Research Article - (2019) Volume 7, Issue 1
Management of Fluid Therapy in Children
Meysam Chahkhoei1, Marziyeh Khalili2, Masoumeh Mohammadian Behbahani2, Somaye Ganjalivand3 and Soamyeh Bashti2*
*Correspondence: Soamyeh Bashti, Social Determinants of Health Research Center, Yasuj University of Medical Sciences, Iran, Email:
Abstract
Introduction and Objective: Pediatric venous nursing care is defined as the application of nursing process in relation to clinical care of children's venous fluid. Management of proper fluid therapy in children can facilitate the process of treatment. Considering this issue, conduct the researcher to this study with the aim of reviewing the management of fluid therapy in pediatric nursing.
Methods: All studies conducted during the years 2005-2017 using the keywords of fluid therapy, fluid therapy in, childrens fluid, serum, pediatric emergency, intravenous fluids from databases of the country and abroad, including magiran, SID, Medlib, CINHAL, PubMed, Scopus. Data were analyzed using meta-analysis.
Results: 20 studies were conducted to determine the management of fluid therapy in children. Ultimately, management of intravenous fluid therapy in children was discussed in disorders such as infectious diseases, burns, trauma, and icterus.
Conclusion: Selection of the type, time and volume of fluids received by the medical staff is very important, so further research in this area with conducting training classes for nurses suggested by the researcher to manage intravenous fluid therapy.
<Keywords
Intravenous therapy, Children, Pediatric emergency, Intravenous fluids
Introduction
Nurses working in medical centers in the current world are faced with a lot of responsibilities and tasks related to specialized skills [1]. They are responsive to providing all decisions and practices for health care at a safe and secure level [2]. The nurse is expected to work according to the framework of the law and the guidance of credible nursing lines, nursing processes, communication skills, and teaching or learning principles [3]. Also, Intravenous therapy is one of the main responsibilities of nurses in their daily functioning, because electrolyte disturbances are usually the most important reason parents bring children to health centers in search of health care services [4]. A large proportion of nursing errors and mistakes are reported in the area of serum reception, so according to studies, errors in the rate of serum reception were the most common types of errors and then errors in the volume and type of serum were the common mistakes of nurses in this area [5-7].
It seems that proper management of fluid therapy in children can facilitate many of these mistakes [8]. Also, there are very few studies in this field and attention to the above issues. So this study designed with the aim of reviewing the management of fluid therapy in pediatric nursing.
Method
In this review study, all studies conducted inside and outside of the Iran country during the years 2005-2017 by using of the keywords of fluid therapy, fluid therapy in children, fluid serum, pediatric emergency and intravenous fluids from the Iran information banks included Magiran -medlib -SID and Iran medex as well as Latin databases like CINHAL -Pubmed -Scopus. The data were analyzed using the meta-analysis method and the data of the selected articles were collected. All papers were reviewed regardless of place of the publication and manner of doing the work. After reviewing and collecting all the published articles, duplicate and non-related articles were removed. In the next step, the articles based on the criteria for entering the study, which included interventional studies in children was conducted. Exit criteria also included data from case reports and posters, conferences. All the necessary ethical issues for the correct use of the extracted articles and the standards for publishing the work were obtained.
Findings
After searching from databases, 220 articles of articles based on the title and abstract, were reviewed, which 193 articles were excluded because they did not examine the intravenous fluids in children? 27 articles in the area of treatment of fluid therapy were reviewed more closely. Finally, 20 articles were reviewed in this review (Figure 1).
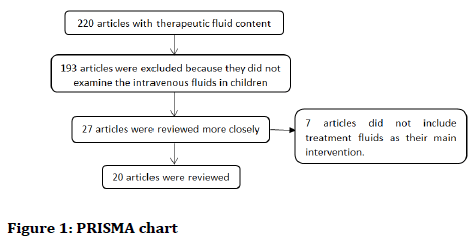
Figure 1. PRISMA chart
Ultimately, children management of intravenous fluid therapy was investigated in disorders such as infectious diseases, burns, trauma and icterus.
Discussion
Articles showed that the types of intravenous fluids in children are classified as follows:
1. Crystalloid solutions to compensate for the reduction of fluids or electrolytes, such as Ringer serum, Rinerglactate, Saline normal serum, Salty sugar serum (Table 1).
