Review Article - (2022) Volume 10, Issue 12
Knowledge, Attitude and Practice Regarding Telemedicine among Health Professionals Involved in Treating Patient Attending a Rural Tertiary Care Hospital in Central India: A Cross Sectional Study
Abhinav Goyal1 and Mahalaqua Nazli Khatib2*
*Correspondence: Dr. Mahalaqua Nazli Khatib, Department of Physiology, Jawaharlal Nehru Medical College, Datta Meghe Institiute of Medical Sciences (Deemed to be University), Sawangi (Meghe), Wardha, Maharashtra, India, Email:
Abstract
Telemedicine has gained significant traction within the recent years, especially during the COVID-19 pandemic, which had put the patient and the care givers at a distance, due to the quarantine restrictions. Telemedicine has been extensive used for the purpose of teleradiology, telepathology and telepsychiatry throughout the course of the pandemic. However, the knowledge, attitude and practices towards the use of telemedicine in rural Indian areas are still limited. Hence, we designed this study to access the views of healthcare professionals regarding the use of telemedicine in the rural areas of central India.
Keywords
Telemedicine, Rural India, Cross sectional survey, Tertiary care hospital
Introduction
Telemedicine (TM) refers to the usage of Information Communication Technologies (ICT) for the purpose of sharing medical information and providing healthcare in cases where distances hinder the participants to access the health care facility [1]. Hence, TM is also referred to as ‘healing at a distance.’ It can play a pivotal role in improving people live through diverse range of applications in patient care such as healthcare delivery, diagnosis of diseases, follow up and transmission of medical records, disease surveillance, epidemiological studies and health promotion through Behavior Change Communication (BCC). Additionally, it can also help in promotion of research and training of the Health Care Professionals (HCPs), which is a critical component of patient care [2]. However, people residing in remote areas across the globe scuffle to get high quality health care services, which can be affordable and available in short time. These remote populations usually have poor access to quality healthcare, mainly due to the fact that the specialist HCPs are more concentrated in urban area [3]. Telemedicine has the potential to bridge this distance and facilitate healthcare in these remote areas [4].
The use of mobile phones and internet is growing rapidly in the India. Worldwide, a large number of people belonging to rural and remote areas have poor access to timely, good quality and affordable specialist medical care. Inhabitants of such areas often have unsatisfactory healthcare at hands, primarily because majority specialist doctors are more likely to be concentrated in urban areas. The recent advancements in ICTs and the internet have paved the way for the rapidly growing mobile phone market globally as well as in India and have facilitated telemedicine in bringing quality healthcare to these remote areas. Telemedicine has emerged as a viable and practical solution for these wide ranged challenges in delivering healthcare for diseases like diabetes, cancer, coronary heart diseases, anxiety disorder, maternal depression, eating disorders and even substance abuse owing to the high penetration of mobile phones into the general population [5-15].
Despite the ever increasing usage of ICT for innumerable purposes, the precise know how and application of TM for health care services is limited. Additionally, knowledge, attitude and practices regarding usage of TM for accessing healthcare, especially in an Indian rural setup are inconclusive. Hence, we conducted this study to assess knowledge, attitude and practice regarding telemedicine among HCP such as (medical doctors, residents, interns) involved in treating patient attending a rural tertiary care hospital in central India. Results of this study can help in designing and implementing future strategies aimed at improving the utilization of TM practices among HCPs in a rural hospital.
Review of literature
The earliest documented record of using ICTs for healthcare dates back to the 20th century when, for the first time electrocardiogram reports were shared over the telephone line [16]. Since then, several advancements in ICTs have led to a simultaneous increase in the use and acceptance of technologies throughout the health care spectrum. The world-wide connectivity and coverage of the internet has also opened up new possibilities in the healthcare sector. Due to the exquisite utilization of ICTs for specific purposes in different medical specialties, a simple definition for telemedicine cannot suffice. The report on telemedicine published by WHO in 2009, has defined TM as “the delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities” [17]. The commonest form of TM is video conferencing between a remotely located patient and a healthcare provider. Other forms of TM include forward transmission of medical information, Remote Patient Monitoring (RPM) and Mobile Health communication (m- Health).
Numerous studies have also been conducted with an aim to evaluate the utility of telecommunication technologies in effective delivery of healthcare and assess the benefits availed by the integration of data processing technologies like Artificial Intelligence (AI), machine learning, deep learning and internet of things into experimental healthcare models [18-25].
Major advancements in telemedicine practices can be attributed hugely to developments seen in internet, with increasing bandwidth, connectivity and outreach to rural areas, thus enabling the under privileged to gain access to quality medical care from the comfort of their homes. As per WHO’s report on telemedicine in 2012, the highest acceptance and usage of telemedicine technologies were mainly dominated by four main clinical branches. Together with the services provided, these divisions were named as teleradiology, teledermatology, telepathology and telepsychiatry. Out of these teleradiology had the highest global service provisions 33%. The use of biometric devices such as heart rate monitors, blood glucose and blood pressure monitors have helped migrate the center of health care delivery from hospitals to patients’ own homes, particularly in industrialized countries. In developing countries with low income and infrastructure limitations, telemedicine platforms are being used to connect patients with specialists and tertiary care centers and promote health by providing health education.
Globally, various national and international projects have been initiated to reap the benefits of telemedicine and provide healthcare in distant parts of the world. For example, a project started by the mongolian government for telemedicine support to promote maternal and newborn health in remote provinces of mongolia, was undertaken to reduce maternal and infant mortality, while addressing the lack of resources in rural health care services [26]. Detection of pregnancy complications at early stages through TM support consultation significantly reduced of maternal and newborn morbidity and mortality. The Opportune Breast Cancer Screening and Diagnosis Program (OBCSDP) aimed at reducing breast cancer mortality rate in women, was designed to tackle the economic and personnel barriers through unique innovations in ICTs. The tele ECG initiative, being one of the early major telemedicine programmers in Norway, was started in 1995 as a way to reduce time lag between onset acute cardiac illness and its treatment. Text based alerts for HIV testing, use of telemedicine in hypertension control, teleconsultations and online prescriptions are some other examples of the use of telecommunications in healthcare [27-30]. On the other end of the spectrum lies the use of artificial intelligence and deep learning in clinical branches like teleophthalmology for screening and early detection of diseases such as diabetic retinopathy and retinopathy of prematurity, in teleradiology for making early diagnosis of certain cancers using CT and MRI images, for designing epidemiological surveillance models, tracking public health issues and illustrating disease trends [31-34].
