified photo polymerization (RAP) initiator technology™-based composite resin and camphor Quinone (CQ)-based bulk-fill composite resin and to compare application of two different surface sealant, one dentin bonding agent subsequent to finishing and polishing procedures performed after thermo-mechanical aging.
Materials and methods: Forty extracted, non-carious human third molars were selected. A total of eighty cavities were prepared on both mesio-occlusal and disto-occlusal surfaces of forty teeth. Forty cavities were restored with RAP technology™- based composite resin, Estelite Posterior (EP), other forty cavities were filled with CQ-based bulk-fill composite resin, Filtek Bulk Fill (FBF) then polymerized. After finishing and polishing procedures teeth were stored in distilled water, divided into four subgroups;BisCover LV Group(BC), Perma Seal Composite Sealer Group(PS), All-Bond Universal Group(ABU), Control Group(n=10 cavity for each group). Teeth were thermocycled, subjected to a chewing simulator. Later they were immersed in basic fusch in dye, first sectioned mesiodistally. A total of twenty surfaces were obtained from each group to evaluate gingival dye penetration. For the evaluation of occlusal dye penetration, these twenty surfaces were then sectioned buccolingually. Finally for each group forty surfaces (twenty surfaces for gingival and twenty surfaces for occlusal)were evaluated for dye penetration scores under a stereomicroscope. Statistical analysis was performed with Kruskal Wallis One-Way ANOVA (p<0.05).
Results: Statistical difference was detected between FBF Control and EP Control at both gingival and occlusal walls (p<0.05). No statistically significant differences were noted between FBF Control, FBF BC and FBF ABU groups at both gingival and occlusal walls (p>0.05). No significant differences were found between EP Control, EP BC and EP PS groups (p>0.05), while statistically significant difference between EP Control and EP ABU groups at both the gingival and occlusal walls (p<0.05).
Conclusion: Superiority of CQ-based bulk-fill to RAP technology TM-based composite resin was indicated in terms of microleakage. Composite surface sealants and dentin bonding agent succeeded in reducing marginal microleakage.
Keywords
Photoinitiator, Bulk-fill composite resin, Marginal microleakage, Composite surface sealants, Stereomicroscope
Introduction
Conventional composite resins are widely used for direct restoration due to their conformity with tooth color and ability to support minimally invasive tooth preparation [1]. Despite the advantages of conventional composite resins, polymerization shrinkage [2] remains one of the most important disadvantages. Polymerization shrinkage creates a gap between the cavity wall interface and the restoration margins, leading to microleakage. Microleakage causes the formation of secondary caries, which commonly are detected around the margins of Class II restorations [3]. Polymerization shrinkage is directly related to the way a composite resin polymerizes [4], different types of photoinitiators can help reduce or even eliminate the occurrence of marginal gaps and consequently microleakage [5,6] to improve the quality and stability of the final restoration.
Attempts to decrease microleakage and shorten the working time have resulted in introduction of bulk-fill composite resins. Some reports have claimed that the polymerization kinetics of bulkfill composite materials are better controlled due to an enhanced translucency that allows deeper light penetration with sufficient polymerization [7] and incorporation of a photoactive group in the methacrylate resin of bulk-fill composite material [8]. According to the manufacturers, bulk-fill composites can include placement of bulk with a depth of up to 5 mm depending on the brand without a prolonged polymerization time [9]. The possibility of placement of bulkfill composites up to 5 mm is due to changes in their chemical compositions, which reduce polymerization stresses [10]. Additionally, changing the initiator, such as camphorquinone, lucirin, or Ivocerin, enables placement of a thicker layer, which results in significantly shorter chair time during the restorative procedures [11].
Recently, the patented and innovative ‘radical amplified photopolymerization’ (RAP) initiator system has been implemented with a composite resin material. The RAP technologyTM offers a reduced curing time compared to that of conventional composite resin and facilitates a longer working time. Therefore, although the incremental technique should be used during application of this composite material, the RAP technology provides advantages for clinicians [12].
To achieve a perfect seal [13] and to reduce marginal leakage [14] around the composite, composite surface sealants (CSSs) are recommended. CSSs are characterized by polymerizable materials with low viscosity and high wettability, including unfilled resins and other low-molecular-weight monomers, such as Bis-GMA, UDMA, and TEGDMA [15]. Ramos et al. [16] have shown that marginal rebonding techniques significantly prolong the marginal integrity of the restoration. The mechanism suggests that the microgaps that occur during the finishing and polishing procedures can easily be filled with CSSs due to their high flow rate property, thereby preventing microleakage between the tooth and restoration [16]. In addition to CSSs, commercial adhesive systems (dentin bonding agents) can be used as a surface sealer for rebonding [17].
In the oral environment, teeth are continuously subjected to stress during mastication, swallowing, and parafunctional habits. Therefore, clinical conditions are often simulated in vitro by thermal applications using a thermal cycling machine, and mechanical aging is simulated with a chewing simulator [18,19].