| Solution | Change in ICF | Change in ECF | Glucose [mg/dl] | Cl- [mmol/L] | Na+ [mmol/L] |
|---|---|---|---|---|---|
| Dextrose 5% | 667 mL | 333 mL | 5000 | 0 | 0 |
| 1/3, 2/3 & D/S | 444 mL | 556 mL | 3333 | 51 | 51 |
| Half-normal saline | 333 mL | 667 mL | 0 | 77 | 77 |
| Normal saline | 0 mL | 1000 mL | 0 | 154 | 154 |
| Ringer lactate | 100 mL | 900 mL | 0 | 109 | 130 |
Table 1: The combination of common crystalloids
2. Colloidal solutions to compensate for decreased intravascular volume such as Dextran and Homoxylate (Table 2)
| Modified gelatin serum [homaxle] | Dextran |
|---|---|
| Group therapy for this serum is a plasma substitute agent. This plasma substitute solution is used in cases of shock caused by reduced blood volume due to bleeding, burns, pancreatic inflammation, water loss and electrolytes due to vomiting and continuous diarrhea, adrenal gland and kidney disease, and diabetic coma. This serum is a vehicle solution for insulin and has not been reported for full use of this drug. | Group therapy for this serum is a substitute for blood plasma. Its compounds include dextrose or chlorine. Dextran 40 reduces the adhesion of erythrocytes and reduces blood density. This serum is used in the treatment of ailments caused by bleeding, burns and surgery, and the amount of prescription depends on the amount of fluid lost and the concentration of blood. Dextran should not be used in cases of pulmonary edema and in kidney patients. |
Table 2: Group therapy for homaxle and dextra
3. Dietary solutions [substitution of intravenous nutrition] such as Amino acid serum and Interalipid serum (Table 3, Explanation 1)
| Intralipid serum | Carbohydrate serum | Amino Acid Serum |
|---|---|---|
| Group therapy for this serum is a nutritional solution for intravenous feeding. These products are metabolized after being used as energy sources in the body. It also increases heat generation, reduces respiration and increases oxygen consumption. | Carbohydrates are sources of calories and the treatment group of this serum is a nutritional need. In temporary treatment of circulatory and shock insufficiency, when other plasma enhancement products are not available, kidney disease is used in cerebral edema. This serum may result in the reduction of B-group vitamins. | The treatment group of this serum is injectable and calories. The drug forms are amino acids 5% and 10%. Its compounds include essential and unnecessary amino acids, nitrogen and electrolytes. Simultaneous consumption of tetracycline amino acids may reduce the effects of protein-retaining effects. |
Table 3: Group therapy for intralipid, carbohydrate and amino acid serum
4. Solutions with specific therapeutic agents, such as serum Mannitol (decreased intracranial pressure, decreased intraocular pressure, and accelerated urinary excretion of salicylic acid, barbiturate and lithium, and prevention of renal damage caused by these drugs).
Explanation 1
Total parenteral nutrition (TPN), an injectable sterile solution containing protein, dextrose and fat along with electrolytes, vitamins, trace elements, and water was used for supportive nourishment in premature and at high risk infants.
Indications for intravenous feeding are similar in children and adults. If the gastrointestinal tract reduces a body calorie intake, it will be indicated by intravenous fluid. The major difference in the intravenous feeding of children from adults is one of the lower levels of reserve in children, and moreover, the daily calorie intake of children is higher than that of adults.
Causes of onset of intravenous feeding in children and infants include:
1. Gastrointestinal anomalies [such asfistulas, obstruction, atresia, and short stomach syndrome]
2. Recurrent and chronic diarrhea and inflammatory bowel disease
3. Malnutrition that oral nutrition does not require body calories
4. Patients who need to be NPO for a longer period [for example, after surgery] to supply calories in them
5. Premature infants
Some of the important points in intravenous nutrition are listed below in Tables 4-7.
| Neonate | Initial | Advancement | Goal |
|---|---|---|---|
| Term | 1.5-2 g/kg/d | 0.5-1 g/kg/d | 2-3 g/kg/d |
| ELBW | 1.5-2 g/kg/d | 0.5-1 g/kg/d | 3.5-4 g/kg/d |
| Septic, Hypoxic | 1 g/kg/d | 0.25-0.5 g/kg/d | 3-4 g/kg/d |
Table 4: The amount of amino acids needed
| Neonate | Initial | Advancement | Goal |
|---|---|---|---|
| Term | 1-2 g/kg/d | 0.5-1 g/kg/d | 3 g/kg/d |
| Preterm | 0.5 -1 g/kg/d | 0.25-1 g/kg/d | 3 g/kg/d |
| Hyper bilirubinemic | 0.5 g/kg/d | 0-0.5 g/kg/d | 1-2 g/kg/d |
| Sepsis | |||
| Severe respiratory distress |
Table 5: The amount of lipid needed
| Neonate | Initial | Increase By | Maximum |
|---|---|---|---|
| Full-Term [≥ 37 weeks] | 60-80 ml/kg/day | 10 ml/kg/day | 150 ml/kg/day |
| Pre-Term [28-36 weeks, ≥ 1000 gm] | 70-80 ml/kg/day | 10 ml/kg/day | 150 ml/kg/day |
| ELBW [23-27 weeks, <1000 gm] | 80-100 ml/kg/day | 10 ml/kg/day | 200 ml/kg/day |
Table 6: Calculation of the fluid needs for intravenous feeding
| In the following | At first | Measurement item |
|---|---|---|
| Daily | Daily | Weight |
| twice a week | At first | Round the head |
| Daily | Every shift | Intake & output |
| every week | First and every 3-1 days | Serum electrolytes, Bun/Cr |
| Every 1-2 weeks | First and if needed | Bili Direct and indirect |
| Every 1-2 weeks | At first | LFT |
Table 7: Time of feed
One of the important points in intravenous nutrition seems to be examination of the child at the time of feed and the calculation of the fluid needs, as summarized in Tables 6 and 7.
