Review Article - (2022) Volume 10, Issue 11
Low-Level Laser Therapy in Oral Maxillofacial Surgery
Rudra R Bharate1*, Bhushan Mundada2, Rahul Bhowate1 and Nitin Bhola2
*Correspondence: Rudra R Bharate, Department of Oral Medicine and Radiology, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Demmed to be University) Sawangi (Meghe) Wardha, Maharashtra, India, Email:
Abstract
One of the basic aims of dental treatment is to impart painless treatment for patients. Intra-operatively this aim it is very well managed by use of proper regional block with local anaesthesia and post-operatively it can be reduced by use of analgesics. Analgesics have its own disadvantage and side effects. To overcome this laser can be used in reduction of pain, swelling and inflammation and restore normal function. High dose of lasers causes side effect and proven to be harmful. To reduce these side effects Low-Level Laser Therapy (LLLT) is used.
Keywords
Low-level laser therapy, Oral maxillofacial surgery, LLLT
Introduction
The “LASER” is an acronym that stands for “light amplification by stimulated emission of radiation”. LLLT increase cell proliferation, collagen synthesis, fibroblast activity, growth factor release, and bleeding circulation, and accelerates the metabolism [1]. It is a gadget that generates light via an optical amplification process that relies on the stimulated emission of electromagnetic energy, and it emits coherent light. Low level laser therapy is also known as soft laser therapy, cold level laser therapy and photo-bio modulation. On the basis of number of interruptions and degree of severity, OSA is divided into three types.
The Laser can have both bio stimulatory and bio inhibitory effects on irradiated tissues, where each of them can have therapeutic applications. The diode laser has several unique characteristics for its use in dentistry such as low cost compared to other lasers, smaller size and easy application. The wavelength emitted by the device determines the effective depth of penetration. In deep tissue lesions application of wavelength greater than 800 nm penetrates deeper [2,3].
Implications of LLLT in oral maxillofacial surgery includes:
• Soft-tissue: Premalignant lesions, recurrent aphthous ulcer Recurrent Aphthous Stomatitis (RAS), Oral Submucosal Fibrosis (OSMF), oral Lichen Planus (LP), herpes simplex infections, periodontitis, dry socket, implant surgeries, endodontic surgeries.
• Hard-tissue: Impacted 3rd molar surgery, Temporomandibular disorders, implant osseointegration, dentin hypersensitivity, orthodontic tooth movement, bone grafting.
Literature Review
Therapy with radiation treatment or chemo radiotherapy causes intricacies in essentially all patients with cutting edge Head and Neck malignant growth (HNC) [4-6]. Organ conservation in HNC therapy is not generally viewed as inseparable from work protection, and the effects on personal satisfaction should be thought of while arranging disease therapy and expanding endurance [7-8]. LLLT has additionally been displayed to help in tissue recovery, aggravation decrease, and agony the board. One of the most well-known surgeries in oral medical procedure is the extraction of the third molar [9]. An incendiary stage much of the time emerges after careful injury, trailed by uneasiness, lockjaw and face edema. Physical techniques, for example, Low Level Laser Treatment (LLLT) have been displayed to give various advantages in decreasing enlarging, torment and advancing tissue recuperating, without unfavourable secondary effects in patients [10].
Mechanism
The Arndt-Schulz principle underpins low level laser therapy. If the stimulus is too faint, no effect is detected, according to this theory. To achieve optimal outcomes, the stimulation must be raised and the dose optimised, as increasing the dose further reduces the efficacy. Additional stimulus causes stimulation to be inhibited. LLLT regulates pathophysiological processes primarily through a non-thermal photo biological method in which laser light is absorbed by chromophores. Irradiation with monochromatic visible light in the blue, red, and far-red areas of the visible spectrum can improve metabolic activities in cells. The wavelengths and intensity of the light have an impact on the photo biological effects of stimulation. Bio-stimulation and photodynamic therapy are the main areas of action of LLLT (Figure 1) [11].