In India, ISRO laid down the foundation of telemedicine in 2001, by introducing the first pilot project which connected chittoor’s apollo rural hospital in Andra Pradesh to Chennai’s apollo hospital in Tamil Nadu. Later other agencies like Department of Information Technology (DIT), Ministry of Health and Family Welfare (MOHFW) and the governments of various states have contributed immensely to the early establishment of telemedicine practices in India. The national cancer network, national medical college network, digital medical library network, national rural telemedicine network and integrated disease surveillance project, are some examples of the projects initiated by the ministry of health, to facilitate the use of Telemedicine throughout the country. National telemedicine portal set up by MOHFW is focused on constructing a National Medical College Network (NMCN) for linking together all the medical colleges across the country and provides eeducation in medical field. Along with this, MOHFW had set up the national rural telemedicine network to aid in the delivery of e-healthcare in rural areas. MoHFW has also developed the standards for Electronic Health Records (EHR) in 2016 [35]. All these initiatives have led to an increase in the use of telemedicine in fields like follow up and monitoring of asthma patients, diabetes care, psychiatric care and other areas [36-39].
With the advent of the COVID-19 pandemic and the burdens it had put on the health care sector globally, telemedicine has proved itself in the test of time to be safer, cheaper, easily accessible and affordable. Although these benefits were hugely influenced by the availability of specialists on telemedicine platforms and the ability of patients to access such facilities. Smartphones have indeed played a crucial role in delivery of efficient healthcare and remote monitoring during the country wide lockdown, while the Indian healthcare system was being massively overwhelmed by COVID-19 cases.
It would not be wise to consider that TM can address all the existing issues. However, it can address a range of issues associated with health care. Facilities like telehealth, teleeducation and telehome healthcare are like a boon. International TM programs are bridging the distance gap between a HCP and the patient and distance is now no longer an obstacle in availing quality healthcare. However, TM has not gained the momentum which it should have. Lack of awareness and acceptance of TM by HCPs as well as patients especially the rural populaces are holding it back. The governing bodies all across the globe are now taking an ardent interest in promoting and improving TM services thereby resulting in a gradual but steady improvement in its usage. Expectantly over the ensuing years, improvement in services of TM and its subsequent utilization will reach their real potential.
Aims and objectives
Primary objective: To assess knowledge, attitude and practices regarding utilization of telemedicine among health professionals (Medical doctors, residents and interns) involved in patient care in a tertiary care rural teaching hospital in central India.
Secondary objective: To examine correlations between genders, exposure, seeming interest in future use of TM for better healthcare by health professionals (medical doctors, residents, interns) involved in patient care in a tertiary care rural teaching hospital in central India.
Materials and Methods
Ethical considerations
This web based survey study was started after seeking approval from the institutional ethics committee of the University. IEC approval letter ref. no. IEC/2021/319.
Study population
Health professionals (medical doctors, residents, interns) involved in patient care attending a 1250 bedded rural tertiary care teaching rural hospital in central India. All the health professionals like medical doctors, residents, interns (involved in patients care) affiliated with a rural tertiary care hospital of central India were recruited to participate in this cross sectional research study. For this study, we have used the World Health Organization (WHO) definition of telemedicine as, “The delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities”. We focused on telemedicine as direct verbal communication, direct messaging (e.g. text, email), patient directed web based applications (apps) and patient provider shared web based apps.
Sample size: Sample size was calculated using formula for cross sectional study. Power of test was kept at 80%; confidence interval at 95%. The sample size was calculated as 254 participants.
Duration of study: Two months.
Selection criteria
Inclusion criteria
• Health professionals like medical doctors, residents, interns involved in care of patient attending a rural tertiary care hospital in central India.
• Health professionals willing to participate in the study.
Exclusion criteria
Following people were excluded from the study owing to differences in settings and e-usage practices.
• Private medical practitioners involved in patient care.
• Health professionals not involved in patient care.
• Nurses and technical staff members.
• Health professionals not willing to participate in the study.
Data collection
In view of the COVID-19 pandemic scenario, instead of contacting the participants personally, whatsapp messages were sent to health care professionals (medical doctors, residents, interns) involved in health care of patients till agreement responses of 255 HCPs was achieved. Health professionals (medical doctors, residents, interns) involved in health care of patients were contacted via whatsapp. A message was then sent providing further information about the purpose of research study in detail, along with a link to access online survey. The survey was divided into three parts, with the part one being used to electronically obtain consent to participate in the study. Part two of the survey was used to collect demographic details like age, gender, specialty and designation. Part three of the survey included the questionnaire. Data was collected in one month period and reminder alerts were sent to all participants on whatsapp. Participation in the study was kept entirely voluntary and participants had the choice to withdraw from the study at any time during the survey period. Responses to the questionnaire were collected separately from personal information and were kept strictly confidential.
Instruments used
In this study we used a previously validated questionnaire, as an online survey for assessing knowledge, attitude and practices regarding effective implementation of Telemedicine in rural Indian population (Annexure 1). The questionnaire broadly covered three domains. First domain consisted of ten components to assess the knowledge, attitude and perception regarding utility of Telemedicine for healthcare; wherein the participant had to choose any opinion ranging from “strongly disagree,” to “somewhat disagree,” “no opinion,” “somewhat agree” or “strongly agree.” The second and third domain had ten components each to assess the benefits and barriers respectively and had to be answered as either “yes” or “no.” The average time to complete the questionnaire was approximately 5-8 minutes. The entire survey was conducted on the website zohosurvery.in and tools for processing of data as well tables and graphs were obtained from same website.
Quality control
Quality control was maintained strictly throughout the duration of the study by ensuring the following quality control measures:
• We will try to adhere to the protocol.
• Early involvement of institutional research assistance unit.
• Confidentiality will be strictly maintained.
• To ensure completion of preform, reminders will be sent to all the participants.
Consent and confidentiality
The participants provided their electronic consent to participate in this study before the questionnaire. The confidentiality was strictly maintained.
Statistical analysis
The thematic analysis of qualitative data was done in two steps. Answers were first obtained from the open ended questions and then analyzed for sets of common themes among them. Frequencies of common themes were calculated into percentages. The themes were then examined for trends and distributions against different influencing factors. We used Chi-square test to analyses the statistical significance of differences between the groups. Quantitative data analyses were performed using STATA version 12.0 software.