Control of urinary output is important for children management fluid therapy in the daily review. The urinary output is in children less than 30 kg/ml, 1-2 times per hour and in children over 30 kg, 0.5-1 ml/kg per hour. The ratio of urine output to the fluid should be about 7/7.
Maintenance fluid
How to calculate the preservative fluid in newborns and children of more age groups per hour and 24 hours, as well as in routine conditions and special cases and the factors affecting them is presented in Table 8.
| How to Calculate Maintenance fluid for children in 24 hours | How to calculate Maintenance fluid for children every hour | Maintenance fluid in certain cases | Maintenance fluid in the Neonate |
|---|---|---|---|
| Law 100-50-20 | Law 4-2-1 | ||
| 1. For ten kilograms per 24 hours: 100 cc per kilogram body weight | 1. For ten kilograms: 4 cc per kilogram body weight per hour | The temperature of each degree of 12% is increased to the preservative, and in opposite hypothermia | Serum preservative for the first day of infancy is 2-3 cc/kg/h |
| 2. The second ten kilograms: 50 cc/kg | 2. The second ten kilograms: 2 cc per kilogram of body weight | In meningitis and stroke, two thirds of the maintenance fluid is given | For the second and third days 4-5 cc/kg/h |
| 3. More than 20 kilos Weight: per kilo 20 cc | 3. More than 20 kg Weight: 1 cc/kg | The hypothyroidism is reduced by 10 to 25% and increased by 25-75% in hyperthyroidism | - |
Table 8: Maintenance fluid
The most common indications for intravenous fluid therapy in infected children were infectious diseases, burns, trauma and icterus respectively.
Infectious diseases
Infectious diseases are one of the most common diseases that affect children 6 months to 14 years of age. In numerous studies the effect of rapid serum therapy on reducing the incidence of hospitalization was studied [9-11].
In the study, which investigated the effect of crystalloid injections on the recovery of urinary tract infection in children aged 6 months to 12 years, it was concluded that extra fluid intake has a beneficial effect on the premature improvement of urinary tract and urinary odour, and therefore to improve urination and smell Urinary tract infection is recommended, but in other cases, such as abdominal pain and a negative urine culture time, it is not advisable to treat it with no effect [12].
Burning
In large burns [more than 15% in small children and more than 20% in older children and adults], these mediators cause systemic responses in addition to topical responses. In patients with large burns due to fluid leakage from the intestine to the interstitial environment, in the first 24 hours to 18 hours after the withdrawal of proteins, patients with hypotension [edema] and edema may be affected. It seems that, after controlling the airway, the correction of missed fluids is a priority for the victims, especially the burned children. Children are more vulnerable to dehydration due to adequate hysterectomy and lack of proper development of the homeostasis system. As a result, the volume of fluids should be carefully monitored.
Colloidal fluids are also given in the second 24 hours to maintain inoculate pressure and maintain intracoronary volume, and some experts have reported that adding colloidal fluids in the first 24 hours improves prognosis [13,14]. Also, the rate of fluid intake in children with burns should be carefully controlled [15-17].
Trauma
The most common cause of death in children is trauma due to bleeding and loss of blood. It seems that compensation for lost fluids after hemorrhage control is a priority of treatment. Ringer Lactate is one of the first line treatments in routine treatment in such emergency rooms. However, patient in a study [18], the effects of hypertonic saline were compared with rheological lactate in patients with trauma, at the start of treatment received 250 cc of hypertonic saline serum at 7.5% for 15 minutes, 250 drops per minute. Finally, it can be said that the use of limited volume hypertonic saline at the start of treatment for patients with traumatic hypovolemic shock reduces the amount of fluid intake and increases the rate of exiting from shock.
Icter
In several studies [19,20], the effect of intravenous fluids on neonatal jaundice has been studied. Due to the effect of the mechanism of the phototherapy converting, the bilirubin to the lumen of the rubin that is excreted in the urine and fluid therapy can facilitate the disposal of this substance by increasing the flow of urine. Therefore, fluid treatment as a direct contributing factor in reducing jaundice and preventing dehydration in the treatment process is very important.
