Research - (2022) Volume 10, Issue 8
Lap Retroperitoneal Pyelolithotomy vs. Percutaneous Nephrolithotomy-or Pelvic Stone Management
Naveed Khan1*, Mohd Tafazul1, Farah Mushtaq2, Mohamad Ommid2 and Muneer Khan1
*Correspondence: Naveed Khan, Department of Urology, Kidney Hospital, India, Email:
Abstract
Objective: To evaluate surgical outcomes of laparoscopic Retroperitoneal Pyelolithotomy (LRP) and Percutaneous Nephrolithotomy (PCNL) in management of isolated pelvic calculus. Material and methods: From February 2004 to December 2011, 30 patients underwent LRP and 30 underwent PCNL for treatment of pelvic stone. Differences in demographics, perioperative data, and complications were compared between LRP and PCNL patients. Results: Stone-free rates were 100 and 93.3% in the LRP and PCNL groups respectively (p=0.003). Mean operation time was significantly longer in the LRP group (p<.001) as compared to the PCNL group. In terms of blood transfusion, drain removal time, ureteral stent removal, and VAS scores, both groups were comparable with each other with no statistically significant difference(p>0.05). Hospital stay, loss of active days of work, cost of treatment were in favour of PCNL. Conclusion: Laparoscopic Retroperitoneal Pyelolithotomy is a safer but technically demanding alternative to PCNL which gives complete stone clearance in a single sitting with minimal bleeding risk and violation of the renal parenchyma.
Keywords
Laparoscopic retroperitoneal pyelolithotomy, Percutaneous nephrolithotomy, Hydronephrosis, Shock wave lithotripsy, Retrograde intrarenal surgery, Bleeding, Ureteral stent, Nephrostomy
Introduction
Renal stone prevalence in the world is increasing globally with advancement of diagnostic modalities and their amplified accuracy [1]. Traditionally renal pelvic calculi were managed with open pyelolithotomy, however, with the advancement of techniques and newer modalities, the management of such pelvic calculi have seen an immense change leading to better results with improved aesthetics and lesser morbidity [2,3].
Techniques such as Percutaneous Nephrolithotomy (PCNL) and RIRS are the mainstay modalities for the management of pelvic calculus but in certain cases of large pelvic calculus with extra renal pelvis, Laparoscopic pyelolithotomy can be a reasonable alternative [4]. In our prospective trial we compare retroperitoneal laparoscopic pyelolithotomy with PCNL. We believe that retroperitoneal laparoscopic pyelolithotomy is a better procedure for large pelvic calculus with an extra renal pelvis in terms of bleeding, operative time, and stone clearance.
SWL is not recommended for large >2 cm pelvic calculus, RIRS and PCNL are the mainstay procedures. Ideal procedure would be the one that achieves complete clearance with minimal morbidity and least number of procedures. Lap pyelolithotomy can remove stones integrally with lesser morbidity, less chance of bleeding and sepsis. Therefore, in this study we evaluated the role of laparoscopic pyelolithotomy by the retroperitoneal route and compared it with PCNL.
Material and Methods
Patient recruitment
This prospective study was carried out at Kidney Hospital, Srinagar, J&K between 20th June 2011 till 20th June 2013. Sixty patients with isolated pelvic calculus (2 cm) were included in the study. Written well informed consent was taken from all the patients and they were randomly allocated into two groups. Patients who were previously operated on the same side, patients with coagulopathy, positive urine culture, associated calyceal or ureteric calculus were excluded from the study.
Baseline screening and investigations
Patients were screened initially with USG to confirm the diagnosis. On admission a detailed history and clinical examination were undertaken in all patients. Baseline investigations such as CBC, serum biochemistry, coagulogram, urine R/E, and Urine culture were done. To define stone size (largest stone diameter), location of stone and pelvicalyceal anatomy CT urography was advised in all patients (Figure 1).