Results
About 321 whatsapp messages were sent to health care professionals (medical doctors, residents, interns) involved in health care of patients till agreement responses of 286 HCPs was achieved. Out of these responses, 255 participants completed the questionnaire with a response rate of 89%. The participants included 32 doctors (12.5%), 105 resident doctors (41.2%) and 118 (46.2%) medical interns with 136 (53.4%) female and 119 (46.5%) males. The age of the participants ranged between 19 to 36 years with the mean age of the male participants as 23.82 ± 2.78 SD and of the female participants as 23.79 ± 1.43 SD. The doctors and PG students that willingly participated in the study were mostly from medicine and radiology department.
Responses in domain 1 of questionnaire
All the participants in the study completed the online questionnaire. First domain consisted of ten components to assess the knowledge, attitude and perception regarding utility of telemedicine for health care (Figure 1). Majority of the participants somewhat agreed that the implementation of telemedicine will help in easy access to healthcare for rural patients (60.94%), saves travel time and costs (64.06%) as well as helping save patients’ time (73.44%) and expenses (60.94%) and should be implemented in all hospitals with internet facility (60.94%). Almost one third of the participants (34.38%) were neutral but less than one third (29.69%) somewhat agreed that telemedicine will be beneficial only for urban population, more than one third (37.50%) somewhat agreed telemedicine can never replace face to face consultation, while almost half of the participants (43.75%) were neutral to the reliability of telemedicine consultations. Views of the participants on the ability of telemedicine to prevent the worsening of patients’ medical condition, were equally divided between somewhat agree (42.19%) and neutral (42.19%). More than half of the participants (53.13%) somewhat agreed that doctors will approve telemedicine only after its benefits have been statistically evaluated. The data examined for trends and distributions about KAP against gender has been depicted (Table 1). Overall, no significant association was observed in gender as well as level of expertise of HCPs (such as interns, PGs and doctors) regarding knowledge, attitude and practices about TM except about TM in helping the easy access of healthcare services for rural patients (Figure 1).
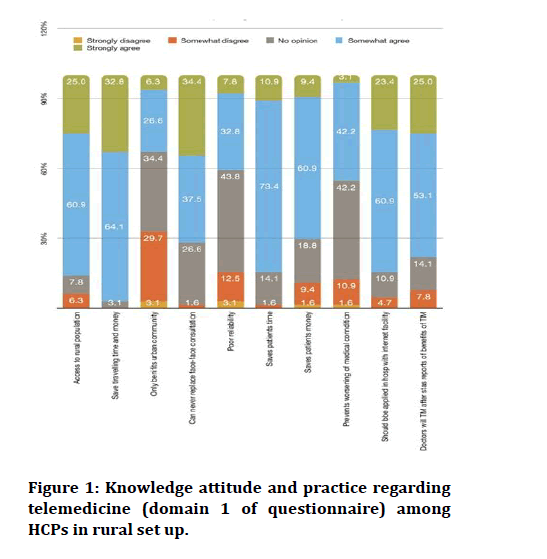
Figure 1: Knowledge attitude and practice regarding telemedicine (domain 1 of questionnaire) among HCPs in rural set up.
| Q. no | Questions in domain 1 of questionnaire | Participants responses | P-value Chi2 value |
||||
|---|---|---|---|---|---|---|---|
| Strongly agree | Somewhat agree | No opinion | Somewhat disagree | Strongly disagree | |||
| Q. 1 | TM will help in easy access of healthcare services for rural patients | Male: 14.29% Female: 33.33% |
Male: 64.29% Female: 58.33% |
Male: 10.71% Female: 5.56% |
Male: 10.71% Female: 2.78% |
Male: 14.29% Female: 33.33% |
P=0.212 Chi2=4.501 |
| Interns: 25.81% PGs: 25.81% Doctors: 0.71% |
Interns: 64.51% PGs: 61.29% Doctors:0.00 |
Interns: 6.45% PGs: 3.23% Doctors:100% |
Interns:6.45% PGs: 6.45% Doctors: 0 |
Interns: 0 PGs: 0 Doctors: 0 |
P=0.00 Chi2=24.59 |
||
| Q. 2 | TM will save travelling time and money for availing expert opinion | Male: 21.43% Female: 41.67% |
Male: 71.43% Female: 58.33% |
Male: 7.14% Female: 0% |
Male: 0% Female: 0% |
Male: 0% Female: 0% |
P=0.084 Chi2=4.959 |
| Interns: 38.71% PGs: 29.71% Doctors: 0 |
Interns: 67.74% PGs: 58.06% Doctors:100% |
Interns: 3.23% PGs: 3.23% Doctors: 0% |
Interns: 0% PGs: 0% Doctors: 0% |
Interns: 0% PGs: 0% Doctors: 0% |
P=0.768 Chi2=1.827 |
||
| Q. 3 | TM will benefit only the urban community | Male: 3.57% Female: 8.33% |
Male: 35.71% Female: 19.44% |
Male: 39.29% Female: 30.56% |
Male: 14.29% Female: 41.67% |
Male: 7.14% Female: 0% |
P=0.06 Chi2=9.039 |
| Interns: 12.9% PGs: 0 Doctors: 0 |
Interns: 25.81% PGs: 29.03% Doctors: 0 |
Interns: 35.48% PGs: 32.26% Doctors:50% |
Interns: 22.58% PGs: 35.48% Doctors:50% |
Interns: 3.23% PGs: 3.23% Doctors: 0 |
P=0.616 Chi2=6.281 |
||
| Q. 4 | TM can never replace face to face consultation | Male: 42.86% Female: 27.78% |
Male: 32.14% Female: 41.67% |
Male: 25% Female: 27.78% |
Male: 0% Female: 2.78% |
Male: 0% Female: 0% |
P=0.523 Chi2=2.246 |