Microleakage is considered a major influencing factor for the longevity of restorative materials and is used by clinicians and researchers as a measure to predict the performance of a restorative material. However, little is known about the long-term clinical behavior/effects of CSSs and dentin bonding agents on microleakage of composite restorations. Therefore, this in vitro study was designed to evaluate the marginal microleakage of Class II ‘slot’ cavities restored with a radical amplified photopolymerization (RAP) initiator technology™-based composite resin and a camphorquinone (CQ)-based bulk-fill composite resin and to compare the application of two different surface sealants and one dentin bonding agent, subsequent to the finishing and polishing procedures performed after thermomechanical aging. The first null hypothesis was that restoring cavities with the RAP technology™-based composite resin would result in less marginal microleakage than restoration with the CQbased bulk-fill composite resin. The second null hypothesis was application of CSSs and a dentin bonding agent would effectively prevent/reduce marginal microleakage.
Materials and Methods
The materials used in the study are listed (Table 1). Forty extracted, non-carious, unerupted, human third molars without defects and cracks were selected for the present study. The study protocol was approved by the ethics committee of the School of Dentistry, Bezmialem Vakif University (14.05.2018/12/112). The teeth were cleaned of soft tissue and other debris using a periodontal scaling instrument, stored in 0.5% chloramine-T solution at 4°C and used within 1 month. Then, the teeth were randomly divided into 2 groups (n=20).
| Materıals | Lot Numbers | Manufacturers | Composıtıons |
|---|---|---|---|
| Sealers | |||
| PermaSeal (PS) (unfilled methacrylate-based resin) | BDNK6 | Ultradent Products, Inc., South Jordan, UT, USA | Bis-GMA, TEGDMA, DMAEMA |
| BisCover LV (BC) (low viscosity liquid polish used to seal composite restoration) | 1700004459 | BISCO Inc., Shamburg, IL, USA | Dipentaerythritol Pentaacrylate Ethanol, Camphorquinone |
| All-Bond Universal (ABU) (Universal Dental Adhesive) | 1700007282 | BISCO Inc., Shamburg, IL, USA | Bis-GMA, MDP,HEMA, Ethanol |
| Etchıng Gel | |||
| Etching Gel | 784152 | DMG Dental Hamburg, Germany |
37% phosphoric acid |
| Adhesıve System | |||
| All-Bond Universal (ABU) (Universal Dental Adhesive) | 1700007282 | BISCO Inc., Shamburg, IL, USA |
Bis-GMA, MDP, HEMA, Ethanol |
| Composıte Materıals | |||
| Estelite Posterior Composite Resin (EP) (packable composite) (A2 Shade) |
W100 | Tokuyama Dental Corporation Inc., Shofu, Japan |
Bis-GMA, TEGDMA, Bis-MPEPP, initiator RAP Silica zirconia filler (mean particle size 2 µm, particle size range 1-10 µm) inorganic filler loading is 84% by weight (70% by volume) |
| Filtek Bulk Fill Posterior Composite Resin (FBF) (bulk-fill composite) (A2 Shade) |
4864A2 | 3M ESPE Dental Products St Paul, MN, USA |
AUDMA, AFM, UDMA, DDDMA, initiator CQ 20 nm silica and 4 to 11 nm zirconia filler, a ytterbium trifluoride filler 100 nm particles inorganic filler loading is 76.5% by weight (58.4% by volume) |
Table 1: The materials used in the study.
Cavity preparations
A total of eighty Class II “slot” cavities were prepared on both mesio-occlusal and distoocclusal surfaces of forty tooth. The preparations were made on each tooth with a #801 round and a #837KR round edge cylinder diamond bur (G&Z Instrumente GmbH, Lustenau, Austria) using a high-speed hand-piece with water-cooling. New burs were used for every five preparations. The dimensions of the slot cavity on each tooth were 3 mm width buccolingually and mesiodistally. The gingival margins of all cavities were placed 1 mm above the cemento-enamel junction. The maximum depth of all cavities was 4 mm. The dimensions mentioned above were confirmed with a periodontal probe.
Restoration techniques
After preparations, the cavities were etched with 37% phosphoric acid gel (Etching Gel, DMG Dental, Hamburg, Germany) for 30 seconds on enamel and 15 seconds on dentin tissues. Then, the teeth were rinsed for 20 seconds and gently air-dried to prevent excessive drying of the dentin tissue. Immediately after etching, the adhesive system (All-Bond Universal, BISCO Inc., Shamburg, IL, USA) was applied as two separate coats; then, the cavities were scrubbed with a microbrush for 10-15 seconds per coat, air-dried thoroughly for 10 seconds, and light-cured for 10 sec with a light-emitting diode (LED) lightcuring unit (LCU) (VALO Cordless LED Curing Light, Ultradent Products Inc., South Jordan, UT, USA) (standard power mode: 1000 mW/ cm2; multiwavelength LED that produces a highintensity light at 395–480 nm). The groups and subgroups were as follows:
In Group A (n=20), the cavities were restored with a RAP technology™-based composite resin [Estelite Posterior (EP), A2, Tokuyama Dental Corporation Inc., Shofu, Japan] according to the manufacturer’s recommendation. Before starting the restorations, an otomatrix was applied to the tooth and tightened with a matched instrument (SuperMat matrix and tightener KerrHawe, Bioggio, Switzerland). Then, the cavities were filled with composite resin materials using an oblique incremental technique (three increments), each with an increment of 2 mm. The first increment was placed on the gingival wall to obtain a contact surface in the inner surface of the matrix band. The second increment was placed on the lingual wall, and the last increment was placed on the buccal wall. Each increment was light-cured for 10 seconds with the LED LCU.