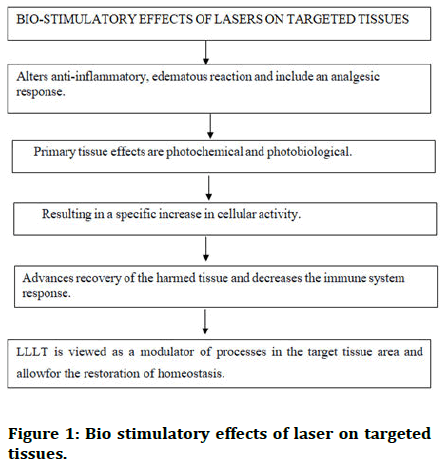
Figure 1: Bio stimulatory effects of laser on targeted tissues.
Bio-stimulation
Photodynamic therapy: The treatment of malignant neoplasia using Photo Dynamic Therapy (PDT) has been used for decades. It is based on a cytotoxic photochemical reaction. The photosensitizer absorbs the wavelength of the light source. Photo oxidation of organic materials underpins the photodynamic process. Cell death in tumour tissue as well as the death of infectious pathogens, is caused by localised creation of Reactive Oxygen Species (ROS) [12,13].
Properties of low power lasers
• The power output is 0.0001-0.1 Watts.
• The intensity is 0.01-10 W/cm2.
• The wavelength range is 300-10,600 nm.
• The pulse rate is 5,000 Hertz (cycles per second).
Principles of LLLT
• Regulatory effect: LLLT functions as a catalyst for endogenous, correct function restoration.
• Selectivity
• Individual variances in biological impacts are referred to as biologic effects.
• Energy density that is required.
Dosage for LLLT
Laser therapy has a wide therapeutic window; however, a reasonable dose is essential to trigger biological effects. High power density (MW per cm2) cannot compensate for low output, and deep laser therapy cannot compensate for gentle laser therapy.
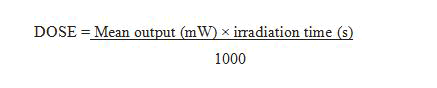
The majority of red and infrared LLLT utilizes mean laser yields of 10 to 100 MW and illumination seasons of 20 to 60 seconds, and does somewhere in the range of 0.6 and 9.6 J, and is just about as powerful as NSAIDs in decreasing irritation [14].
Dosage Principles
• Minimal response dose
• Time of irradiation/cm2 30 sec 3-4 min
• Power density: 1 MW/cm2
• Wavelength: 632-904 nm
LLLT equipment
Semiconductor diode lasers are small and efficient in converting electrical energy into laser energy. Simplex external circuitry can also be used to pulse the light at different frequencies.
An internal phototransistor is installed within the laser device's package to monitor the temperature or output of the laser diode. A typical diode lasers beam profile is rectangular, with high divergence along the long axis and low divergence along the short axis. This results in a sweep or significantly divergent oval profile. The integrated optics of a diode laser can produce a collimated and focussed light beam. A laser transmissive disposable barrier should be able to appropriately protect components that come into close contact with patients.
In terms of the optical risks, they represent to personnel and patients, LLLT laser units are commonly categorized as Class III or Class III b. The patient and the clinician must wear proper protective eyewear during therapy.
LLLT devices
Q 1000 soft laser: It is a low level laser device that is portable. It combines pulse laser light and infrared radiation to produce a consistent and regulated effect.
Lasers heal LH302: This laser has power ranging from 50-700 MW and wavelength 600-900 nm.
LC KMI unique: As a normal unit, this laser's source is a HeNe with wavelength of 632 nm. An optional far infrared heater with a power output of 300 W is also available.
LC KMI DY type: As a standard unit, this laser's source is a HeNe. Its wavelength is 632 nm and a power output of 15 MW 407-420 nm blue light lamp.
Physiological effects of LLLT
• Increase in angiogenesis and neovascularization.
• Collagen production.
• Increase muscle regeneration.
• Decrease in muscle atrophy.
• Increase Bone formation.