| Interns: 29.03% PGs: 38.71% Doctors: 50% |
Interns: 32.26% PGs: 41.94% Doctors:50% |
Interns: 29.03% PGs: 25.81% Doctors: 0 |
Interns: 0 PGs: 3.23% Doctors: 0 |
Interns: 0 PGs: 0 Doctors: 0 |
P=0.844 Chi2=2.715 |
||
| Q. 5 | Reliability of consultation by TM will be poor | Male: 7.14% Female: 8.33% |
Male: 42.86% Female: 25% |
Male: 39.29% Female: 47.22% |
Male: 10.71% Female: 13.89% |
Male: 0% Female: 5.56% |
P=0.483 Chi2=3.465 |
| Interns: 12.90% PGs: 3.23% Doctors: 0 |
Interns: 25.81% PGs: 38,71% Doctors: 50% |
Interns: 41,94% PGs: 45.16% Doctors: 50% |
Interns: 16.13% PGs: 9.68% Doctors: 0 |
Interns: 3.23% PGs: 3.23% Doctors: 0 |
P=0.867 Chi2=3.885 |
||
| Q. 6 | TM will help to save patients' time | Male: 3.57% Female: 16.67 |
Male: 82.14% Female: 66.67 |
Male: 14.29% Female: 13.89% |
Male: 0% Female: 2.78% |
Male: 0%% Female: 0% |
P=0.288 Chi2=3.762 |
| Interns: 12.90% PGs: 9.68% Doctors: 0 |
Interns: 70.97% PGs: 77.42% Doctors: 50% |
Interns: 12.90% PGs: 12.90% Doctors: 50% |
Interns: 3.23% PGs: 00% Doctors: 00% |
Interns: 00% PGs: 00% Doctors: 0% |
P=0.734 Chi2=3.576 |
||
| Q. 7 | TM will help to save patients' money | Male: 3.57% Female: 13.89% |
Male: 60.71% Female: 61.11% |
Male: 25% Female: 13.89 |
Male: 7.14% Female: 11.11% |
Male: 3.57% Female: 0% |
P=0.357 Chi2=4.376 |
| Interns: 9.68% PGs: 9.68% Doctors: 0 |
Interns: 61.29% PGs: 61.29% Doctors:50% |
Interns: 12.58% PGs: 16.13% Doctors: 0 |
Interns: 12.90% PGs: 3.23% Doctors: 50% |
Interns: 3.23% PGs: 0% Doctors: 0% |
P=0.514 Chi2=7.212 |
||
| Q. 8 | TM prevents from worsening of the medical condition of the patient | Male: 0% Female: 5.56% |
Male: 28.57% Female: 52.78% |
Male: 57.14% Female: 30.56% |
Male: 10.71% Female: 11.11% |
Male: 3.57% Female: 0% |
P=0.104 Chi2=7.670 |
| Interns: 6.45% PGs: 0 Doctors: 0 |
Interns: 58.06% PGs: 29.03% Doctors: 0 |
Interns: 25.81% PGs: 54.84% Doctors:100% |
Interns: 6.45% PGs: 16.13% Doctors: 0 |
Interns: 3.23% PGs: 0 Doctors: 0 |
P=0.097 Chi2=13.446 |
||
| Q. 9 | TM should be applied in all the hospitals equipped with internet facility | Male: 17.86% Female: 27.78% |
Male: 57.14% Female: 63.89% |
Male: 21.43% Female: 2.78% |
Male: 3.57% Female: 5.56% |
Male: 0% Female: 0% |
P=0.116 Chi2=5.920 |
| Interns: 29.03% PGs: 19.35% Doctors: 0 |
Interns: 54.84% PGs: 67.74% Doctors:50% |
Interns: 12.90% PGs: 6.45% Doctors:50% |
Interns: 3.23% PGs: 6.45% Doctors: 0% |
Interns: 0 PGs: 0 Doctors: 0 |
P=0.484 Chi2=5.478 |
||
| Q. 10 | Doctors will approve of telemedicine only after getting the statistical reports of the benefits of TM | Male: 21.43% Female: 27.78% |
Male: 57.14% Female: 50% |
Male: 14.29% Female: 13.89% |
Male: 7.14% Female: 8.33% |
Male: 0% Female: 0% |
P=0.933 Chi2=0.435 |
| Interns: 25.81% PGs: 25.81% Doctors: 0 |
Interns: 51.61% PGs: 54.84% Doctors:50% |
Interns: 19.35% PGs: 9.68% Doctors: 0 |
Interns: 3.23% PGs: 9.68% Doctors:50% |
Interns: 0 PGs: 0 Doctors: 0 |
P=0.285 Chi2=7.401 |
||
Table 1: Knowledge attitude and practices regarding telemedicine (domain 1 of questionnaire) among HCPs in a rural set up with regards to gender and level of expertise of HCPs.
Responses in domain 2 of questionnaire
The second domain had ten components to assess the benefits and had to be answered as either “yes” or “no.” Figure 2 clearly outlines that the benefits of telemedicine that can be availed even at rural centers, although there are some limitations. Most of the participants acknowledge the use of telemedicine as helpful in obtaining laboratory results via internet (96.88%), helping in transmission of medical data like x-rays (96.88%), providing health education (96.88%), video consultations between healthcare professionals (95.31%), getting second opinions (95.31%), making outpatients appointments online (93.75%) and referring patients to tertiary care centers (90.63%). However, a lesser percentage agreed that telemedicine is useful in rural areas for monitoring and follow-ups of patient at home (84.38%), teleconferencing via telephone (76.56%) and for pre-operative services (67.19%). The data examined for trends and distributions about benefits of telemedicine as perceived by HCPs against gender and level of expertise of HCPs has been depicted (Table 2). Overall, no significant association was observed in gender as well as level of expertise (HCPs such as interns, PGs and doctors) regarding benefits of TM in health care.