In Group B (n=20), the cavities were restored using a CQ-based bulk-fill composite resin [Filtek Bulk Fill Posterior Restorative (FBF), A2, 3M-ESPE Dental Products, St. Paul, MN, USA] with a single step and a 4 mm thickness. Before starting the restorations, an otomatrix was applied to the tooth and tightened with a matched instrument (SuperMat matrix and tightener, KerrHawe, Bioggio, Switzerland). The bulk-placed composite material was lightcured with the LED LCU for 10 seconds from the occlusal surface.
After removing the matrixes, each restoration was also light-cured from the vestibule and lingual surfaces to obtain maximum polymerization. As a result, forty cavities were restored with EP, other forty cavities were filled with FBF. In each group, the mesio-occlusal and disto-occlusal cavities were restored with the same composite resin material. Finally, all of the restorations were finished with #368 pointed and #858 needle diamond burs (GZ Instrumente GmbH, Austria), polished with #4001 polishing points (Composite Microfil Polishers, Kenda AG, Liechtenstein) and divided into four subgroups according to the application of the composite surface sealants and dentin bonding agent (n=10 cavity for each group).
Subgroup 1: The restoration surfaces were etched with 37% phosphoric acid gel for 15 seconds and then rinsed gently and dried. Following this procedure, BisCover LV (BISCO, Inc., Shamburg, IL, USA) was applied on the restoration surfaces with a microbrush, left for 15 seconds for evaporation and then light-cured for 30 seconds with the LED LCU.
Subgroup 2: The restoration surfaces were etched with 37% phosphoric acid gel for 20 seconds and then rinsed and air-dried for 5 seconds. After these applications, PermaSeal Composite Sealer (Ultradent Products, Inc., South Jordan, UT, USA) was applied to the surfaces and light-cured for 20 seconds with the LED LCU.
Subgroup 3: The restoration surfaces were etched with 37% phosphoric acid gel for 30 seconds, rinsed, and dried. Then, the dentin bonding agent All-Bond Universal (BISCO Inc., Shamburg, IL, USA) was applied to the surfaces and light-cured 10 seconds with the LED LCU.
Subgroup 4: This group was the Control Group. No CSS or dentin bonding agent was applied to the restoration surfaces.
After these procedures, all specimens were stored in distilled water at 37°C for 1 week. Following storage, the teeth were thermocycled in distilled water (10.000 cycles at 5°C and 55°C ± 1°C with a dwell time of 30 seconds and transfer time of 10 seconds) (SD Mechatronik Thermocycler, Germany). The teeth were embedded in acrylic blocks and then subjected to 50,000 cycles in the chewing simulator with a 50 N vertical load at a frequency of 1.7 Hz (SD Mechatronik Chewing Simulator CS-4, Germany) [19]. Subsequent to the thermomechanical aging procedure, the entire surface of each specimen was covered with two coats of nail varnish up to 1 mm in area far from the restoration margins. Then, the teeth were soaked in 0.5% basic fuchsin solution (A.D.R. Group, Mediko Kimya, Turkey, Lot Number: 180305) for 24 hours at 37°C. Next, the teeth were cleaned under tap water to remove excess dye, brushed gently for 1 minute and dried at room temperature. Later, the crowns were removed from the roots using a diamond bur, and teeth were first sectioned mesiodistally using a diamond disc (Mecatome T180 Cutting Machine, Presi, France). A total of twenty surfaces were obtained from each group in order to evaluate the gingival dye penetration. For occlusal dye penetration, these twenty surfaces were then sectioned buccolingually. Finally for each group forty surfaces (twenty surfaces for gingival and twenty surfaces for occlusal) were obtained and evaluated for the dye penetration scores. The occlusal and gingival microleakage dye penetration scores were evaluated under a stereomicroscope with 40x magnification (SMZ 1000, NIKON, Japan). The degree of marginal leakage was evaluated using a standardized scoring system (Table 2, Figures 1 and 2) [20].
| Scores | Definition of the scores |
|---|---|
| 0 | Perfect adaptation/ No dye penetration |
| 1 | Dye penetration up to one-half of the cavity wall |
| 2 | Dye penetration greater than one-half, but not reaching to the axial wall |
| 3 | Dye penetration reaches to the axial wall |
Table 2: The scale used to evaluate the dye penetration scores at the occlusal and gingival restoration interfaces.
