Research Article - (2022) Volume 10, Issue 10
Malignant Otitis Externa: A Retrospective Analysis and Treatment Outcomes
MK Rajasekar, J Mohankumar* and KR Muralidharan
*Correspondence: Dr. J Mohankumar, Department of Otorhinolaryngology, Sree Balaji Medical College and Hospital, Chrompet, Chennai,Tamil Nadu, India, Email:
Abstract
Malignant otitis external or skull base osteomyelitis is an extremely rare but potentially fatal disease of the external auditory meatus which is seen among aged people, diabetic or immune compromised patients. The most common organism is Pseudomonas aeruginosa. The disease spreads to the invading surrounding soft tissues, bones and cartilage causing their necrosis and even spreading to the skull base and involving cranial nerves. It is a rare fatal disease especially when spread involves skull base. This is most commonly treated with anti-pseudomonas, third generation cephalosporins and local debridement of the wound. The pathology of the disease, clinical picture, diagnosis, management and the outcome has been discussed and reviewed. This article includes 5 series of cases presented to our ENT opd with ear pain and discharge for past 3 months.
Keywords
Malignant otitis, Immuno compromised patients, Osteomyelitis
Introduction
Toulmouche first identified moe or skull base osteomyelitis in 1838, and Chandler coined the term "malignant" in 1968. Pseudomonas aeruginosa is the most common cause, although it is more common in geriatrics with diabetes or immunocompromised status. MOE has also been linked to Staphylococcus aureus, proteus mirabilis and some fungi, such as Aspergillus niger [1,2].
Otalgia that last more than a month, chronic otorrhea, fever and cranial nerve involvement are mostly symptoms of the condition. Santorini's fissures cause the disease to start in the external auditory canal and spread to the skull base [3]. The seventh cranial nerve (facial) is the most commonly affected, but glossopharyngeal, vagus, accessory, or hypoglossal nerve involvements are however common. Parotitis, mastoiditis, jugular vein thrombosis, meningitis, and death may all complicate MOE. MOE may very well be diagnosed clinically as well as radiologically (Table 1) [4].
| Major Criteria (Obligatory) | Minor Criteria (Occasional) |
|---|---|
| Nocturnal Pain | Pseudomonas/s.aureus in culture |
| Purulent Otorrhoea | Diabetes mellitus |
| Edema | Old age |
| Granulation tissue in EAC | Cranial nerve involvement |
| Microabscesses (when operated) | Positive radiograph |
| Positive Technetium-99 (99 Tc) bone scan for failure of treatment after more than 1 week | Debilitating conditions |
Table 1: Diagnostic criteria of malignant otitis externa (Levenson’s criteria).
Materials and Methods
We came across five cases of malignant otitis external presented to ENT opd with severe otalgia, purulent otorrhoeal for 3 months. Based on a thorough history and clinical assessment, related inquiries such as culture and sensitivity of the discharge, as well as HRCT scans, were performed. Out of 5 cases, 2 patients had granulation tissue in external auditory canal, 2 patients had oedematous EAC with nocturnal pain and purulent otorrhoea and 1 patient developed facial palsy. All patients found to be diabetic and their sugar levels were controlled and all 5 patients were treated with intravenous antibiotic, antifungal and antibiotic ear drops, cauterisation with TCA, vinegar wash, antibiotic ear wick and regular aural toileting with ultrasonic physiotherapy for the TM joint. Patient’s symptoms improved with conservative management over a period of 1-3 months (Table 2 and Figures 1-5).
| Sl.no | Age | Sex | Nocturnal pain | Purulent discharge | Diabetes mellitus | Otoscopic findings | Pus c/s | Iv antibiotics | Tcacauterisation | Post treatment |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 52 | M | present | present | present | granulation tissue in eac | pseudomonas aeruginosa | piptaz | done | pain and dischrge reduced |
| 2 | 58 | M | present | present | present | odematous eac | mrsa coagulase negative | iv cipro | ____ | reduced |
| 3 | 48 | F | present | present | present | polyp in eac | pseudomonas aeruginosa | piptaz | done | reduced |
| 4 | 56 | F | present | present | present | granulation tissue in eac | s.aureus | amoxy clav | done | reduced |
| 5 | 49 | M | present | present | present | odematous eac | klebsiella | meropenam | ____ | reduced |
Table 2: Diagnostic tests of malignant otitis externa according to their age and sex.