| Q. no | Questions in domain 2 of questionnaire | Responses | P-value Chi2 value |
|
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Q. 11 | Obtaining laboratory results via internet | Male: 100 Female: 94.44 |
Male: 0 Female: 5.56 |
P=0.205 Chi2=1.605 |
| Interns: 100 PGs: 93.55 Doctors:100 |
Interns: 0 PGs: 6.45 Doctors: 0 |
P=0.333 Chi2=2.197 |
||
| Q. 12 | Making outpatient appointments using internet | Male: 89.29 Female: 97.22 |
Male: 10.71 Female: 2.78 |
P=0.193 Chi2=1.693 |
| Interns: 93.55 PGs: 93.55 Doctors:100 |
Interns: 6.45 PGs: 6.45 Doctors: 0 |
P=0.933 Chi2=0.137 |
||
| Q. 13 | Transmission of electrocardiograms, x-rays, still images | Male: 100 Female: 94.44 |
Male: 0 Female: 5.56 |
P=0.205 Chi2=1.605 |
| Interns: 96.77 PGs: 96.77 Doctors: 100 |
Interns: 3.23 PGs: 3.23 Doctors: 0 |
P=0.967 Chi2=0.066 |
||
| Q. 14 | Teleconferencing with patients by telephone | Male: 67.86 Female: 83.33 |
Male: 32.14 Female: 16.67 |
P=0.147 Chi2=2.102 |
| Interns: 83.87 PGs: 70.97 Doctors:50 |
Interns: 16.13 PGs: 29.03 Doctors:50 |
P=0.325 Chi2=2.249 |
||
| Q. 15 | Videoconferencing of a consultation between health care professionals | Male: 92.86 Female: 97.22 |
Male: 7.14 Female: 2.78 |
P=0.412 Chi2=0.671 |
| Interns: 93.55 PGs: 97.66 Doctors:100 |
Interns: 6.45 PGs: 3.23 Doctors: 0 |
P=0.794 Chi2=0.462 |
||
| Q. 16 | Videoconferencing a meeting for health education | Male: 96.43 Female: 97.22 |
Male: 3.57 Female: 2.78 |
P=0.856 Chi2=0.032 |
| Interns: 96.77 PGs: 96.77 Doctors:100 |
Interns: 3.23 PGs: 3.23 Doctors: 0 |
P=0.967 Chi2=0.0666 |
||
| Q. 17 | Monitoring patient at home (follow up) | Male: 85.71 Female: 83.33 |
Male: 14.29 Female: 16.67 |
P=0.795 Chi2=0.0670 |
| Interns: 87.10 PGs: 80.65 Doctors: 0 |
Interns: 19.35 PGs: 12.90 Doctors: 0 |
P=0.647 Chi2=0.871 |
||
| Q. 18 | Preoperative services | Male: 64.29 Female: 69.44 |
Male: 35.71 Female: 30.56 |
P=0.663 Chi2=0.190 |
| Interns: 74.19 PGs: 58.06 Doctors:100 |
Interns: 25.81 PGs: 41.94 Doctors: 0 |
P=0.242 Chi2=2.837 |
||
| Q. 19 | Obtaining second opinion | Male: 92.86 Female: 97.22 |
Male: 7.14 Female: 2.78 |
P=0.412 Chi2=0.671 |
| Interns: 96.77 PGs: 93.55 Doctors:100 |
Interns: 3.23 PGs: 6.45 Doctors: 0 |
P=0.794 Chi2=0.462 |
||
| Q. 20 | Referrals of patients to tertiary Care Centers | Male: 89.29 Female: 91.67 |
Male:10.71 Female: 8.33 |
P=0.746 Chi2=0.105 |
| Interns: 93.55 PGs: 87.10 Doctors: 100 |
Interns: 6.45 PGs: 12.97 Doctors: 0 |
P=0.615 Chi2=0.973 |
||
Table 2: Responses regarding benefits of telemedicine (domain 2 of questionnaire) among HCPs in a rural set up with regards to gender and level of expertise of HCPs.
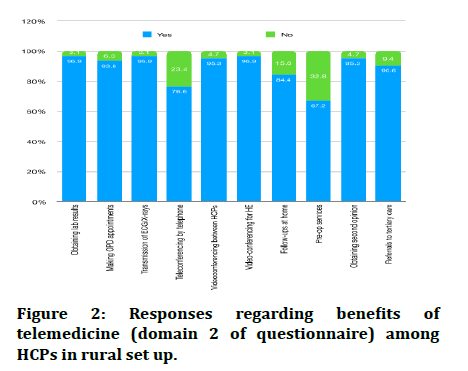
Figure 2: Responses regarding benefits of telemedicine (domain 2 of questionnaire) among HCPs in rural set up.
Responses in domain 3 of questionnaire
The third domain had ten components to assess the barriers and had to be answered as either “yes” or “no” (Figure 2). It delineates the participants’ opinion on barriers faced in implementation of telemedicine in rural areas. Majority candidates asserted that the biggest hurdle in telemedicine practice in rural areas is the legal responsibility (88.14%) that entails its use, followed by the loss of effective communication between the doctors and patients due to distance (86.44%) and the lack of suitable training for equipment use (83.05%). More than three fourth of the participants considered the lack of consultation between IT experts and doctors (79.66%), lack of perceived clinical usefulness (76.27%), lack of user friendly software (72.88%), negative attitude of staff (72.88%) and concerns regarding patients’ privacy (71.19%) as other potential obstacles in the success of telemedicine in rural areas. Only two third of the participants viewed perceived increase in workload (66.10%) while using telemedicine as a barrier. Around half of the responses concluded that the high cost of equipment (59.32%) is yet a barrier in developing successful telemedicine models for rural India. The data examined for trends and distributions about barriers to effective use of telemedicine as perceived by HCPs against gender and level of expertise of HCPs has been depicted (Table 3). Overall, no significant association was observed in gender as well as level of expertise (HCPs such as interns, PGs and doctors) regarding barriers in using of TM in health care (Figure 3).
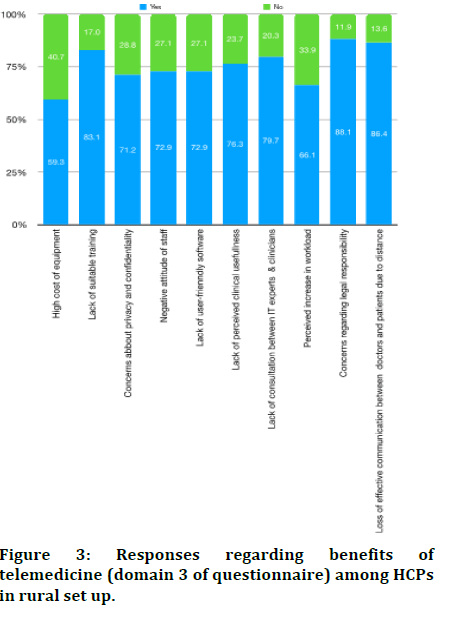
Figure 3: Responses regarding benefits of telemedicine (domain 3 of questionnaire) among HCPs in rural set up.