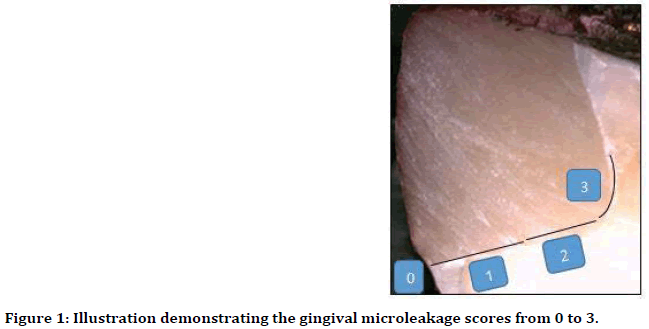
Figure 1. Illustration demonstrating the gingival microleakage scores from 0 to 3.
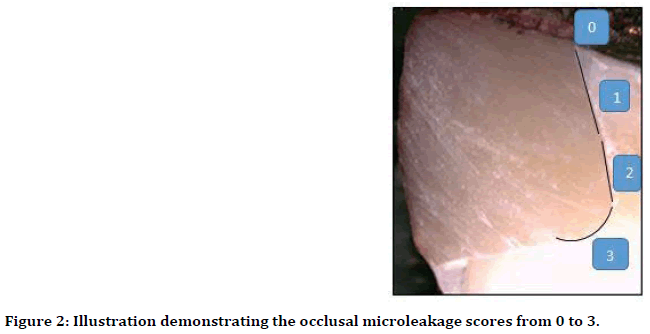
Figure 2. Illustration demonstrating the occlusal microleakage scores from 0 to 3.
Statistical analysis
The microleakage values did not show normal distribution according to Saphiro Wilks test. Therefore, non-parametric test, Kruskal Wallis One-Way ANOVA, was performed among groups for multiple comparisons. The results for all data were analyzed at a significance level of p<0.05 [21].
Results
In terms of materials, a statistically significant difference was found between the FBF Control and EP Control groups at both the gingival and occlusal walls (p<0.05). The EP Control group exhibited more microleakage than the FBF Control group (Table 3, Figure 3A and 3B). No statistically significant differences were observed between FBF Control, FBF Biscover and FBF All Bond Universal groups at both the gingival and occlusal walls (p>0.05). A statistically significant difference was detected between FBF Control and FBF Permaseal groups at gingival walls (p<0.05) while no significant difference at the occlusal walls (p>0.05). No statistically significant differences were observed between FBF Biscover, FBF Permaseal groups and FBF All Bond Universal groups at both gingival and occlusal walls (p>0.05). While FBF Permaseal group showed a statistically significant difference between FBF All Bond Universal group at the gingival walls (p<0.05), no significant difference was found at the occlusal walls (p>0.05). No statistically significant differences were observed between EP Control, EP Biscover and EP Permaseal groups at both the gingival and occlusal walls (p>0.05). A statistically significant difference was detected between EP Control and EP All Bond Universal groups at both gingival and occlusal walls (p<0.05). Less microleakage was detected in the EP All Bond Universal group than EP Control group (Table 3, Figure 3B and 3C). No statistically significant differences were observed between EP Biscover, EP Permaseal and EP All Bond Universal groups at both the gingival and occlusal walls (p>0.05). A statistically significant difference was observed between the EP PermaSeal and EP All Bond Universal groups at both the gingival and occlusal walls (p <0.05). EP Permaseal group showed higher microleakage than EP All Bond Universal group (Table 3, Figure 3C and 3D). A statistically significant difference was detected between FBF Biscover and EP Biscover groups at gingival walls (p<0.05) while no significant difference at the occlusal walls (p>0.05). A statistically significant difference was observed between the FBF PermaSeal and EP PermaSeal groups at both the gingival and occlusal walls (p<0.05). Less microleakage was observed in the FBF PermaSeal group than in the EP PermaSeal group (Table 3, Figure 3D and 3E). No statistically significant difference was observed between FBF All Bond Universal and EP All Bond Universal groups at the both gingival and occlusal walls (p>0.05).
| Materıals | Occlusal Scores |
Gıngıval Scores |
Occlusal | Gıngıval | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 0 | 1 | 2 | 3 | Median (Min-Max) | Median (Min-Max) | |
| Filtek Bulk Fill (FBF) Control | 75% (n=15) |
5% (n=1) |
20% (n=4) |
- | 40% (n=8) |
55% (n=11) |
- | 5% (n=1) |
(0-2) | (0-3) |
| Filtek Bulk Fill (FBF) BisCover (BC) | 90% (n=18) |
10% (n=2) |
- | - | 80% (n=16) |
20% (n=4) |
- | - | (0-1) | (0-2) |
| Filtek Bulk Fill (FBF) PermaSeal (PS) | 95% (n=19) |
5% (n=1) |
- | - | 95% (n=19) |
5% (n=1) |
- | - | (0-1) | (0-2) |
| Filtek Bulk Fill (FBF) All-Bond Universal (ABU) | 55% (n=11) |
20% (n=4) |
20% (n=4) |
5% (n=1) |
40% (n=8) |
40% (n=8) |
5% (n=1) |
15% (n=3) |
(0-3) | (0-3) |
| Estelite Posterior (EP) Control | 20% (n=4) |
30% (n=6) |
5% (n=1) |
45% (n=9) |
15% (n=3) |
30% (n=6) |
- | 55% (n=11) |
(0-3) | (0-3) |
| Estelite Posterior (EP) BisCover (BC) | 55% (n=11) |
10% (n=2) |
- | 35% (n=7) |
25% (n=5) |
25% (n=5) |
10% (n=2) |
40% (n=8) |
(0-3) | (0-3) |
| Estelite Posterior (EP) PermaSeal (PS) | 15% (n=3) |
10% (n=2) |
5% (n=1) |
70% (n=14) |
20% (n=4) |
- | 5% (n=1) |
75% (n=15) |
(0-3) | (0-3) |
| Estelite Posterior (EP) All-BondUniversal (ABU) | 80% (n=16) |
15% (n=3) |
5% (n=1) |
- | 55% (n=11) |
40% (n=8) |
- | 5% (n=1) |
(0-2) | (0-3) |
Table 3: Distribution of dye penetration scores, percentage of dye penetration values (RL%), and median values of groups for marginal microleakage.