Conclusion
Evidence of intravenous fluid therapy is very limited and the exact selection of the type, time and volume of fluids received will be ignored. Therefore, further research in this area, along with conducting training courses for nurses on the management of intravenous fluid therapy by the researcher is suggested.
References
- Hockenberry MJ, Wilson D, Rentfro AR, et al. Study guide for Wong's nursing care of infants and children-e-book. Elsevier Health Sciences 2018.
- Pillitteri A. Maternal & child health nursing: Care of the childbearing & childrearing family. Lippincott Williams & Wilkins 2010.
- Ball JE, Murrells T, Rafferty AM, et al. Care left undone during nursing shifts: Associations with workload and perceived quality of care. BMJ Qual Saf 2014; 23:116-25.
- You LM, Aiken LH, Sloane DM, et al. Hospital nursing, care quality, and patient satisfaction: Cross-sectional surveys of nurses and patients in hospitals in China and Europe. Int J Nurs Stud 2013; 50:154-61.
- Kampmeier T, Rehberg S, Ertmer C, et al. Evolution of fluid therapy. Best Pract Res Clin Anaesthesiol 2014; 28:207-16.
- Valentine SL, Sapru A, Higgerson RA, et al. Fluid balance in critically ill children with acute lung injury. Crit Care Med 2012; 40:2883.
- Mousavi M, Khalili H, Dashti-Khavidaki S, et al. Errors in fluid therapy in medical wards. Int J Clin Pharm 2012; 34:374-81.
- Dychter SS, Gold DA, Carson D, et al. Intravenous therapy: A review of complications and economic considerations of peripheral access. J Infus Nurs 2012; 35:84-91.
- Maitland K, Kiguli S, Opoka RO, et al. Mortality after fluid bolus in African children with severe infection. N Engl J Med 2011; 364:2483-95.
- Hatami G, Motamed N, Pak IH, et al. Effect of nebulized 3% hypertonic saline in the treatment of acute viral bronchiolitis in children. ISMJ 2015; 18:334-43.
- Moritz ML, Ayus JC. Improving intravenous fluid therapy in children with gastroenteritis. Pediatr Nephrol 2010; 25:1383-4.
- Usefi P, Siroos A, Drreh F, et al. Study of the effect of excess fluid [1.5 times the preservative] on the treatment of infection. Children's urine. J Ardabil Univ Med Sci 2008; 8:321-5.
- Guyette F, Suffoletto B, Castillo JL, et al. Prehospital serum lactate as a predictor of outcomes in trauma patients: A retrospective observational study. J Trauma Acute Care Surg 2011; 70:782-6.
- Hoste EA, Maitland K, Brudney CS, et al. Four phases of intravenous fluid therapy: A conceptual model. Br J Anaesth 2014; 113:740-7.
- Nguyen TJ, Thaller S. Psychological rehabilitation of pediatric burn patients. J Craniomaxillofac Surg 2008; 19:882-7.
- Kraft R, Herndon DN, Branski LK, et al. Optimized fluid management improves outcomes of pediatric burn patients. J Surg Res 2013; 181:121-8.
- Senel E, Yasti AC, Reis E, et al. Effects on mortality of changing trends in the management of burned children in Turkey: Eight years’ experience. Burns 2009; 35:372-7.
- Branski LK, Herndon DN, Byrd JF, et al. Transpulmonary thermodilution for hemodynamic measurements in severely burned children. Crit Care 2011; 15:R118.
- Turkman M, Afsharpayman SH, Matinzadeh KZ, et al. The effect of intravenous fluid therapy on the reduction of bilirubin concentration in neonatal icteric patients under phototherapy in Najmej hospital in 2002. Acta Medica Iranica 2006; 64:85-9.
- Saeidi R, Heydarian F, Fakehi V, et al. Role of intravenous extra fluid therapy in icteric neonates receiving phototherapy. Saudi Med J 2009; 30:1176-9.
Author Info
Meysam Chahkhoei1, Marziyeh Khalili2, Masoumeh Mohammadian Behbahani2, Somaye Ganjalivand3 and Soamyeh Bashti2*
1Department of Nursing, School of Nursing and Midwifery, Bam University of Medical Sciences, Bam, Iran2Social Determinants of Health Research Center, Yasuj University of Medical Sciences, Yasuj, Iran
3Hospital Research Development Committee, Bam University of Medical Sciences, Bam, Iran
Citation: Meysam Chahkhoei, Marziyeh Khalili, Masoumeh Mohammadian Behbahani, Somaye Ganjalivand, Soamyeh Bashti, Management of fluid therapy in children, J Res Med Dent Sci, 2019, 7(1): 47-51.
Received: 21-Dec-2018 Accepted: 04-Jan-2019