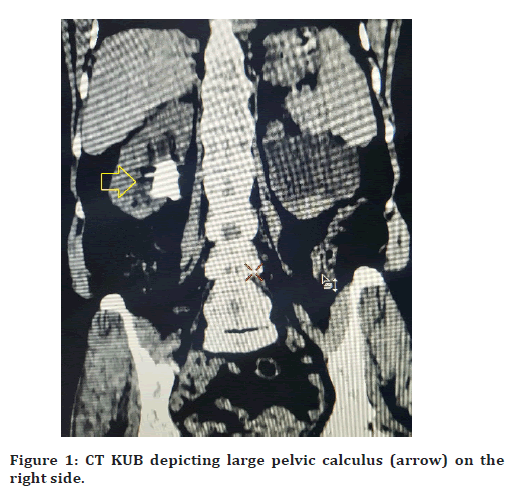
Figure 1. CT KUB depicting large pelvic calculus (arrow) on the right side.
LRP
Patient was placed in supine position for intravenous line, induction, endotracheal tube, and urinary catheter placement. Patient position was then changed to lateral decubitus depending on the side to be operated with hyperextension. A 15mm incision was made 1 cm below the tip of the 12th rib in the anterior axillary line and an opening was made in the lumbodorsal fascia with the use of a long artery forceps. The retroperitoneal space was dissected using blunt finger dissection and peritoneum was separated anteriorly using finger sweeping motion. The working space was expanded using a balloon dissector (PDB) which was filled upto 400-600 ml of air and kept for 5 min to achieve hemostasis.
The balloon was then deflated, withdrawn, and under finger guidance two ports were created one 10 mm and other 5mm. The ports were placed depending on the side to be operated as 10mm port is usually placed as the working port. The locations were one at the renal angle marked by the 12th rib and the lateral border of sacrospinalis muscle confluence and the other around 2 cm above the anterior superior iliac spine. A Hassan trocar was placed at the primary port which was used as the camera port. Additional 5 mm port was placed as required (Figure 2).
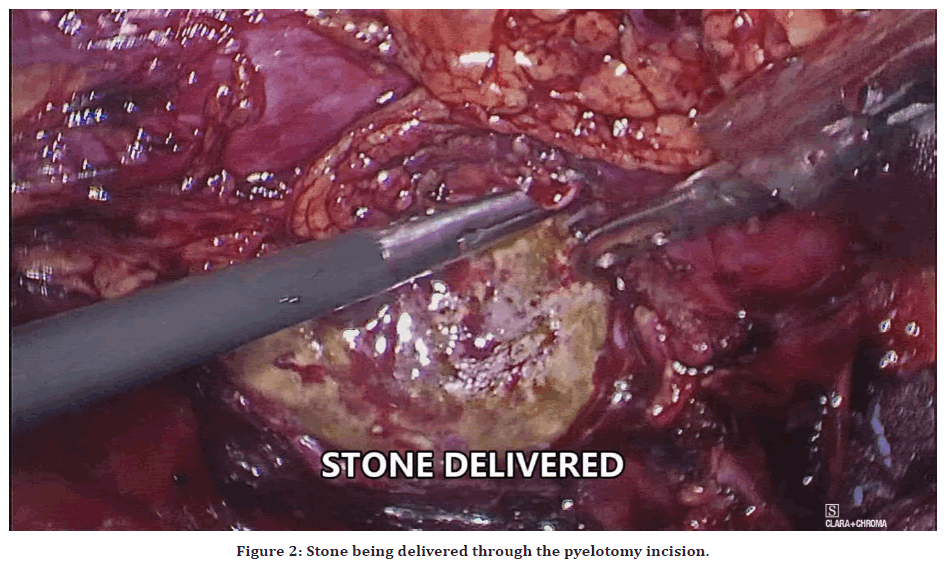
Figure 2. Stone being delivered through the pyelotomy incision.
The first step was the identification of the psoas muscle after which the ureter was identified just above and medial to the psoas tendon. The ureter was then traced upto the pelvis. Pyelotomy was made using an Endo knife which was extended by the use of endo scissors. The stone was dislodged and retrieved using cup forceps and the pelvis was then thoroughly irrigated. DJ stent was then placed across. The Pyelotomy was closed using 4 O polyglactin sutures. A drain was kept and the post sites were closed back (Figures 3 and 4).