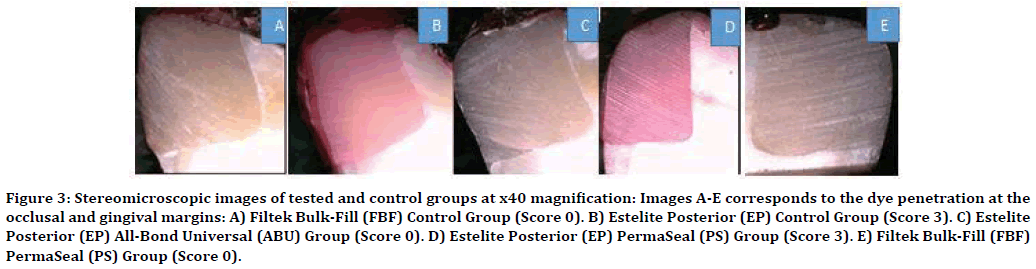
Figure 3. Stereomicroscopic images of tested and control groups at x40 magnification: Images A-E corresponds to the dye penetration at the occlusal and gingival margins: A) Filtek Bulk-Fill (FBF) Control Group (Score 0). B) Estelite Posterior (EP) Control Group (Score 3). C) Estelite Posterior (EP) All-Bond Universal (ABU) Group (Score 0). D) Estelite Posterior (EP) PermaSeal (PS) Group (Score 3). E) Filtek Bulk-Fill (FBF) PermaSeal (PS) Group (Score 0).
Discussion
In this in vitro study, the marginal microleakage of Class II ‘slot’ cavities restored with RAP technology®-based composite resin and CQbased bulk-fill composite resin were evaluated, and the applications of two different surface sealants and one dentin bonding agent subsequent to the finishing and polishing procedures after thermomechanical aging were compared. The results demonstrated the superiority of CQ-based bulk-fill composite resin in terms of marginal microleakage. Therefore, the first null hypothesis was rejected. As noted in our results, the CSSs and dentin bonding agent were effective in reducing marginal microleakage for both composite resins. Therefore, the second null hypothesis was accepted.
Although many techniques have been tried, polymerization shrinkage is accepted to not completely disappear. Since a direct relationship between polymerization contraction stress and marginal adaptation has been demonstrated [4], new restorative materials are being developed. In the present study, a RAP technology®-based composite resin material with a high filler load (84% by weight) that offered decreased polymerization shrinkage and a CQ-based bulkfill composite material with less volumetric (polymerization) shrinkage were tested. Also the marginal sealing ability of different types of photoinitiators included in the composite resins was compared.
The literatures report various methods to evaluate microleakage between the tooth and the restorative material. The dye penetration technique is a commonly used, low cost, simple, easy, and comparable method for microleakage evaluation [22]. In this study, a conventional dye penetration method was chosen. In the dye penetration tests, various dyes can be used. Basic fuchsin (0.5-2%) dye is one of the dyes that can be used to detect microleakage [23]. Therefore, in the present study, 0.5% basic fuchsin dye was used for evaluation of marginal microleakage.
To minimize the occurrence of microleakage at the tooth/restoration interface, some clinicians prefer a bonding agent for rebonding of the restoration after the finishing and polishing procedures. The main purpose of using a bonding agent is to create a stable seal between the restoration and the tooth structure and to close the gaps [24]. Currently, CSSs have been developed as an alternative to dentin bonding agent material [25]. Some studies have suggested that restoration cavity-sealing is improved by coating with a low viscosity surface sealant, which is a type of light-polymerizable, resin-based material that can penetrate into microgaps or microdefects on the restoration interfaces to reduce microleakage [16]. CSSs have enhanced formulations, including unfilled resins, low-molecular-weight monomers (Bis- GMA, UDMA, TEGDMA), and photoinitiators [25]. The CSS application and light-curing processes are performed similarly after the acid-etching process, but the acid-etching and light-curing times differ according to the manufacturer's instructions. Therefore, in this study, two CSSs and one dentin bonding agent were used as coating materials to compare their effects on the microleakage of different composite materials.