| Q. no | Questions in domain 3 of questionnaire | Responses to questions | P-value Chi2 value |
|
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Q. 21 | High cost of equipment | Male: 53.85 Female: 63.64 |
Male: 46.15 Female: 36.36 |
P=0.447 Chi2=0.577 |
| Interns: 53.57 PGs: 68.97 Doctors: 0 |
Interns: 46.43 PGs: 31.03 Doctors: 100 |
P=0.110 Chi2=4.418 |
||
| Q. 22 | Lack of suitable training in the use of equipment | Male: 80.77 Female: 84.85 |
Male: 19.23 Female: 15.15 |
P=0.678 Chi2=0.171 |
| Interns: 78.57 PGs: 86.21 Doctors:100 |
Interns: 21.43 PGs: 13.79 Doctors: 0 |
P=0.603 Chi2=1.012 |
||
| Q. 23 | Concerns about patient privacy and confidentiality | Male: 69.23 Female: 72.73 |
Male: 30.77 Female: 27.27 |
P=0.768 Chi2=0.086 |
| Interns: 67.86 PGs: 72.41 Doctors: 100 |
Interns: 32.14 PGs: 27.59 Doctors: 0 |
P=0.612 Chi2=0.982 |
||
| Q. 24 | Negative attitude of staff involved | Male: 69.23 Female: 75.76 |
Male: 30.77 Female: 24.24 |
P=0.576 Chi2=0.313 |
| Interns: 78.57 PGs: 72.41 Doctors: 0 |
Interns: 21.43 PGs: 27.59 Doctors:100 |
P=0.054 Chi2=5.836 |
||
| Q. 25 | Lack of user friendly software | Male: 69.23 Female: 75.76 |
Male: 30.77 Female: 24.24 |
P=0.576 Chi2=0.313 |
| Interns: 78.57 PGs: 68.97 Doctors:50 |
Interns: 21.43 PGs: 31.03 Doctors:50 |
P=0.545 Chi2=1.213 |
||
| Q. 26 | Lack of perceived clinical usefulness | Male: 73.08 Female:78.79 |
Male: 26.92 Female: 21.21 |
P=0.609 Chi2=0.262 |
| Interns: 75 PGs: 79.31 Doctors:50 |
Interns: 25 PGs: 20.69 Doctors:50 |
P=0.626 Chi2=0.935 |
||
| Q. 27 | Lack of consultation between information technology experts and clinicians | Male: 80.77 Female: 78.79 |
Male: 19.23 Female: 21.21 |
P=0.851 Chi2=0.035 |
| Interns: 82.14 PGs: 79.31 Doctors:50 |
Interns: 17.86 PGs: 20.69 Doctors: 50 |
P=0.550 Chi2=1.194 |
||
| Q. 28 | Perceived increase in workload | Male: 69.23 Female: 63.64 |
Male: 30.77 Female: 36.36 |
P=0.652 Chi2=0.2031 |
| Interns: 67.86 PGs: 68.97 Doctors: 0 |
Interns: 32.14 PGs: 31.03 Doctors: 100 |
P=0.132 Chi2=4.044 |
||
| Q. 29 | Concerns regarding legal responsibility | Male: 84.62 Female: 90.91 |
Male: 15.38 Female: 9.09 |
P=0.458 Chi2=0.551 |
| Interns: 92.86 PGs: 82.76 Doctors: 100 |
Interns: 7.14 PGs: 17.24 Doctors: 0 |
P=0.434 Chi2=1.668 |
||
| Q. 30 | Concerns regarding loss of effective communication between the doctors and patients due to distance between the two | Male: 88.46 Female: 84.85 |
Male: 11.54 Female: 15.15 |
P=0.687 Chi2=0.162 |
| Interns: 89.29 PGs: 86.21 Doctors: 50 |
Interns: 10.71 PGs: 13.79 Doctors: 50 |
P=0.292 Chi2=2.46 |
||
Table 3: Responses regarding barriers to the use of telemedicine (domain 3 of questionnaire) among HCPs in a rural set up with regards to gender and level of expertise of HCPs.
Discussion
This study assessed the knowledge, attitude and practices regarding utilization of TM among HCPs (medical doctors, residents, interns) involved in patient care in a tertiary care rural teaching hospital in central India and observed that though the HCPs perceived that telemedicine has a lot of utilities and benefits but also several barriers that limits its use in resource poor settings.
Telemedicine being a relatively new intervention methodology needs tremendous amounts of research and statistical analysis to be effectively applied in resource poor settings. Success of any implementation model largely depends on the input costs, electronic infrastructure, patient awareness and quality of service. Global and national initiatives along with appropriate execution models can enormously escalate the standards of healthcare in low income population using telemedicine. Recent technological advances in the development of telemedicine in developing countries seem promising. The declining costs of electronic gadgets, increasing computing speeds, high speed internet band width, the falling costs of digital storage and storage options, all have cumulatively driven telemedicine to its widespread use today. Cost effectiveness studies have showed that TM can cut the cost, but not all. Lack of randomized control trials and paucity of quality data limit the economic evaluations of TM.
Telemedicine helps rural health centers to provide quality health services at lower costs, which helps rural patients by reducing cost travel to access specialty health care services.
Infrastructure plays a crucial role in realizing the true potentials of any healthcare service. Telemedicine heavily relies on the ICT infrastructure available in different regions and the level of communicability between them. Unfortunately, in most developing countries infrastructure is not adequate enough to utilize most recent technologies. Coupled with this is the limited penetration of computers or other electronic devices into the remote locations, significantly impacting the adoption of TM in such areas. In India, the problem of unstable electric power supply, lack of high speed internet connectivity beyond metropolitan cities and tropical climate are other unfavorable factors which impose further limitations in designing efficient telemedicine models for rural India. Internet congestion can cause a delay in receipt of images or poor resolution of images that may hinder diagnosis and treatment thereof. Slow bandwidth can restrict effective video conference. At places where basic infrastructure exists, there is a lack of inter-operability standards for software and equipment or possibility of computer system failure [40].
Due to the impact of COVID-19 pandemic, there has been an unprecedented increase in the use of TM in almost all of the medical specialties [41,42]. Telehealth rose as a fore most mode of delivering health care services during the COVID-19 pandemic, when patients as well as healthcare providers tried to decrease person to person contact through routine visits. To increase an access to TM and augment flexibility of HCPs, laws, compensation strategies and protocols were momentarily altered through emergency regulations. There are chances that these regulations might become permanent. Assessment of the knowledge and usage of TM will aid in drafting appropriate policy sanctions for enhancing effective and efficient TM use in a rural setup.