• Increase cartilage production.
• Increase nerve regeneration.
• Decrease in inflammation and edema.
Discussion
Implications of low level laser therapy
Soft tissue
Premalignant lesions: Premalignant sores of the oral mucosa incorporate leukoplakia, erythroplakia, OSMF, other oral injuries. Paners, et al. also, Vermey, et al. were quick to portray the utilization of a CO2 careful laser to treat a shallow oral mucosal injury in the oral depression. The CO2 laser administrated in central premalignant oral infection shows specific upper hands over regular careful extraction and cryotherapy [15]. The CO2 laser was viewed as a viable instrument for the treatment of premalignant sores of the oral mucosa. Lim et al. detailed that the utilization of KTP (Potassium Titanyl Phosphate) lasers for the treatment of oral Leukoplakia may bring about lower repeat rates than when utilizing CO2 lasers [16].
Recurrent aphthous ulcer or Recurrent Aphthous Stomatitis (RAS): In 1972, Stanley defined (RAS) as three distinct clinical variants [17]. Severe RAS, also known as periadenitis mucosa, necroticcarecurrens or Sutton's disease and herpetic form ulceration, which is characterized by repeated crops of numerous ulcers that can number in the hundreds. Effective specialists, fundamental and effective steroids, corticosteroids, burning, anti-toxins, oral washes containing dynamic chemicals and other helpful choices are accessible [18,19]. LLLT is being used to treat RAS because of its bio-modulation and analgesic benefits, which stimulate the healing process and provide quick pain relief without the use of excessive medication or side effects. According to various studies [20], using LLLT on a reoccurring aphthous ulcer resulted in faster healing and less discomfort. Therapeutic laser is ideal for promptly alleviating pain and functional impairment, which are the main causes of discomfort in RAS patients.
Oral lichen planus: T cells are involved in the pathophysiology of lichen planus, which is a mucocutaneous illness of uncertain cause [21]. Keratotic (white) and non keratotic (erosive/atrophic/ulcerative) oral lichen planus are two different types of oral lichen planus.
Corticosteroids, Griseofulvin, curcuminoid, Sulodexide, O xpentifylline, surgery, photochemotherapy and laser have all been used to treat oral lichen planus [22]. LLLT in oral LP reduces inflammation, relieves pain and promotes ulcer healing, according to several studies [23].
Herpes simplex infections: LLLT has demonstrated good therapeutic effects as a longer term suppression therapy, according to several studies [24,25]. Two clinical instances with recurrent labial herpes that were treated with LLLT were documented in one of the studies. Throughout the 17 month clinical follow up period after therapy, both patients remained symptom free [26]. Herpes labial is and herpetic gingiva stomatitis can also benefit from LLLT therapy.
Oral mucositis: It is one of the most dangerous side effects of several cancer treatments. Mucositis may affect any part of the digestive tract, although stomatitis, or mouth sores are the most common symptoms of oral mucositis. It was carried out with red and infrared wavelength diode lasers. The epithelium's surface layer can be affected by shorter wavelengths (632.8–660 nm), whereas longer wavelengths penetrate deeper into the epithelium and affect sub-epithelial tissues. The red laser is absorbed in the surface layer of the oral mucosa, which promotes wound healing [27].
Periodontitis: It is one of the most prevalent disorders of the tooth's attachment and, in its late stages, is the leading cause of tooth loss. Based on histological results, Obradovic, et al. found that when periodontal disease patients were treated with LLLT (670 nm) in addition to traditional periodontal therapy, healing and collagenization and homogenization in the gingival lamina propria improved [28].
Dry socket: As per blum dry attachment is characterized as "postoperative inconvenience at and around the extraction site that deteriorates somewhere in the range of 1 and 3 days following the extraction, followed with a somewhat or totally broke down blood cluster inside the alveolar attachment, with or without halitosis" [29]. Water system of the attachment and curettage ought to be acted in a totally dry climate. Extra medicines like LLLT, zinc oxide eugenol or plasma containing a ton of zinc. In torment abatement, development factors were more compelling just as the recuperating of the alveolar mucosa.