To assess the in vitro performance of a resin material, thermal cycling and mechanical loading are common methods that are used to simulate the long-term stresses and thermal changes to which the restorations are exposed [26]. Additionally, restorations have been reported to be exposed to 1,000,000 active cycles, which are equal to 20 years of aging time [27]. Based on this result; 10,000 cycles correspond to 1 year of a thermal aging procedure. Therefore, in the present study to obtain real data, the teeth were exposed to 10,000 thermal cycles at 5-55 °C and 50,000 times chewing force in the axial direction with 100 N at 1.7 Hz [28].
In this in vitro study, the CQ-based bulk-fill (FBF) composite material showed less microleakage than the RAP initiator technology™-based composite resin. The composition such as; photoinitiators, fillers and organic matrix, is one of the parameters that may affect the degree of polymerization of bulk-fill composites [29]. In the present study the tested composite materials were compared according to their photoinitiators. Current composite resins utilize a variety of alpha diketone initiators; such as CQ, phenylpropanedione (PPD), and acylphosphine oxide (lucerin TPO), and germanium-based compounds, such as bis-(4-methoxybenzoyl) dievthyl-germane (Ivocerin), which can be irradiated using a visible light [30]. Activation of these photoinitiators is dependent upon appropriate dental LCU irradiation at wavelengths that overlap absorption of the photoinitiator. LED LCUs have become increasingly popular and are more efficient than QHT due to their ability to generate narrow ranges of wavelength output near the maximum absorbance of CQ (approximately 468 nm) [31]. The tested bulkfill composite resin material (FBF) was based on the photoinitiator CQ. The other tested material (EP) was a RAP initiator technology™-based composite resin. With the RAP technology, CQ is recycled within the polymerization initiator generation reaction, and a single CQ molecule can produce multiple initiator radicals [32]. According to the manufacturer, the clinicians can use any conventional light curing unit with a wavelength range of 400 to 500 nm (peak: 470 nm), which is the absorption spectrum of CQ contained in the material of EP as a photoinitiator [33]. In the present study, VALO was used as an LED LCU. VALO LED LCU has a multiwavelength that produces a high-intensity light at 395–480 nm. This broad-spectrum light output means that VALO is capable of polymerizing all light-curable dental materials, including those with CQ [34]. Therefore, it can be concluded that incorporating only a novel photoinitiator for a composite resin material may not be sufficient to overcome polymerization shrinkage and marginal leakage. Moreover, the photoinitiator concentration was reported to influence polymerization shrinkage stress and consequently gap formation [35]. Unfortunately, the manufacturers did not give any explanations about the photoinitiator concentrations of the tested materials. Therefore, the CQ-based bulk-fill composite resin material may have a higher photoinitiator concentration than the RAP initiator technology®-based composite resin, which might result in less microleakage. Another reason of the less microleakage that was observed for FBF could be the composition of the material. Indeed, EP has a higher filler load (84% by weight) than FBF (76.5% by weight), which offers decreased polymerization shrinkage. However, different from the composition of EP, FBF contains two novel methacrylate monomers that, in combination, act to lower polymerization stress. Therefore, in this in vitro study, the superiority of bulk-fill to a high filler load composite resin was demonstrated.
Different surface sealants were chosen to evaluate how their compositions influenced the fluidity and penetrability, thus prevented/ reduced marginal microleakage. According to the results of this study, none of the tested surface sealants or the dentin bonding agent completely prevented dye penetration on the occlusal and gingival walls. However, they succeeded in reducing the marginal microleakage.
When the combinations of different surface sealants and denting bonding agent with FBF material, PS (PermaSeal) was determined to be the most compatible surface sealant material with FBF showing the highest Score 0 (95%). Numerically, the lowest microleakage score (only 5% for Score 1) was obtained for the combination of FBF and PS when compared with those of the other groups. This result can be considered to arise from the structure of PS, which contains the TEGDMA monomer. The low molecular weight of TEGDMA allows PS to flow into small defects and to penetrate deeply into microgaps, thereby to seal the cavity margins [36]. Significant difference was obtained between the EP Control and EP ABU groups at both the gingival and occlusal walls (p<0.05). When evaluated numerically, the lowest microleakage scores (Occlusal Score 0: 80%, Gingival Score 0: 55%) were detected for the EP and ABU combination. From this perspective, ABU was investigated as the most compatible surface sealant material with EP compared with the results obtained with the other CSS materials. The compatibility of ABU can be attributed to the material content, because ABU is a universal dentin bonding agent that contains Bis-GMA, HEMA, MDP, and ethanol. Thirty years ago, a dental manufacturer (Kuraray Noritake Dental Inc., Tokyo, Japan) incorporated 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) as a functional monomer in their dental adhesives. Researchers [37,38] noted that MDP-based adhesives could chemically bond to the hydroxyapatite crystals of dentin via the electrostatic interactions of ionic bonds formed with the calcium ions of the hydroxyapatite crystals, resulting in an insoluble MDP-calcium salt. Moreover, the phosphate groups in MDP form covalent bonds with the corresponding phosphate groups of hydroxyapatite crystals to form insoluble salts [37,38]. Recently, bonding of multimode adhesives to dentin in the etch-andrinse mode was found to rely on the infiltration of resin into exposed collagen fibril scaffolds in a process known as ‘micromechanical interlocking’. Furthermore, a true chemical bond was found to have formed due to the presence of the MDP functional monomer groups [39,40]. In 2013, Munoz et al. [41] evaluated μTBS and nanoleakage of universal adhesives that did or did not contain MDP via etch-and-rinse and self-etch strategies and found that universal adhesives that contained MDP applied in two different etching modes showed higher and more stable μTBS with reduced nanoleakage at the interfaces after 6 months of water storage [41]. The findings of the present study were correlated with those of Munoz et al. [41]. In the present study, the etch-and-rinse mode was chosen, and ABU was applied to the teeth as a dentin bonding agent. After the restoration and polishing procedures, the teeth were coated with ABU as a CSS. Therefore, teeth restored with EP had two applications of ABU, which induced a positive effect on microleakage, achieved substantial bonding to dentin and finally showed almost the lowest scores for both the occlusal and gingival walls compared with those of the EP Control group.