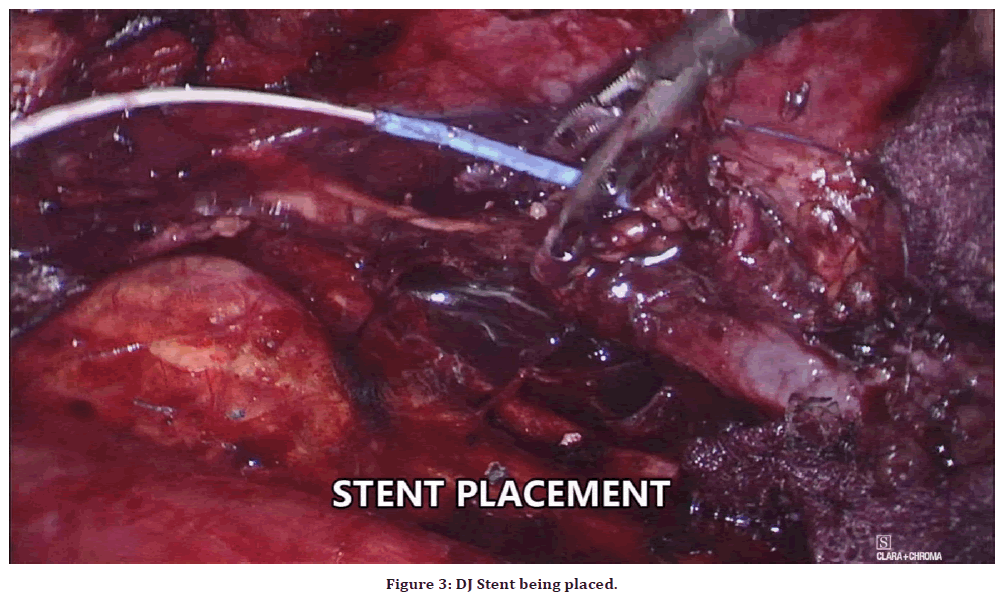
Figure 3. DJ Stent being placed.
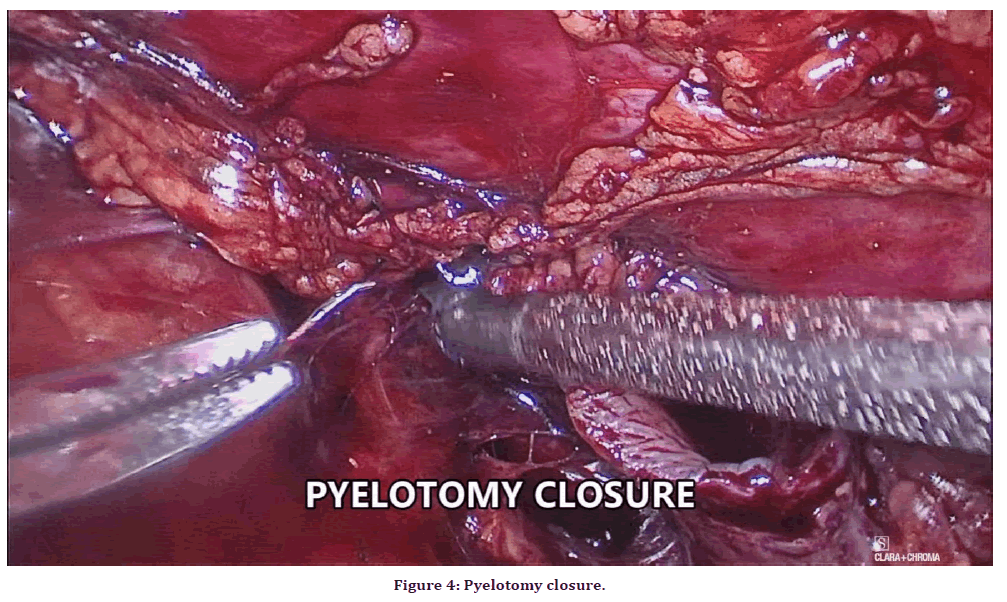
Figure 4. Pyelotomy closure.
PCNL
PCNL was performed in standard prone position. Under C arm guidance posterior calyceal puncture was made using 18-gauge puncture needle, tract was dilated upto 30 Fr and stone broken down using lithotripsy and fragments retrieved with forceps. Stent and nephrostomy were placed at the end.
In the LRP group catheter was removed on first post op day and drain was removed when the output was < 50 ml.
In PCNL group catheter removal on day one followed by nephrostomy removal after 6 hrs. was done.
Patients were followed after 1wk, 4 weeks, 3 months, and 6 months. The two groups were compared.