Hard tissue
Temporomandibular disorders: LLLT is an alternative for the treatment of TMD due to its simplicity of application, short treatment period, and few contraindications. As a result, it is a safe and non-invasive therapy option for TMDs. LLLT reduces pain and improves health in patients with temporomandibular or zygapophyseal joint abnormalities when used within a recommended dose range [30].
Bone grafting: Garcia I, et al. discovered that combining LLLT with autogenously bone successfully encouraged bone growth.
Impacted 3rd molar surgery: The most common surgical treatment in oral maxillofacial surgery is the extraction of an impacted third molar. It is a small surgical treatment performed primarily under local anaesthetic, with varying degrees of difficulty depending on the tooth's position. Postoperative complaints by the patient are pain, swelling, limited opening of the mouth, and hypoesthesia. Several techniques have also been explored to prevent these problems, one of which is the application of LLLT. LLLT extra orally had a significantly positive effect on trismus and swelling [31-34].
Advantages of LLLT
• The laser's power can be adjusted, as well as the mode of application and the duration of the application.
• It is a non-invasive procedure hence it does not require a surgical incision.
• Injured soft and hard tissues heal more quickly.
• Minimizes bleeding or blood loss.
• At times, minimizes or eliminates the need for anaesthesia (however, this depends on the clinical procedure).
• Bacterial decontamination of root canal systems and deep periodontal pockets.
• Assists in the regeneration of the Periodontal Ligament (PDL).
• Hard tissue repair is easier and more comfortable for patients.
• Because there is no contact, the performance is aseptic and atraumatic.
• Quick, painless, and precise application.
• Treatment time is limited.
• Analgesic, antiphlogistic, and wound-healing stimulatory effects are all present at the same time.
• Laser therapy does not necessitate the use of any drugs.
Disadvantages of LLLT
• Occasionally, separate device is required in getting the beam onto area to be treated.
• Objective factors are typically difficult to regulate when it comes to treatment results [35].
Factors affecting efficacy of LLLT
Patient selection factors
• Anaesthesia
• Length of follow up
• Inclusion of controls
• Standardized clinical presentation
• Optimal ‘window’ for the timing of treatment
Optical factors
• Wavelength
• Spot size
• Laser or LED light source
• Power density
• Energy density
• Mode of operation
• Timing of treatment
Conclusion
LLLT can be used as a supplementary treatment in a variety of dental situations. It has a positive impact on the hard and soft tissues of the oral cavity while having a minimal negative impact. Future LLLT studies in dentistry will need to use standardized, revealed outcomes. The effectiveness of LLLT should also be investigated in terms of wavelength, treatment length, and dosage.
LLLT is a developing field of science. With each passing day, more is understood about laser therapy's mechanics, doses, treatment sites, and illnesses that lasers can treat. To accomplish the various techniques in a fair amount of time while adhering to cross-infection control regulations, improvements in the design of LLLT equipment are required. LLLT applications have a bright future because of their low tech, low cost qualities. To achieve the standardization of treatment procedures, the goal should be to figure out the precise dosimeter required for therapeutic laser effects.
LLLT can assist the osseointegration of implants. It improves the initial contact between the bone and implant, increases the proliferation and adhesion of osteoblasts to the implant surface, enhances the content of calcium and promotes angiogenesis in bone tissue.
LLLT increases the local microcirculation and has a positive bio-modulatory effect on bone tissue repair. It improves the collagen fibre deposition and the amount of well-organized bone trabeculae at an early stage. Garcia et al. in their study reported that the use of LLLT with autogenous bone effectively stimulated bone formation in critical size defects in the calvarias of immunosuppressed rats.
The mode of action of LLLT on the inflammatory process during orthodontic treatment is by vasodilatation and induction of degranulation of mast cells, with the release of pro-inflammatory substances to accelerate tissue healing. LLLT also increases osteoblastic and osteoclastic activity and stimulates collagen production. Genc, et al. reported that low level laser could significantly accelerate orthodontic tooth movement in humans.