Conclusion
The superiority of a CQ-based bulk-fill composite resin to a RAP technologyTM-based composite resin was indicated in terms of microleakage.
Incorporating only a novel photoinitiator in a composite resin material may not be sufficient to overcome polymerization shrinkage and marginal leakage. The photoinitiator concentration is also crucial. Additionally, novel monomers are important factors that decrease the polymerization stresses, thereby preserving the marginal integrity.
Neither the surface sealant materials nor the dentin bonding agent could completely prevent dye penetration at the occlusal and gingival walls. However, they succeeded in reducing marginal microleakage. Therefore, these materials should be recommended to clinicians due to their success in reducing marginal microleakage.
Unfilled methacrylate-based resin was determined to be the most compatible surface sealant material with the CQ-based bulk-fill composite material. Numerically, CQ-based bulkfill composite resin and unfilled methacrylatebased resin have been a combination that prevents the highest marginal microleakage.
Universal dental adhesive was investigated as the most compatible dentin bonding agent as a surface sealant material with the RAP technologyTM-based composite material. The MDP content of the dentin bonding agent achieved substantial bonding to dentin tissue.
Acknowledgment
The authors would like to thank Dr. Nazmiye Donmez for evaluating the statistical analysis.
References
- Stein PS, Sullivan J, Haubenreich JE, et al. Composite resin in medicine and dentistry. J Long Term Eff Med Implants. 2005; 15:641-654.
- Schneider LF, Cavalcante LM, Silikas N. Shrinkage stresses generated during resin-composite applications: A Review. J Dent Biomech 2010; 2010:131630.
- Sadeghi M. The effect of fluid composite as gingival layer on microleakage of class II composite restorations. Dent Res J 2007; 4:40-47.
- Braga RR, Ballester RY, Ferracane JL. Factors involved in the development of polymerization shrinkage stress in resin composites: A systematic review. Dent Mater 2005; 21:962-970.
- Neumann MG, Miranda WG, Schmitt CC, et al. Molar extinction coefficients and the photon absorption efficiency of dental photoinitiators and light curing units. J Dent 2005; 33:525-532.
- Neumann MG, Schmitt CC, Ferreira GC, et al. The initiating radical yields and the efficiency of polymerization for various dental photoinitiators excited by different light curing units. Dent Mater 2006; 22:576-584.
- Bucuta S, Ilie N. Light transmittance and micro-mechanical properties of bulk fill vs. conventional resin based composites. Clin Oral Investig 2014; 18:1991-2000.
- Van Ende A, De Munck J, Van Landuyt KL, et al. Bulk-filling of high C-factor posterior cavities: Effect on adhesion to cavity-bottom dentin. Dent Mater 2013; 29:269-277.
- Furness A, Tadros MY, Looney SW, et al. Effect of bulk/incremental fill on internal gap formation of bulk-fill composites. J Dent 2014; 42:439-449.
- Al Sunbulh H, Silikas N, Watts DC. Polymerization shrinkage kinetics and shrinkage-stress in dental resin composite. Dent Mater 2016; 32:998-1006.
- Tiba A, Zeller GG, Estrich CG, et al. Laboratory evaluation of bulk-fill versus traditional multi-increment-fill resin-based composites. ADA Professional Product Review 2013; 8:13-17.
- http://www.tokuyama-dental.com/tdc/pdf/productsheet/EstelitePosterior-110907.pdf
- Perez CR, Hirata R, Silva AHMFT, et al. Effect of a glaze/composite sealant on the 3-D surface roughness of esthetic restorative materials. Oper Dent 2009; 34:674-680.
- Tjan A, Tan D. Microleakage at gingival margins of Class V composite resin restoration rebonded with various low viscosity resin systems. Quintessence Int 1992; 22:565-573.
- Hepdeniz OK, Temel UB, Ugurlu M, et al. The effect of surface sealants with different filler content on microleakage of class V resin composite restorations. Eur J Dent 2016; 10:163-169.
- Ramos RP, Chinelatti MA, Chimello DT, et al. Assessing microleakage in resin composite restorations rebonded with a surface sealant and three low-viscosity resin sysyems. Quintessence Int 2002; 33:450-456.