The study has several strengths as well as limitations. This study adds to the limited and inconclusive evidence base on knowledge, attitude and practices regarding usage of TM for accessing healthcare, especially in an Indian rural setup. The participants comprised doctors, PG students as well as interns. However; due to time restrictions, wide variety of HCPs such as nurses, private practitioners, dentists, physiotherapists, etc. were not included. This study can be replicated on a larger scale with variety of HCPs involved in providing health care to the patients.
Further investigation of the knowledge, ease of access and cost of utilization of TM would help to deliver tailor made policy recommendations for Indian requirements thus enhancing effective and efficient use of TM in rural health care setup. Quality randomized controlled trials with adequate sample sizes are required to address the knowledge gap regarding use of TM in rural setups.
Conclusion
This study assessed the knowledge, attitude and practices regarding utilization of TM among HCPs (Medical doctors, residents, interns) involved in patient care in a tertiary care rural teaching hospital in central India and observed that though the HCPs perceived that TM has a lot of utilities and benefits, it has several barriers that limits its use in resource poor settings.
TM can help in providing better health care services to the patients residing in rural areas However, proper access to these patients needs to be ensured. Results of this study can help in designing and implementing future strategies aimed at improving the utilization of TM practices among HCPs in a rural hospital.
Summary
Telemedicine (TM) is referred to as ‘healing at a distance’. It can play a pivotal role in improving people live through healthcare delivery, diagnosis of diseases; follow up, transmission of medical data research and training of the Health Care Professionals (HCPs). However, people residing in remote areas all across the globe usually have poor access to quality healthcare and TM has the potential to bridge this distance and facilitate healthcare in these remote areas. Despite the ever increasing usage of ICT for innumerable purposes, the precise know how and application of TM for health care services is limited. Hence, we conducted this study to assess Knowledge, attitude and practice regarding TM among HCPs in treating patient attending a rural tertiary care hospital in central India.
This cross sectional study was started after seeking approval from the IEC. Health professionals (Medical doctors, residents, interns) involved in patient care participated in study. The participants were contacted via whatsapp. They were informed about the nature and purpose of research study and were requested to fill the online questionnaire. The entire survey was conducted on the website zohosurvery.in. The questionnaire broadly covered three domains, each with 10 questions. First domain consisted of ten components to assess the knowledge, attitude and perception regarding utility of Telemedicine for healthcare. The second and third domain had ten components each to assess the benefits and barriers respectively. Answers were analyzed for sets of common themes among them. Frequencies of common themes were calculated into percentages. The themes were then examined for trends and distributions against different influencing factors.
A total of 255 HCPs comprising of 32 doctors (12.5%), 105 residents (41.2%) and 118 (46.2%) medical interns with 136 (53.4%) female and 119 (46.5%) males. The age of the participants ranged between 19 to 36 years. It was observed that though the HCPs perceived that telemedicine has a lot of utilities and benefits, it has several barriers that limits its use inn resource poor settings.
Telemedicine being a relatively new intervention methodology needs tremendous amounts of research and statistical analysis to be effectively applied in resource poor settings. Success of any implementation model largely depends on the input costs, electronic infrastructure, patient awareness and quality of service. Due to the impact of COVID-19 pandemic, there has been an unprecedented increase in the use of TM in almost all of the medical specialties. Telehealth rose as a fore most mode of delivering health care services during the COVID-19 pandemic, when patients as well as health care providers tried to decrease person to person contact through routine visits. Further investigation of the knowledge, ease of access and cost of utilization of TM would help to delivery policy tailor made recommendations for Indian requirements for enhancing effective and efficient use of TM in rural health care set up.
The study found that though the HCPs perceived that TM has a lot of utilities and benefits, it has several barriers that limits its use in resource-poor settings.
References
- Dasgupta A, Deb S. Telemedicine: A new horizon in public health in India. Indian J Community Med Off Publ Indian Assoc Prev Soc Med 2008; 33:3–8.
- Katzmarzyk PT, Mason C. The physical activity transition. J Phys Act Health 2009;; 6:269–280.
- Lucas H. Information and communications technology for future health systems in developing countries. Soc Sci Med 2008; 66:2122–2132.
- World Health Organisation (WHO). Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth. Global Observatory for eHealth Series 2009; 2.
- Nemecek R, Huber P, Schur S, et al. Telemedically augment palliative care. Wien Klin Wochenschr 2019; 131:620–626.
- Pfaeffli Dale L, Whittaker R, Jiang Y, et al. Text message and internet support for coronary heart disease self-management: Results from the Text 4 Heart randomized controlled trial. J Med Internet Res 2015; 17:e237.
- Thabrew H, Stasiak K, Hetrick SE, et al. E-health interventions for anxiety and depression in children and adolescents with long-term physical conditions. Cochrane Database Syst Rev 2018; 8:CD012489.
- Nair U, Armfield NR, Chatfield MD, et al. The effectiveness of telemedicine interventions to address maternal depression: A systematic review and meta-analysis. J Telemed Telecare 2018; 24:639–650.
- Sproch LE, Anderson KP. Clinician delivered teletherapy for eating disorders. Psychiatr Clin North Am 2019; 42:243–252.
- Anderson KE, Byrne CE, Crosby RD, et al. Utilizing telehealth to deliver family based treatment for adolescent anorexia nervosa. Int J Eat Disord 2017; 50:1235–1238.
- Prior AL, Woodward D, Hoefkens T, et al. Telephone helplines as a source of support for eating disorders: Service user, career and health professional perspectives. Eat Disord 2018; 26:164-184.
- Huskamp HA, Busch AB, Souza J, et al. How is telemedicine being used in opioid and other substance use disorder treatment? Health Aff Proj Hope 2018; 37:1940–1947.
- Barash D. Telemedicine in substance use disorder treatment. Health Aff 2019; 38:331.
- Lin LA, Casteel D, Shigekawa E, et al. Telemedicine delivered treatment interventions for substance use disorders: A systematic review. J Subst Abuse Treat 2019; 101:38–49.
- Molfenter T, Brown R, O’Neill A, et al. Use of telemedicine in addiction treatment: Current practices and organizational implementation characteristics. Int J Telemed Appl 2018; 2018:3932643.