Statistical analysis
All data were entered in Microsoft excel sheet and was subjected to statistical analysis by SPSS version 21. Continuous variables were expressed as mean ± SD and categorical variables were expressed as frequency (%). Different variables between the two groups were compared by student t test. P values less than 0.05 were considered to be significant.
Results
As listed in Table 1 both groups were comparable based on age, gender, stone size, laterality, and grade of hydronephrosis.
| Variable | Laparoscopic Retroperitoneal Pyelolithotomy | Percutaneous Nephrolithotomy | P value | ||
|---|---|---|---|---|---|
| Age | 38.03 ± 18.47 | 39.90 ± 12.58 | 0.649 | ||
| Gender | Male | 20 | 17 | ||
| Female | 10 | 13 | |||
| Stone size (mm) | 19.42 ± 7.20 | 21.64 ± 7.44 | 0.247 | ||
| Laterality | Left | 16 | 13 | 0.438 | |
| Right | 14 | 17 | |||
| Hydronephrosis | Grade I | 16 | 19 | 0.296 | |
| Grade II | 9 | 10 | |||
| Grade III | 5 | 1 | |||
| Operative time (min) | 61.6 ± 26.36 | 49.7 ± 17.36 | 0.044 | ||
| Stone clearance | 30 (100 %) | 28 (93.3 %) | 2 (6.6%) | ||
| Hospital stay (days) | 4.73 ± 2.62 | 3.60 ± 1.47 | 0.044 | ||
| Cost of treatment (Rupees) | 42600 ± 3937.87 | 40900 ± 2214.37 | 0.044 | ||
| Loss of active days of work | 7.30 ± 4.51 | 4.90 ± 2.45 | 0.044 | ||
| Blood transfusion | 0 | 2 | 0.492 | ||
| Drain removal (days) | 2.60 ± 1.24 | 1.30 ± 0.66 | 0.001 | ||
| Ureteral stent removal (weeks) | < 4 wks | 29 | 30 | 1 | |
| > 4 wks | 1 | 0 | |||
| VAS score | 2 | 5 | 12 | ||
| 3 | 24 | 15 | |||
| 4 | 1 | 3 | |||
| Open conversion | 0 | 0 | |||
Table 1: Preoperative and post-operative variables.
A statistically significant difference was seen in the operative time, hospital stay, cost of treatment, loss of active days of work, and drain removal time between the groups. Stone free rate was 100 % in LRP group while it was 93.3% in the PCNL group.
Blood transfusion was required in none of the patients in the LRP group; however, 2 patients required blood transfusion in the PCNL group. Ureteral stents were removed within 4 weeks in all patients except 1 in the LRP group. No open conversion was seen in our series of patients. VAS scores were also analyzed among the two groups and were depicted in the Table 1. No complications were seen in 23 patients in the LRP group and in 26 patients in the PCNL group. The observed complications are listed in Table 2.
| Complications | Laparoscopic Retroperitoneal Pyelolithotomy | Percutaneous Nephrolithotomy |
|---|---|---|
| Fever | 1 | 1 |
| Haematuria | 1 | 3 |
| Inadvertent peritoneal entry | 4 | 0 |
| Surgical emphysema | 1 | 0 |
| Urinary leak | 0 | 0 |
| hematoma | 0 | 0 |
| No complication | 23 | 26 |
Table 2: List of complications observed in the two groups.
Discussion
The management of renal pelvic calculus largely depends on the size and the hardness of the stone. Traditionally, SWL, RIRS,and PCNL are the modalities used in the management of renal pelvic calculus. Open pyelolithotomy has become an obsolete procedure with the advent of newer technology but its minimal invasive alterative in the form of LRP may still have a role in cases of large renal calculus which can be dealt in a single sitting as compared to staging required by other procedures. LRP is a technically advanced procedure and is rarely adopted by people due to its longer learning curve. In this study we aimed to evaluate the utility of two modalities (LRP and PCNL) and have drawn inference on which technique to be adopted in which circumstances.
In the study, parameters like age, sex, stone size, grade of hydronephrosis, and laterality were comparable between the groups.
In terms of operative time, longer times were seen with the LRP group which can be due to creation of space, intracorporeal suturing, and stent placement.