References
- Demirkol N, Sari F, Bulbul M, et al. Effectiveness of occlusal splints and low-level laser therapy on myofascial pain. Lasers Med Sci 2015; 30:1007-1012.
- Walsh LJ. The current status of low-level laser therapy in dentistry, Part 1 Soft tissue applications. Aust Dent J 1997; 42:247-254.
- Fávaro–Pípi E, Ribeiro DA, Ribeiro JU, et al. Low-level laser therapy induces differential expression of osteogenic genes during bone repair in rats. Photo Med Laser Surg 2011; 29:311-317.
- Sol Silverman MA. Oral cancer: Complications of therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 88:122-126.
- Madhumathi D, Kumar MP. Low-level laser therapy in oral and maxillofacial surgery-A review. Drug Invent Today 2018; 10.
- Walsh LJ. Dental lasers: Some basic principles. Postgrad Dent 1994; 4:26-29.
- Zell JA, Cinar P, Mobasher M, et al. Survival for patients with invasive cutaneous melanoma among ethnic groups: the effects of socioeconomic status and treatment. J Clin Oncol 2008; 26: 66-75.
- Van der Molen L, van Rossum MA, Burkhead LM, et al. Functional outcomes and rehabilitation strategies in patients treated with chemoradiotherapy for advanced head and neck cancer: A systematic review. Eur Arch Oto Rhino Laryngol 2009; 266:889-900.
- Sato FR, Asprino L, de Araujo DE, et al. Short-term outcome of postoperative patient recovery perception after surgical removal of third molars. J Oral Maxillofac Surg 2009; 67:1083-1091.
- Colorado-Bonnin M, Valmaseda-Castellon E, Berini-Aytes L, et al. Quality of life following lower third molar removal. Int J Oral Maxillofac Surg 2006; 35:343-347.
[Crossref] [Googlescholar][Indexed]
- Goyal M, Makkar S, Pasricha S. Low level laser therapy in dentistry. Int J Laser Dent 2013; 3:82-88.
- Karu TI. Multiple roles of cytochrome c oxidase in mammalian cells under action of red and IR-A radiation. IUBMB Life 2010; 62:607-610.
- Karu TI. Molecular mechanism of the therapeutic effect of low-intensity laser radiation. Lasers Life Sci 1988; 2:53-74.
- Bjordal JM, Lopes-Martins RA, Joensen J, et al. The anti-inflammatory mechanism of low level laser therapy and its relevance for clinical use in physiotherapy. Phys Ther Rev 2010; 15:286-293.
- Flynn MB, White M, Tabah RJ. Use of carbon dioxide laser for the treatment of premalignant lesions of the oral mucosa. J Surg Oncol 1988; 37:232-234.
- Lim B, Smith A, Chandu A. Treatment of oral leukoplakia with carbon dioxide and potassium-titanyl phosphate lasers: A comparison. J Oral Maxillofac Surg 2010; 68:597-601.
- Preeti L, Magesh KT, Rajkumar K, et al. Recurrent aphthous stomatitis. J Oral Maxillofac Pathol 2011; 15:252.
- Natah SS, Konttinen YT, Enattah NS, et al. Recurrent aphthous ulcers today: A review of the growing knowledge. Int J Oral Maxillofac Surg 2004; 33:221-234.
- Horch HH, Gerlach KL. CO2 laser treatment of oral dysplastic precancerous lesions: a preliminary report. Lasers Surg Med 1982; 2:179-185.
- Anand V, Gulati M, Govila V, et al. Low level laser therapy in the treatment of aphthous ulcer. Indian J Dent Res 2013; 24:267.
- Al-Hashimi I, Schifter M, Lockhart PB, et al. Oral lichen planus and oral lichenoid lesions: diagnostic and therapeutic considerations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103:e1-12.