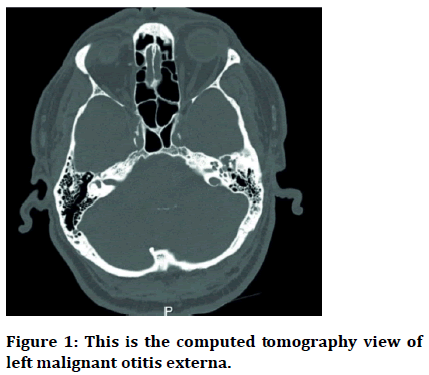
Figure 1: This is the computed tomography view of left malignant otitis externa.
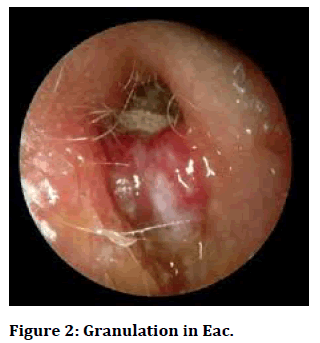
Figure 2: Granulation in Eac.
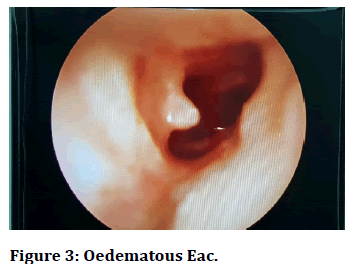
Figure 3: Oedematous Eac.
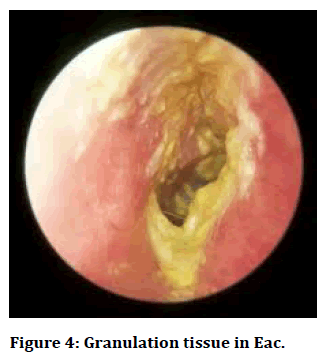
Figure 4: Granulation tissue in Eac.
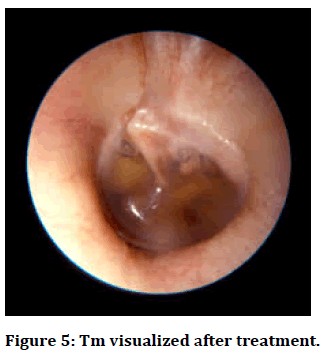
Figure 5: Tm visualized after treatment.
Discussion
A necrotizing infection of the EAC, temporal bone, and underlying soft tissue is known as malignant otitis external. Besides that, cranial nerve involvement can be linked to dysphagia, dysphonia, and facial paralysis. The most common sign of MOE is tragal tenderness, and the second most common symptom is purulent ear discharge [5].
Patients with diabetes are more likely to develop malignant otitis external. Micro angiopathy and impaired blood circulation in diabetic patients can play a key role in the pathogenesis of MOE, according to Rubin and Yu. Furthermore, elderly patients need more inpatient treatments and remain in hospitals for longer periods of time. Because of its proximity to the external auditory canal, the facial nerve is the most frequently affected cranial nerve. Patients with and without facial paralysis who were diagnosed with MOE were compared by Mani, et al. and Soudry, et al. and found no substantial difference in survival [6].