Stone clearance was 100% with LRP group while in PCNL group it was 93%. This is the major advantage of LRP as in this the stone is extracted completely leading to complete clearance. Similar observations were reported by other authors [4-10].
In terms of blood transfusion, drain removal of time, ureteral stent removal, and VAS scores both groups were comparable with each other. No transfusion was required in LRP but it was required in 2 patients in the PCNL group. Consistent with the findings of the present study, Adel et al, have also reported similar findings [5].
The length of hospital stay, loss of active days of work, and cost of treatment were favorable in the PCNL group as compared to the LRP group. Cost is a variable factor as the cost in our series was increased due to the use of specialized gadgets (Thunder beat) and HD monitors. This cost can be decreased if simple gadgets like cautery hook are used.
Major limitation of the study was the size of the stone, with increasing size the efficacy of LRP will increase as the stone is removed in total and in a single stage while in PCNL the larger the stone more is the time taken, bleeding and need of staging the procedure. Also, in LRP there is no puncture of the renal parenchyma and no nephron loss which was not measured in the study. Further in specialized situation in concurrent UPJ obstruction, ectopic kidneys with stones and in solitary kidney LRP may be a better alternative.
Conclusion
LRP is a safer but technically demanding alternative to PCNL which gives complete stone clearance in a single sitting and with minimal bleeding risk and no violation of the renal parenchyma. Also, it can be adopted by trained surgeons in remote places where there are no facilities of C arm or blood bank. However, this technique should be performed by appropriately skilled surgeons to provide the benefit of this minimal invasive technique for patient care.
References
- Norlin A, Lindell B, Granberg PO, et al. Urolithiasis: A study of its frequency. Scand J Urol Nephrol 1976; 10:150-153.
- Gaur DD, Agarwal DK, Purohit KC, et al. Retroperitoneal laparoscopic pyelolithotomy. J Urol 1994; 151:927-929.
- Agarwal K, Agrawal MS. Place of percutaneous nephrolithotripsy (PCNL) in the management of renal calculi. Sri Lanka J Surg 2014; 31:41-47.
- Singh V, Sinha RJ, Gupta DK, et al. Prospective randomized comparison of retroperitoneoscopic pyelolithotomy versus percutaneous nephrolithotomy for solitary large pelvic kidney stones. Urol Int 2014; 92:392-395.
- Al-Hunayan A, Abdulhalim H, El-Bakry E, et al. Laparoscopic pyelolithotomy: Is the retroperitoneal route a better approach? Int J Urol 2009; 16:181-186.
- Goel A, Hemal AK. Evaluation of role of retroperitoneoscopic pyelolithotomy and its comparison with percutaneous nephrolithotripsy. Int Urol Nephrol 2003; 35:73-76.
- Meria P, Milcent S, Desgrandchamps F, et al. Management of pelvic stones larger than 20 mm: laparoscopic transperitoneal pyelolithotomy or percutaneous nephrolithotomy? Urol Int 2005; 75:322-326.
- Haggag YM, Morsy G, Badr MM, et al. Comparative study of laparoscopic pyelolithotomy versus percutaneous nephrolithotomy in the management of large renal pelvic stones. Canadian Urol Assoc J 2013; 7:171.
- Türk C, Petřík A, Sarica K, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol 2016; 69:475-482. 10.1016/j.eururo.2015.07.041.
- Bai Y, Tang Y, Deng L, et al. Management of large renal stones: laparoscopic pyelolithotomy versus percutaneous nephrolithotomy. BMC Urol 2017; 17:75.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Naveed Khan1*, Mohd Tafazul1, Farah Mushtaq2, Mohamad Ommid2 and Muneer Khan1
1Department of Urology, Kidney Hospital, Sonwar, Srinagar, Jammu and Kashmir, India2Department of Anaesthesia, Kidney Hospital, Sonwar, Srinagar, Jammu and Kashmir, India
Received: 18-Jul-2022, Manuscript No. jrmds-22-69418; , Pre QC No. jrmds-22-69418(PQ); Editor assigned: 20-Jul-2022, Pre QC No. jrmds-22-69418(PQ); Reviewed: 04-Aug-2022, QC No. jrmds-22-69418(Q); Revised: 09-Aug-2022, Manuscript No. jrmds-22-69418(R); Published: 16-Aug-2022