- Conrotto D, Carbone M, Carrozzo M, et al. Ciclosporin vs. clobetasol in the topical management of atrophic and erosive oral lichen planus: A double blind, randomized controlled trial. Br J Dermatol 2006; 154:139-145.
- Jajarm HH, Falaki F, Mahdavi O. A comparative pilot study of low intensity laser versus topical corticosteroids in the treatment of erosive atrophic oral lichen planus. Photomed Laser Surg 2011; 29:421-425.
- Wutzler P, Doerr HW, Farber I, et al. Seroprevalence of herpes simplex virus Type 1 and Type 2 in selected German populations relevance for the incidence of genital herpes. J Med Virol 2000; 61:201-207.
- Wulandari EA, Subita GP. Diagnosis and management of recurrent herpetiform stomatitis and Behçet syndrome like recurrent aphthous stomatitis herpetiform type. Padjadjaran J Dent 2008; 20.
- Ferreira DC, Reis HL, Cavalcante FS, et al. Recurrent herpes simplex infections: laser therapy as a potential tool for long-term successful treatment. Rev Soc Bras Med Trop 2011; 44:397-399.
- Fekrazad R, Chiniforush N. Oral mucositis prevention and management by therapeutic laser in head and neck cancers. J Lasers Med Sci 2014; 5:1.
- Obradovic R, Kesic L, Mihailovic D, et al. A histological evaluation of a low-level laser therapy as an adjunct to periodontal therapy in patients with diabetes mellitus. Lasers Med Sci 2013; 28:19-24.
- Taberner-Vallverdu M, Nazir M, Sanchez-Garces MA, et al. Efficacy of different methods used for dry socket management: A systematic review. Med Oral Patol Oral Cir Bucal 2015; 20:e633.
- Agrawal N, Dangore S, Bhowate R, et al. Comparative efficacy of laser and topical corticosteroid in the management of aphthous stomatitis. J Datta Meghe Inst Med Sci Univ 2019; 14:155.
- Baid R, Rathi N, Jain SA, et al. Comparison of Effectiveness of Diode Laser with Er: Yag Laser on Fluoride Uptake of Enamel Surface Using Acidic and Neutral Topical Fluorides: An in vitro Study. Int J Cur Res Rev 2021; 13:168.
- Chaudhari PS, Chandak MG, Relan KN, et al. Lasers in diagnosis, interception and management of white spot lesions and dental caries-A review. J Evol Med Dent Sci 2021; 10:624-632.
- Singh AL, Chandak M, Ghatge A, et al. study of efficacy of diode laser in unwanted facial hair: dynamic versus static mode. Int J Pharm Res 2021; 33:267–272.
- Bjordal JM, Couppe C, Chow RT, et al. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother 2003; 49:107-116.
- Garcia VG, Sahyon AS, Longo M, et al. Effect of LLLT on autogenous bone grafts in the repair of critical size defects in the calvaria of immunosuppressed rats. J Craniomaxillofac Surg 2014; 42:1196-1202.
Author Info
Rudra R Bharate1*, Bhushan Mundada2, Rahul Bhowate1 and Nitin Bhola2
1Department of Oral Medicine and Radiology, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Demmed to be University) Sawangi (Meghe) Wardha, Maharashtra, India2Department of Oral and Maxillofacial Surgery, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Demmed to be University) Sawangi (Meghe) Wardha, Maharashtra, India
Citation: Rudra R Bharate, Bhushan Mundada, Rahul Bhowate, Nitin Bhola, Low-Level Laser Therapy in Oral Maxillofacial Surgery, J Res Med Dent Sci, 2022, 10 (11): 039-044.
Received: 29-Aug-2022, Manuscript No. JRMDS-22-47956; , Pre QC No. JRMDS-22-47956(PQ); Editor assigned: 01-Sep-2022, Pre QC No. JRMDS-22-47956(PQ); Reviewed: 15-Sep-2022, QC No. JRMDS-22-47956; Revised: 31-Oct-2022, Manuscript No. JRMDS-22-47956(R); Published: 08-Nov-2022