Pseudomonas aeruginosa is the most frequently isolated microbiological agent, according to most reports, and S. aureus is the other major microorganism involved to some degree. Patients with MOE may have elevated inflammatory markers such as ESR, white blood cell count, or CRP. As a result, ESR and CRP are useful laboratory markers for MOE screening. HRCT assesses the disease's anatomical spread through the base of the skull. As a result, early detection and care are critical. The prognosis seems to be directly linked to the stage of the disease at the time of treatment. This necessitates heightened understanding of the disease, with antipseudomonal antibiotics, primarily quinolones, and surgical debridement serving as the mainstay of care [7].
Relapse of the disease is a well-known feature of this condition, and it is normally marked by the onset of otalgia, accompanied by headache and temporomandibular joint pain With the development of powerful antipseudomonal antibiotics, the high mortality rate recorded in the early studies (37 percent by Chandler in 1977) has steadily decreased [3,8,9].
Conclusion
Skull base osteomyelitis is a necrotising disease that requires early diagnosis with prolonged antibiotic therapy, cauterisation with trichloroacetic acid, icthammolgycerin wick, antibiotic ear drops, vinegar wash, and physiotherapy usually proves successful. Poor prognosis is noticed in patients with uncontrolled diabetes and immune compromised patients.
References
- Rubin J, Yu VL. Malignant external otitis: insights into pathogenesis, clinical manifestations, diagnosis, and therapy. Am J Med 1988; 85:391-398.
[Crossref] [Googlescholar] [Indexed]
- Shavit SS, Soudry E, Hamzany Y, et al. Malignant external otitis: Factors predicting patient outcomes. Am J Otolaryngol 2016; 37:425–30.
[Crossref] [Googlescholar] [Indexed]
- Chandler JR. Malignant otitis externa. Laryngoscope. 1968; 78:1257-1294.
[Crossref] [Googlescholar] [Indexed]
- Nadol JB. Histopathology of Pseudomonas osteomyelitis of the temporal bone starting as malignant external otitis. Am J Otolaryngol 1980; 1:359-371.
[Crossref] [Googlescholar] [Indexed]
- Cohen D, Friedman P. The diagnostic criteria of malignant external otitis. J Laryngol Otol 1987; 101:216-221.
[Crossref] [Googlescholar] [Indexed]
- Mani N, Sudhoff H, Rajagopal S, et al. Cranial nerve involvement in malignant external otitis: Implications for clinical outcome. Laryngoscope 2007; 117:907-910.
- Strauss M, Aber RC, Conner GH, et al. Malignant external otitis: Long-term (months) antimicrobial therapy. Laryngoscope. 1982; 92:397-406.
[Crossref] [Googlescholar] [Indexed]
- Sylvester MJ, Sanghvi S, Patel VM, et al. Malignant otitis externa hospitalizations: Analysis of patient characteristics. Laryngoscope 2017; 127:2328-2336.
[Crossref] [Googlescholar] [Indexed]
- Soudry E, Joshua BZ, Sulkes J, et al. Characteristics and prognosis of malignant external otitis with facial paralysis. Arch Otolaryngol Head Neck Surg 2007; 133:1002-1004.
[Crossref] [Googlescholar] [Indexed]
Author Info
MK Rajasekar, J Mohankumar* and KR Muralidharan
Department of Otorhinolaryngology, Sree Balaji Medical College and Hospital, Chrompet, Chennai,Tamil Nadu, IndiaCitation: MK Rajasekar, J Mohankumar, KR Muralidharan, Malignant Otitis Externa: A Retrospective Analysis and Treatment Outcomes, J Res Med Dent Sci, 2022, 10 (10): 130-132.
Received: 05-Aug-2022, Manuscript No. JRMDS-22-41488; , Pre QC No. JRMDS-22-41488(PQ); Editor assigned: 08-Aug-2022, Pre QC No. JRMDS-22-41488(PQ); Reviewed: 22-Aug-2022, QC No. JRMDS-22-41488; Revised: 24-Oct-2022, Manuscript No. JRMDS-22-41488(R); Published: 31-Oct-2022