[Crossref] [Googlescholar] [Indexed]
- Chellaiyan VG, Nirupama AY, Taneja N. Telemedicine in India: Where do we stand? J Fam Med Prim Care 2019; 8:1872–1876.
- World Health Organization (WHO). Telemedicine: Opportunities and developments in member states: Report on the second global survey on e-Health. Geneva, Switzerland, 2009.
- Bohr A, Memarzadeh K. The rise of artificial intelligence in healthcare applications. Elsevier 2020; 25–60.
- Hamet P, Tremblay J. Artificial intelligence in medicine. Metabolism 2017; 69:S36–S40.
- Handelman GS, Kok HK, Chandra RV, et al. eDoctor: Machine learning and the future of medicine. J Intern Med 2018; 284:603–619.
- Deo RC. Machine learning in medicine. Circulation 2015; 132:1920–1930. [Crossref]
[Googlescholar] [Indexed]
- Chan HP, Samala RK, Hadjiiski LM, et al. Deep learning in medical image analysis. Adv Exp Med Biol 2020; 1213:3–21.
- Bizopoulos P, Koutsouris D. Deep learning in cardiology. IEEE Rev Biomed Eng 2019; 12:168–193.
[Crossref] [Googlescholar] [Indexed]
- Singh RP, Javaid M, Haleem A, et al. Internet of things (IOT) applications to fight against COVID-19 pandemic. Diabetes Metab Syndr 2020; 14:521–524.
[Crossref] [Googlescholar] [Indexed]
- Kelly JT, Campbell KL, Gong E, et al. The internet of things: Impact and implications for health care delivery. J Med Internet Res 2020; 22:e20135.
- Baatar T, Suldsuren N, Bayanbileg S, et al. Telemedicine support of maternal and newborn health to remote provinces of Mongolia. Stud Health Technol Inform 2012; 182:27–35. [Crossref]
[Googlescholar] [Indexed]
- Portillo B, Garcia-Cervigon P, Figueras P, et al. Telemedicine, prison and illness associated with HIV. Rev Espanola Quimioter Publicacion of Soc Espanola Quimioter 2019; 32:539–544. [Crossref]
[Googlescholar] [Indexed]
- Omboni S, Caserini M, Coronetti C. Telemedicine and M-health in hypertension management: Technologies, applications and clinical evidence. High Blood Press Cardiovasc Prev Off J Ital Soc Hypertens 2016; 23:187–196.
[Crossref] [Googlescholar] [Indexed]
- Augusterfer EF, O’Neal CR, Martin SW, et al. The role of telemental health, teleconsultation and telesupervision in post disaster and low resource settings. Curr Psychiatry Rep 2020; 22:85.
[Crossref] [Googlescholar] [Indexed]
- Le T, Toscani M, Colaizzi J. Telepharmacy: A new paradigm for our profession. JPharm Pract 2020; 33:176–182.
- Fatehi F, Jahedi F, Kanagasingam Y, et al. Teleophthalmology for the elderly population: A review of the literature. Int J Med Inf 2020; 136:104089.
- Grisolia ABD, Abalem MF, Lu Y, et al. Teleophthalmology: Where are we now? Arq Bras Oftalmol 2017; 80:401–406.
- Hanna TN, Steenburg SD, Rosenkrantz AB, et al. Emerging challenges and opportunities in the evolution of teleradiology. AJR Am J Roentgenol 2020; 215:1411–1416.
- Bradley WG. Teleradiology. Neuroimaging Clin N Am 2012; 22:511–517.
- Ministry of Health and Family Welfare (MOHFW). Electronic Health Records (EHR) standards for India. Department of Health and Family Welfare. 2016.
- Jain S, Thakur C, Kumar P, et al. Telemedicine for asthma follow up in children during COVID-19 pandemic. Indian J Pediatr 2021; 88:1050.
[Crossref] [Googlescholar] [Indexed]
- Ghosh A, Gupta R, Misra A. Telemedicine for diabetes care in India during COVID-19 pandemic and national lockdown period: Guidelines for physicians. Diabetes Metab Syndr 2020; 14:273–276.
[Crossref] [Googlescholar] [Indexed]
- Ramalho R, Adiukwu F, Gashi Bytyci D, et al. Tele-psychiatry and healthcare access inequities during the COVID-19 pandemic. Asian J Psychiatry 2020; 53:102234.
- Ateriya N, Saraf A, Meshram VP, et al. Telemedicine and virtual consultation: The Indian perspective. Natl Med J India 2018; 31:215–218.
[Crossref] [Googlescholar] [Indexed]
- Combi C, Pozzani G, Pozzi G. Telemedicine for developing countries. Appl Clin Inform 2016; 7:1025–1050.
[Crossref] [Googlescholar] [Indexed]
- Lukas H, Xu C, Yu Y, et al. Emerging telemedicine tools for remote COVID-19 diagnosing, monitoring and management. ACS Nano 2020; 14:16180–16193.
[Crossref] [Googlescholar] [Indexed]
- Colbert GB, Venegas Vera AV, et al. Utility of telemedicine in the COVID-19 era. Rev Cardiovasc Med 2020; 21:583–587.
[Crossref] [Googlescholar] [Indexed]
Author Info
Abhinav Goyal1 and Mahalaqua Nazli Khatib2*
1Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institiute of Medical Sciences (Deemed to be University), Sawangi (Meghe), Wardha, Maharashtra, India2Department of Physiology, Jawaharlal Nehru Medical College, Datta Meghe Institiute of Medical Sciences (Deemed to be University), Sawangi (Meghe), Wardha, Maharashtra, India
Citation: Abhinav Goyal, Mahalaqua Nazli Khatib, Knowledge, Attitude and Practice Regarding Telemedicine among Health Professionals Involved in Treating Patient Attending a Rural Tertiary Care Hospital in Central India: A Cross Sectional Study, J Res Med Dent Sci, 2022, 10 (12): 247-258.
Received: 07-Oct-2022, Manuscript No. JRMDS-22-77327 ; , Pre QC No. JRMDS-22-77327(PQ) ; Editor assigned: 11-Oct-2022, Pre QC No. JRMDS-22-77327(PQ) ; Reviewed: 25-Oct-2022, QC No. JRMDS-22-77327 ; Revised: 08-Dec-2022, Manuscript No. JRMDS-22-77327(R) ; Published: 15-Dec-2022