- dos Santos PH, Pavan S, Assuncao WG, et al. Influence of surface sealants on microleakage of composite resin restorations. J Dent Child 2008; 75:24-28.
- Schmid-Schwapa M, Graf A, Preinerstorfer A, et al. Microleakage after thermacycling of cemented crowns-A meta-analysis. Dent Mater 2011; 27:855-869.
- Zamboni SC, Nogueira L, Bottino MA, et al. The effect of mechanical loading on the cusp defection of premolars restored with direct and indirect techniques. J Contemp Dent Pract 2014; 15:75-81.
- Ozcan S, Yikilgan I, Bala O, et al. The effect of different liners on the microleakage of class II restorations after thermocycling and occlusal loading. Marmara Dent J 2013; 2:71-75.
- Hazra A, Gogtay N. Biostatistics series module 3: Comparing groups: Numerical variables. Indian J Dermatol 2016; 61:251–260.
- Ozel E, Soyman M. Effect of fiber nets, application techniques and flowable composites on microleakage and the effect of fiber nets on polymerization shrinkage in class II MOD cavities. Oper Dent 2009; 34:174-180.
- Ayyildiz S, Uyar A, Yuzugullu B. Microleakage and the evaluation methods in dentistry. J Dent Fac Ataturk Uni 2009; 19:219-226.
- Miyazaki M, Tsujimoto A, Tsubota K, et al. Important compositional characteristics in the clinical use of adhesive systems. J Oral Sci 2014; 56:1-9.
- D’Alpino PH, Pereira JC, Rueggeberg FA, et al. Efficacy of composite surface sealers in sealing cavosurface marginal gaps. J Dent 2006; 34:252-259.
- Olmez A, Oztas N, Bilici S. Microleakage of resin composite restorations with glass-ceramic inserts. Quintessence Int 1998; 29:725-729.
- Wiskott HW, Nochols JI, Belser UC. Stress fatigue: Basic principles and prosthodontic implications. Int J Prosthodontics 1989; 8:105-116.
- Bates J, Stafford G, Harrison A. Masticatory function-A review of the literature: The form of the masticatory cycle. J Oral Rehabil 1975; 2:281-301.
- Amirouche-Korichi A, Mouzali M, Watts DC. Effects of monomer ratios and highly radiopaque fillers on degree of conversion and shrinkage-strain of dental resin composites. Dent Mater 2009; 25:1411-1418.
- Arikawa H, Takahashi H, Kanie T, et al. Effect of various visible light photoinitiators on the polymerization and color of light-activated resins. Dent Mater J 2009; 28:454-460.
- Jiménez-Planas A, Martín J, Abalos C, et al. Developments in polymerization lamps. Quintessence Int 2008; 39:74-84.
- http://www.tokuyamadental.com/tdc/pdf/technicalreport/EFQ_and_EFQ_HF_TechnicalReport.pdf
- https://www.tokuyama-us.com/wp-content/uploads/resources/Technical-Report_ESQ-3.pdf
- https://www.ultradent.com/products/procedures/restorative/class-I-II-III-IV-composite restoration/curing-lights/valo-story
- Schneider LF, Consani S, Sakaguchi RL, et al. Alternative photoinitiator system reduces the rate of stress development without compromising the final properties of the dental composite. Dent Mater 2009; 25:566-572.
- Youn YH, Hyun HK, Kim YJ, et al. The effect of surface sealing on the microleakage of class V composite resin restorations. L Korean Acad Pediatr Dent 2007; 34:359-369.
- Yoshihara K, Yoshida Y, Hayakawa S, et al. Nanolayering of phosphoric acid ester monomer on enamel and dentin. Acta Biomater 2011; 7:3187-3195.
- Yoshida Y, Yoshihara K, Nagaoka N, et al. Self-assembled nano-layering at the adhesive interface. J Dent Res 2012; 91:376-381.
- De Munck J, Van Landuyt K, Peumans M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res 2005; 84:118-132.
- Taschner M, Nato F, Mazzoni A, et al. Influence of preliminary etching on the stability of bonds created by one-step self-etch bonding systems. Eur J Oral Sci 2012; 120:239-248.
- Muñoz MA, Luque I, Hass V, et al. Immediate bonding properties of universal adhesives to dentine. J Dent 2013; 41:404-411.
Author Info
Magrur Kazak*, Rabianur Yurdan, Nazmiye Donmez and Safiye Selin Koymen
1Department of Restorative Dentistry, School of Dental Medicine, Bahcesehir University, Istanbul, Turkey2Department of Restorative Dentistry, Bezmialem Vakif University, Istanbul, Turkey
Citation: Magrur Kazak, Rabianur Yurdan, Nazmiye Donmez, Safiye Selin Koymen, Marginal Microleakage of Composite Resin Materials Comprising Different Photo Initiators with Surface Sealants and Bonding Agent Application after Thermomechanical Aging, J Res Med Dent Sci, 2020, 8(1): 16-25.
Received: 17-Dec-2019 Accepted: 31-Dec-2019
